Some women’s breasts can’t make enough milk, and the effects can be devastating
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many new mothers worry about their milk supply. For some, support from a breastfeeding counsellor or lactation consultant helps.
Others cannot make enough milk no matter how hard they try. These are women whose breasts are not physically capable of producing enough milk.
Our recently published research gives us clues about breast features that might make it difficult for some women to produce enough milk. Another of our studies shows the devastating consequences for women who dream of breastfeeding but find they cannot.
Some breasts just don’t develop
Unlike other organs, breasts are not fully developed at birth. There are key developmental stages as an embryo, then again during puberty and pregnancy.
At birth, the breast consists of a simple network of ducts. Usually during puberty, the glandular (milk-making) tissue part of the breast begins to develop and the ductal network expands. Then typically, further growth of the ductal network and glandular tissue during pregnancy prepares the breast for lactation.
But our online survey of women who report low milk supply gives us clues to anomalies in how some women’s breasts develop.
We’re not talking about women with small breasts, but women whose glandular tissue (shown in this diagram as “lobules”) is underdeveloped and have a condition called breast hypoplasia.
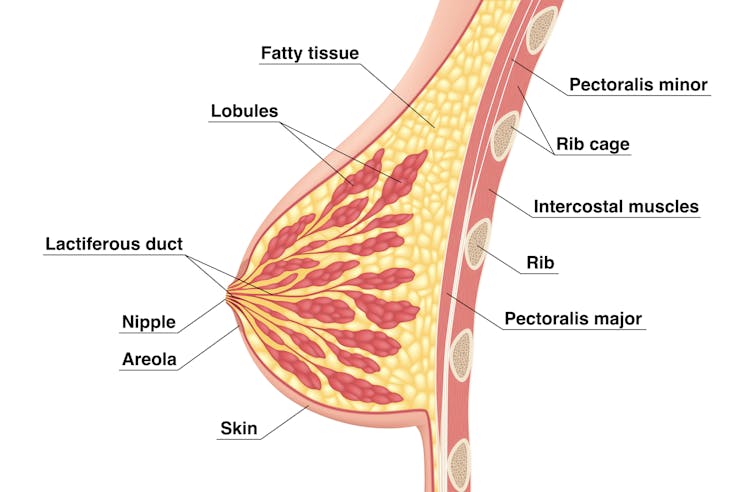
Tsuyna/Shutterstock
We don’t know how common this is. But it has been linked with lower rates of exclusive breastfeeding.
We also don’t know what causes it, with much of the research conducted in animals and not humans.
However, certain health conditions have been associated with it, including polycystic ovary syndrome and other endocrine (hormonal) conditions. A high body-mass index around the time of puberty may be another indicator.
Could I have breast hypoplasia?
Our survey and other research give clues about who may have breast hypoplasia.
But it’s important to note these characteristics are indicators and do not mean women exhibiting them will definitely be unable to exclusively breastfeed.
Indicators include:
- a wider than usual gap between the breasts
- tubular-shaped (rather than round) breasts
- asymmetric breasts (where the breasts are different sizes or shapes)
- lack of breast growth in pregnancy
- a delay in or absence of breast fullness in the days after giving birth
In our survey, 72% of women with low milk supply had breasts that did not change appearance during pregnancy, and about 70% reported at least one irregular-shaped breast.
The effects
Mothers with low milk supply – whether or not they have breast hyoplasia or some other condition that limits their ability to produce enough milk – report a range of emotions.
Research, including our own, shows this ranges from frustration, confusion and surprise to intense or profound feelings of failure, guilt, grief and despair.
Some mothers describe “breastfeeding grief” – a prolonged sense of loss or failure, due to being unable to connect with and nourish their baby through breastfeeding in the way they had hoped.
These feelings of failure, guilt, grief and despair can trigger symptoms of anxiety and depression for some women.

Bricolage/Shutterstock
One woman told us:
[I became] so angry and upset with my body for not being able to produce enough milk.
Many women’s emotions intensified when they discovered that despite all their hard work, they were still unable to breastfeed their babies as planned. A few women described reaching their “breaking point”, and their experience felt “like death”, “the worst day of [my] life” or “hell”.
One participant told us:
I finally learned that ‘all women make enough milk’ was a lie. No amount of education or determination would make my breasts work. I felt deceived and let down by all my medical providers. How dare they have no answers for me when I desperately just wanted to feed my child naturally.
Others told us how they learned to accept their situation. Some women said they were relieved their infant was “finally satisfied” when they began supplementing with formula. One resolved to:
prioritise time with [my] baby over pumping for such little amounts.
Where to go for help
If you are struggling with low milk supply, it can help to see a lactation consultant for support and to determine the possible cause.
This will involve helping you try different strategies, such as optimising positioning and attachment during breastfeeding, or breastfeeding/expressing more frequently. You may need to consider taking a medication, such as domperidone, to see if your supply increases.
If these strategies do not help, there may be an underlying reason why you can’t make enough milk, such as insufficient glandular tissue (a confirmed inability to make a full supply due to breast hypoplasia).
Even if you have breast hypoplasia, you can still breastfeed by giving your baby extra milk (donor milk or formula) via a bottle or using a supplementer (which involves delivering milk at the breast via a tube linked to a bottle).
More resources
The following websites offer further information and support:
- Australian Breastfeeding Association
- Lactation Consultants of Australia and New Zealand
- Royal Women’s Hospital, Melbourne
- Supply Line Breastfeeders Support Group of Australia Facebook support group
- IGT And Low Milk Supply Support Group Facebook support group
- Breastfeeding Medicine Network Australia/New Zealand
- Supporting breastfeeding grief (a collection of resources).
Shannon Bennetts, a research fellow at La Trobe University, contributed to this article.
Renee Kam, PhD candidate and research officer, La Trobe University and Lisa Amir, Professor in Breastfeeding Research, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Use Topical Estrogen Cream For Aging Skin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Sam Ellis, dermatologist, explains:
Tackling the cause
Estrogen is important for very many aspects of health beyond the sexual aspects. When it comes to skin, a drop in estrogen (usually because of menopause) leads to changes like collagen loss, dryness, reduced elasticity, and slower wound healing. Applying estrogen creams to the skin can reverse these changes.
If your estrogen levels are already within normal pre-menopausal female ranges, by the way, there isn’t so much science to indicate its benefit when used topically. If you are already on systemic HRT (i.e., you take estrogen already to raise your blood estrogen levels and affect your body in its entirety), you may or may not gain extra benefits from the topical cream, depending on factors such as your estrogen dose, your route of administration, your cardiovascular health, and other factors.
For those with lower estrogen and not currently on HRT, you may be wondering: can topical estrogen cream affect systemic estrogen levels? And the answer is that it mostly depends on the dose. In other words: it’s definitely possible, but for most people it’s unlikely.
As ever, if thinking of taking up any hormonal treatment, do consult an endocrinologist and/or gynecologist, and if you have an increased breast cancer risk (for example genetically or prior history), then an oncologist too, just to be safe.
That sounds like a lot of scary things, but mostly it’s just to be on the safe side. The dose of estrogen is very low in topical creams, and even then, only a tiny amount is used per day.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- “Why Does It Hurt When I Have Sex?” (And What To Do About It) ← because topical estrogen is not just for your face! Yes, you can use it down there too and it’s commonly prescribed for exactly this use.
- Hormones & Health, Beyond The Obvious
- The Hormone Therapy That Reduces Breast Cancer Risk & More
Take care!
Share This Post
-
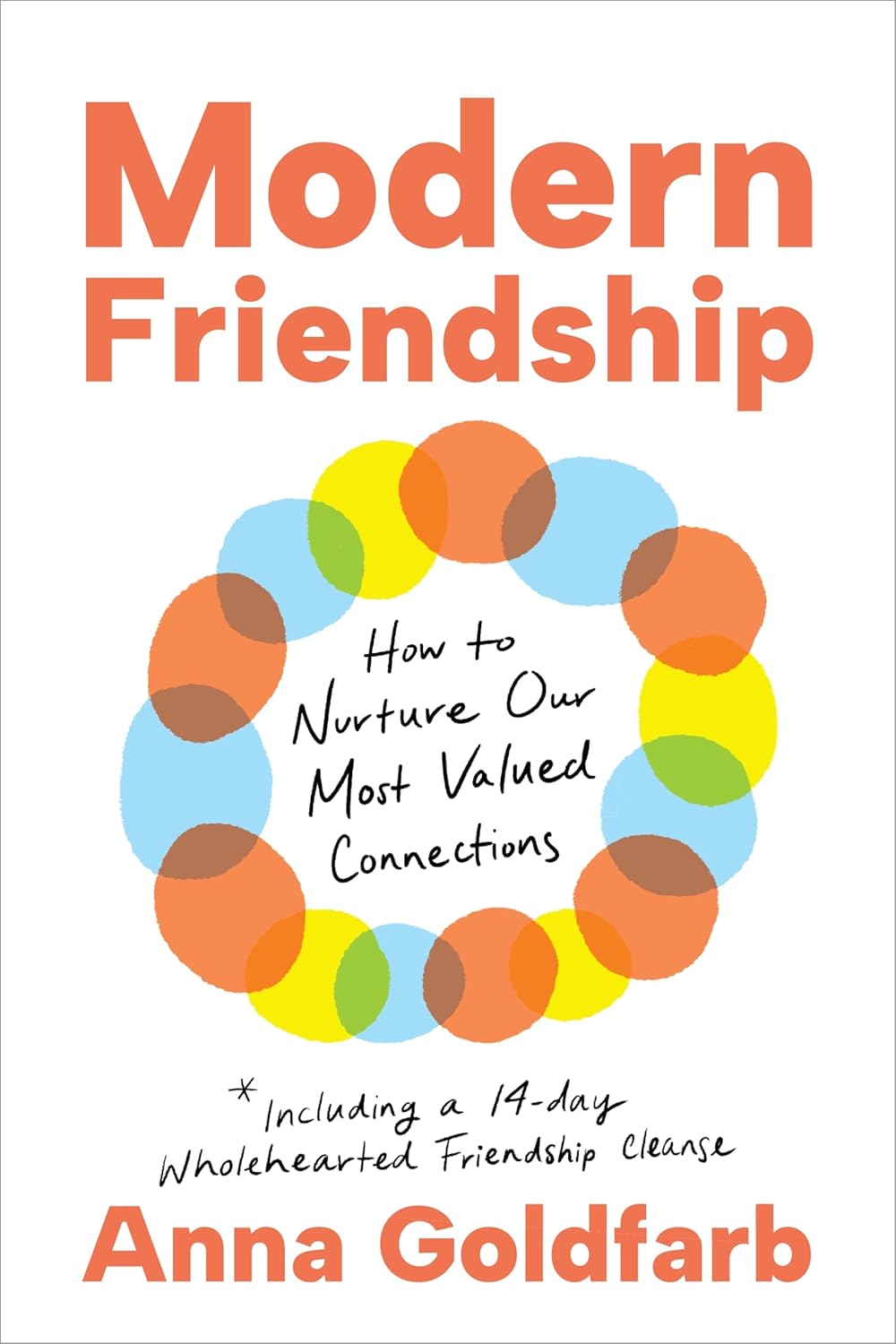
Modern Friendship – by Anna Goldfarb
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a topic we’ve covered before at 10almonds: Human Connection In An All-Too-Busy World.
Here, however, Goldfarb has an entire book to cover what we had one article to cover, so of course it’s a lot more in-depth.
Importantly, if also covers: what if you seem to be doing everything right, and it’s still not working out? What if you’re already reaching out, suggesting things, doing your part?
Piece by piece, she uncovers what the very many problems are, ranging from availability issues and priorities, to health concerns and financial difficulties, to challenges as diverse as trust issues and exhaustion, and much more.
After all the hard truths about modern friendship, she gets onto equally cheery topics such as why friendships fail, but fear not, solutions are forthcoming too—and indeed, that’s what most of the book is about.
Covering such topics as desire, diligence, and delight, we learn how to not only practise wholehearted friendship, but also, how to matter to others, too. She finishes up with a “14-day friendship cleanse”, which sounds a lot more alarming than it actually is.
The style is interesting, being personal and, well, friendly throughout—but still with scholarly citations as we go along, and actual social science rather than mere conjecture.
Bottom line: if you find that your friendships are facing challenges, this book can help you to get to the bottom of any problems and move forwards (likely doing so together).
Click here to check out Modern Friendship, and learn how to truly nurture and grow your connections!
Share This Post
-
How To Set Anxiety Aside
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Set Anxiety Aside
We’ve talked previously about how to use the “release” method to stop your racing mind.
That’s a powerful technique, but sometimes we need to be calm enough to use it. So first…
Breathe
Obviously. But, don’t underestimate the immediate power of focusing on your breath, even just for a moment.
There are many popular breathing exercises, but here’s one of the simplest and most effective, “4–4 breathing”:
- Breathe in for a count of four
- Hold for a count four
- Breathe out for a count of four
- Hold for a count of four
- Repeat
Depending on your lung capacity and what you’re used to, it may be that you need to count more quickly or slowly to make it feel right. Experiment with what feels comfortable for you, but the general goal should breathing deeply and slowly.
Identify the thing that’s causing you anxiety
We’ve also talked previously about how to use the RAIN technique to manage difficult emotions, and that’s good for handling anxiety too.
Another powerful tool is journaling.
Read: How To Use Journaling to Challenge Anxious Thoughts
If you don’t want to use any of those (very effective!) methods, that’s fine too—journaling isn’t for everyone.
You can leverage some of the same benefits by simply voicing your worries, even to yourself:
There’s an old folk tradition of “worry dolls”; these are tiny little dolls so small they can be kept in a pocket-size drawstring purse. Last thing at night, the user whispers their worries to the dolls and puts them back in their bag, where they will work on the person’s problem overnight.
We’re a health and productivity newsletter, not a dealer of magic and spells, but you can see how it works, right? It gets the worries out of one’s head, and brings about a helpful placebo effect too.
Focus on what you can control
- Most of what you worry about will not happen.
- Some of what you worry about may happen.
- Worrying about it will not help.
In fact, in some cases it may bring about what you fear, by means of the nocebo effect (like the placebo effect, but bad). Additionally, worrying drains your body and makes you less able to deal with whatever life does throw at you.
So while “don’t worry; be happy” may seem a flippant attitude, sometimes it can be best. However, don’t forget the other important part, which is actually focusing on what you can control.
- You can’t control whether your car will need expensive maintenance…
- …but you can control whether you budget for it.
- You can’t control whether your social event will go well or ill…
- …but you can control how you carry yourself.
- You can’t control whether your loved one’s health will get better or worse…
- …but you can control how you’re there for them, and you can help them take what sensible precautions they may.
…and so forth.
Look after your body as well!
Your body and mind are deeply reliant on each other. In this case, just as anxiety can drain your body’s resources, keeping your body well-nourished, well-exercised, and well-rested and can help fortify you against anxiety. For example, when it comes to diet, exercise, and sleep:
- Read: Fruit and vegetable intake is inversely associated with perceived stress across the adult lifespan
- Read: Exercise and anxiety: physical activity appears to be protective against anxiety disorders in clinical and non-clinical populations
- Read: Sleep problems predict and are predicted by generalized anxiety/depression
Don’t know where to start? How about the scientifically well-researched, evidence-based, 7-minute workout?
Share This Post
Related Posts
-
I’m iron deficient. Which supplements will work best for me and how should I take them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Iron deficiency is common and can be debilitating. It mainly affects women. One in three premenopausal women are low in iron compared to just 5% of Australian men. Iron deficiency particularly affects teenage girls, women who do a lot of exercise and those who are pregnant.
The body needs iron to make new red blood cells, and to support energy production, the immune system and cognitive function. If you’re low, you may experience a range of symptoms including fatigue, weakness, shortness of breath, headache, irregular heartbeat and reduced concentration.
If a blood test shows you’re iron deficient, your doctor may recommend you start taking an oral iron supplement. But should you take a tablet or a liquid? With food or not? And when is the best time of day?
Here are some tips to help you work out how, when and what iron supplement to take.
LittlePigPower/Shutterstock How do I pick the right iron supplement?
The iron in your body is called “elemental iron”. Choosing the right oral supplement and dose will depend on how much elemental iron it has – your doctor will advise exactly how much you need.
The sweet spot is between 60-120 mg of elemental iron. Any less and the supplement won’t be effective in topping up your iron levels. Any higher and you risk gastrointestinal symptoms such as diarrhoea, cramping and stomach pain.
Low iron can especially affect people during pregnancy and women who do a lot of sport. Kamil Macniak/Shutterstock In Australia, iron salts are the most common oral supplements because they are cheap, effective and come in different delivery methods (tablets, capsules, liquid formulas). The iron salts you are most likely to find in your local chemist are ferrous sulfate (~20% elemental iron), ferrous gluconate (~12%) and ferrous fumarate (~33%).
These formulations all work similarly, so your choice should come down to dose and cost.
Many multivitamins may look like an iron supplement, but it’s important to note they usually have too little iron – usually less than 20 mg – to correct an iron deficiency.
Should I take tablets or liquid formulas?
Iron contained within a tablet is just as well absorbed as iron found in a liquid supplement. Choosing the right one usually comes down to personal preference.
The main difference is that liquid formulas tend to contain less iron than tablets. That means you might need to take more of the product to get the right dose, so using a liquid supplement could work out to be more expensive in the long term.
What should I eat with my iron supplement?
Research has shown you will absorb more of the iron in your supplement if you take it on an empty stomach. But this can cause more gastrointestinal issues, so might not be practical for everyone.
If you do take your supplement with meals, it’s important to think about what types of food will boost – rather than limit – iron absorption. For example, taking the supplement alongside vitamin C improves your body’s ability to absorb it.
Some supplements already contain vitamin C. Otherwise you could take the supplement along with a glass of orange juice, or other vitamin C-rich foods.
Taking your supplement alongside foods rich in vitamin C, like orange juice or kiwifruit, can help your body absorb the iron. Anete Lusina/Pexels On the other hand, tea, coffee and calcium all decrease the body’s ability to absorb iron. So you should try to limit these close to the time you take your supplement.
Should I take my supplement in the morning or evening?
The best time of day to take your supplement is in the morning. The body can absorb significantly more iron earlier in the day, when concentrations of hepcidin (the main hormone that regulates iron) are at their lowest.
Exercise also affects the hormone that regulates iron. That means taking your iron supplement after exercising can limit your ability to absorb it. Taking your supplement in the hours following exercise will mean significantly poorer absorption, especially if you take it between two and five hours after you stop.
Our research has shown if you exercise every day, the best time to take your supplement is in the morning before training, or immediately after (within 30 minutes).
My supplements are upsetting my stomach. What should I do?
If you experience gastrointestinal side effects such as diarrhoea or cramps when you take iron supplements, you may want to consider taking your supplement every second day, rather than daily.
Taking a supplement every day is still the fastest way to restore your iron levels. But a recent study has shown taking the same total dose can be just as effective when it’s taken on alternate days. For example, taking a supplement every day for three months works as well as every second day for six months. This results in fewer side effects.
Oral iron supplements can be a cheap and easy way to correct an iron deficiency. But ensuring you are taking the right product, under the right conditions, is crucial for their success.
It’s also important to check your iron levels prior to commencing iron supplementation and do so only under medical advice. In large amounts, iron can be toxic, so you don’t want to be consuming additional iron if your body doesn’t need it.
If you think you may be low on iron, talk to your GP to find out your best options.
Alannah McKay, Postdoctoral Research Fellow, Sports Nutrition, Australian Catholic University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Canned Tuna vs Canned Sardines – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing canned tuna to canned sardines, we picked the sardines.
Why?
This comparison is unfair, but practical—because both are sold next to each other in the supermarket and often used for similar things.
It’s unfair because in a can of tuna, there is tuna meat, whereas in a can of sardines, there is sardine meat, skin, and bones.
Consequently, sardines outperform tuna in almost everything, because a lot of nutrients are in the skin and bones.
To be completely unambiguous:
Sardines have more vitamins and minerals by far (special shout-out to calcium, of which sardines contain 6000% more), and more choline (which is sometimes reckoned as a vitamin, sometimes not).
Tuna does have marginally more protein, and less fat. If you are trying to limit your cholesterol intake, then that could be an argument for choosing tuna over sardines.
All in all: the sardines are more nutrient dense by far, are good sources of vitamins and minerals that tuna contains less of (and in many cases only trace amounts of), and for most people this will more than offset the difference in cholesterol, especially if having not more than one can per day.
About that skin and bones…
That’s where the real benefit for your joints lies, by the way!
See: We Are Such Stuff As Fish Are Made Of
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
We Are Such Stuff As Fish Are Made Of
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Research Review: Collagen
For something that’s a very popular supplement, not many people understand what collagen is, where it comes from, or what it does.
In a nutshell:
Collagen is a kind of protein. Our bodies make it naturally, and we can also get more in our diet and/or take extra as a supplement.
Our bodies use collagen in connective tissue, skin, tendon, bone, and cartilage. It has many functions, but a broad description would be “holding things together”.
As we get older, our bodies produce less collagen. Signs of this include wrinkles, loss of skin hydration, and joint pain.
Quick test: pinch the skin on the middle of the back of one of your hands, and then watch what happens when you get low. How quickly and easily did your skin returns to its original shape?
If it was pretty much instantanous and flawless, congratulations, you have plenty of collagen (and also elastin). If you didn’t, you are probably low on both!
(they are quite similar proteins and are made from the same base “stuff”, so if you’re low on one, you’ll usually be low on both)
Quick note: A lot of research out there has been funded by beauty companies, so we had our work cut out for us today, and have highlighted where any research may be biased.
More than skin deep
While marketing for collagen is almost exclusively aimed at “reduce wrinkles and other signs of aging”, it does a lot more than that.
You remember we mentioned that many things from the bones outward are held together by collagen? We weren’t kidding…
Read: Osteoporosis, like skin ageing, is caused by collagen loss which is reversible
Taking extra collagen isn’t the only way
We can’t (yet!) completely halt the age-related loss of collagen, but we can slow it, with our lifestyle choices:
- Don’t smoke tobacco
- Drink only in moderation (or not at all)
- Avoid foods with added sugar, and high-processed foods in general
- Wear sunscreen when appropriate
Can I get collagen from food?
Yep! Just as collagen holds our bodies together, it holds the bodies of other animals together. And, just like collagen is found in most parts of our body but most plentifully in our skin and bones, that’s what to eat to get collagen from other animals, e.g:
- Chicken skin
- Fish skin
- Bone broth ← health benefits and recipes at this link!
What about vegans?
Yes, vegans are also held together by collagen! We do not, however, recommend eating their skin or boiling their bones into broth. Ethical considerations aside, cannibalism can give you CJD!
More seriously, if you’re vegan, you can’t get collagen from a plant-based diet, but you can get the stuff your body uses to make collagen. Basically, you want to make sure you get plenty of:
- Protein (beans, pulses, nuts, etc are all fine; it’s hard to go wrong with this)
- Vitamin C
- Vitamin D
- and Zinc
Just be sure to continue to remember to avoid highly-processed foods. So:
- Soy mince/chunks whose ingredients list reads: “soya”? Yes!
- The Incredible Burger or Linda McCartney’s Sausages? Sadly less healthy
Read: Advanced Glycation End Products in Foods and a Practical Guide to Their Reduction in the Diet
Meat-eaters might want to read that one too. By far the worst offenders for AGEs (Advanced Glycation End Products, which can not only cause collagen to stiffen, but also inactivate proteins responsible for collagen repair, along with doing much more serious damage to your body’s natural functions) include:
- Hot dogs
- Bacon
- Fried/roasted/grilled meats
Is it worth it as a supplement?
That depends on you, your age, and your lifestyle, but it’s generally considered safe*
*if you have a seafood allergy, be careful though, as many supplements are from fish or shellfish—you will need to find one that’s free from your allergen
Also, all collagen is animal-derived. So if you’re a vegan, decide for yourself whether this constitutes medicine and if so, whether that makes it ethically permissible to you.
With that out of the way:
What the science says on collagen supplementation
Collagen for skin
Read: Effects of collagen supplementation on skin aging (systematic review and meta-analysis)
The short version is that they selected 19 studies with over a thousand participants in total, and they found:
In the meta-analysis, a grouped analysis of studies showed favorable results of hydrolyzed collagen supplementation compared with placebo in terms of skin hydration, elasticity, and wrinkles.
The findings of improved hydration and elasticity were also confirmed in the subgroup meta-analysis.
Based on results, ingestion of hydrolyzed collagen for 90 days is effective in reducing skin aging, as it reduces wrinkles and improves skin elasticity and hydration.
Caveat: while that systematic review had no conflicts of interests, at least some of the 19 studies will have been funded by beauty companies. Here are two, so that you know what that looks like:
Funded by Quiris to investigate their own supplement, Elasten®:
A Collagen Supplement Improves Skin Hydration, Elasticity, Roughness, and Density
Funded by BioCell to investigate their own supplement, BioCell Collagen:
The Effects of Skin Aging Associated with the Use of BioCell Collagen
A note on funding bias: to be clear, the issue is not that the researchers might be corrupt (though that could happen).
The issue is more that sometimes companies will hire ten labs to do ten research studies… and then pull funding from ones whose results aren’t going the way they’d like.
So the “best” (for them) study is the one that gets published.
Here’s another systematic review—like the one at the top of this section—that found the same, with doses ranging from 2.5g–15g per day for 8 weeks or longer:
Read: Oral Collagen Supplementation: A Systematic Review of Dermatological Applications
Again, some of those studies will have been funded by beauty companies. The general weight of evidence does seem clear and favorable, though.
Collagen for bones
Here, we encountered a lot less in the way of potential bias, because this is simply marketed a lot less. Despite being arguably far more important!
We found a high quality multi-vector randomized controlled study with a sample size of 131 postmenopausal women. They had these women take 5g collagen supplement (or placebo), and studied the results over the course of a year.
They found:
- The intake of the supplement increased bone mineral density (BMD)
- Supplementation was also associated with a favorable shift in bone markers, indicating:
- increased bone formation
- reduced bone degradation
Read: Specific Collagen Peptides Improve Bone Mineral Density and Bone Markers in Postmenopausal Wome
A follow-up study with 31 of these women found that taking 5 grams of collagen daily for a total of 4 years was associated with a progressive increase in BMD.
You might be wondering if collagen also helps against osteoarthritis.
The answer is: yes, it does (at least, it significantly reduces the symptoms)
Read: Effect of collagen supplementation on osteoarthritis symptoms
In summary:
- You need collagen for health skin, bones, joints, and more
- Your body makes collagen from your food
- You can help it by getting plenty of protein, vitamins, and minerals
- You can also help it by not doing the usual Bad Things™ (smoking, drinking, eating processed foods, especially processed meats)
- You can also eat collagen directly in the form of other animals’ skin and bones
- You can also buy collagen supplements (but watch out for allergens)
Want to try collagen supplementation?
We don’t sell it (or anything else), but for your convenience…
Check it out: Hydrolyzed Collagen Peptides (the same as in most of the above studies), 90 days supply at 5g/day
We selected this one because it’s the same kind used in many of the studies, and it doesn’t contain any known allergens.
It’s bovine collagen, meaning it’s from cows, so it’s not vegan, and also some subscribers may want to abstain for religious reasons. We respect that, and/but make our recommendations based solely on the science of health and productivity.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: