Semaglutide’s Surprisingly Unexamined Effects
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide’s Surprisingly Big Research Gap
GLP-1 receptor agonists like Ozempic, Wegovy, and other semaglutide drugs. are fast becoming a health industry standard go-to tool in the weight loss toolbox. When it comes to recommending that patients lose weight, “Have you considered Ozempic?” is the common refrain.
Sometimes, this may be a mere case of kicking the can down the road with regard to some other treatment that it can be argued (sometimes even truthfully) would go better after some weight loss:
How weight bias in health care can harm patients with obesity: Research
…which we also covered in fewer words in the second-to-last item here:
But GLP-1 agonists work, right?
Yes, albeit there’s a litany of caveats, top of which are usually:
- there are often adverse gastrointestinal side effects
- if you stop taking them, weight regain generally ensues promptly
For more details on these and more, see:
…but now there’s another thing that’s come to light:
The dark side of semaglutide’s weight loss
In academia, “dark” is often used to describe “stuff we don’t have much (or in some cases, any) direct empirical evidence of, but for reasons of surrounding things, we know it’s there”.
Well-known examples include “dark matter” in physics and the Dark Ages in (European) history.
In the case of semaglutide and weight loss, a review by a team of researchers (Drs. Sandra Christenen, Katie Robinson, Sara Thomas, and Dominique Williams) has discovered how little research has been done into a certain aspect of GLP-1 agonist’s weight loss effects, namely…
Dietary changes!
There’s been a lot of popular talk about “people taking semaglutide eat less”, but it’s mostly anecdotal and/or presumed based on parts of the mechanism of action (increasing insulin production, reducing glucagon secretions, modulating dietary cravings).
Where studies have looked at dietary changes, it’s almost exclusively been a matter of looking at caloric intake (which has been found to be a 16–39% reduction), and observations-in-passing that patients reported reduction in cravings for fatty and sweet foods.
This reduction in caloric intake, by the way, is not significantly different to the reduction brought about by counselling alone (head-to-head studies have been done; these are also discussed in the research review).
However! It gets worse. Very few studies of good quality have been done, even fewer (two studies) actually had a registered dietitian nutritionist on the team, and only one of them used the “gold standard” of nutritional research, the 24-hour dietary recall test. Which, in case you’re curious, you can read about what that is here:
Dietary Assessment Methods: What Is A 24-Hour Recall?
Of the four studies that actually looked at the macros (unlike most studies), they found that on average, protein intake decreased by 17.1%. Which is a big deal!
It’s an especially big deal, because while protein’s obviously important for everyone, it’s especially important for anyone trying to lose weight, because muscle mass is a major factor in metabolic base rate—which in turn is much important for fat loss/maintenance than exercise, when it comes to how many calories we burn by simply existing.
A reasonable hypothesis, therefore, is that one of the numerous reasons people who quit GLP-1 agonists immediately put fat back on, is because they probably lost muscle mass in amongst their weight loss, meaning that their metabolic base rate will have decreased, meaning that they end up more disposed to put on fat than before.
And, that’s just a hypothesis and it’s a hypothesis based on very few studies, so it’s not something to necessarily take as any kind of definitive proof of anything, but it is to say—as the researchers of this review do loudly say—more research needs to be done into this, because this has been a major gap in research so far!
Any other bad news?
While we’re talking research gaps, guess how many studies looked into micronutrient intake changes in people taking GLP-1 agonists?
If you guessed zero, you guessed correctly.
You can find the paper itself here:
What’s the main take-away here?
On a broad, scoping level: we need more research!
On a “what this means for individuals who want to lose weight” level: maybe we should be more wary of this still relatively new (less than 10 years old) “wonder drug”. And for most of those 10 years it’s only been for diabetics, with weight loss use really being in just the past few years (2021 onwards).
In other words: not necessarily any need to panic, but caution is probably not a bad idea, and natural weight loss methods remain very reasonable options for most people.
See also: How To Lose Weight (Healthily!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Coca-Cola vs Diet Coke – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Coca-Cola to Diet Coke, we picked the Diet Coke.
Why?
While the Diet Coke is bad, the Coca-Cola has mostly the same problems plus sugar.
The sugar in a can of Coca-Cola is 39g high-fructose corn syrup (the worst kind of sugar yet known to humanity), and of course it’s being delivered in liquid form (the most bioavailable way to get, which in this case, is bad).
To put those 39g into perspective, the daily recommended amount of sugar is 36g for men or 25g for women, according to the AHA.
The sweetener in Diet Coke is aspartame, which has had a lot of health risk accusations made against it, most of which have not stood up to scrutiny, and the main risk it does have is “it mimics sugar too well” and it can increase cravings for sweetness, and therefore higher consumption of sugars in other products. For this reason, the World Health Organization has recommended to simply reduce sugar intake without looking to artificial sweeteners to help.
Nevertheless, aspartame has been found safe (in moderate doses; the upper tolerance level would equate to more than 20 cans of diet coke per day) by food safety agencies ranging from the FDA to the EFSA, based on a large body of science.
Other problems that Diet Coke has are present in Coca-Cola too, such as its acidic nature (bad for tooth enamel) and gassy nature (messes with leptin/ghrelin balance).
Summary: the Diet Coke is relatively less unhealthy, but is still bad in numerous ways, and remains best avoided.
Read more:
Share This Post
-
How Your Exercise Today Gives A Brain Boost Tomorrow
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Regular 10almonds readers may remember we not long back wrote about a study that showed how daily activity levels, in aggregate, make a difference to brain health over the course of 1–2 weeks (in fact, it was a 9-day study):
Daily Activity Levels & The Measurable Difference They Make To Brain Health
Today, we’re going to talk about a new (published today, at time of writing) study that shows the associations between daily exercise levels (amongst other things) and how well people performed in cognitive tests the next day.
By this we mean: they recorded exercise vs sedentary behavior vs sleep on a daily basis (using wearable tech to track it), and tested them daily with cognitive tests, and looked at how the previous day’s activities (or lack thereof) impacted the next day’s test results.
Notably, the sample was of older adults (aged 50–83). The sample size wasn’t huge but was statistically significant (n=76) and the researchers are of course calling for more studies to be done with more people.
What they found
To put their findings into few words:
- Consistent light exercise boosts general cognitive performance not just for hours (which was already known) but through the next day.
- More moderate or vigorous activity than usual in particular led to better working memory and episodic memory the next day.
- More sleep (especially slow-wave deep sleep) improved episodic memory and psychomotor speed.
- Sedentary behavior was associated with poorer working memory.
Let’s define some terms:
- general cognitive performance = average of scores across the different tests
- working memory = very short term memory, such as remembering what you came into this room for, or (as an example of a test format) being able to take down a multi-digit number in one go without it being broken down (and then, testing with longer lengths of number until failure)
- episodic memory = memory of events in a narrative context, where and when they happened, etc
- psychomotor speed = the speed of connection between perception and reaction in quick-response tests
These are, of course, all useful things to have, which means the general advice here is to:
- move more, generally
- exercise more, specifically
- sit less, whenever reasonably possible
- sleep well
You can read the study itself here:
Want to know the best kind of exercise for brain health?
Check out our article about neuroscientist Dr. Suzuki, and what she has to say about it:
The Exercise That Protects Your Brain
Enjoy!
Share This Post
-
The Best Menopause Advice You Don’t Want To Hear About
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nutritionist and perimenopause coach Claudia Canu, whom we’ve featured before in our Expert Insights segment, has advice:
Here’s to good health
When it comes to alcohol, the advice is: don’t.
Or at least, cut back, and manage the effects by ensuring good hydration, having an “alcohol curfew” and so forth.
What’s the relation to menopause? Well, alcohol’s not good for anyone at any time of life, but there are some special considerations when it comes to alcohol and estrogenic hormonal health:
- The liver works hard to process the alcohol as a matter of urgency, delaying estrogen processing, which can increase the risk of breast and uterine cancer.
- Alcohol has no positive health effects and is also linked to higher risks of breast and colorectal cancer.
- Alcohol can also trigger some menopausal symptoms, such as night sweats and hot flashes. So, maybe reaching for that “cooling drink” isn’t the remedy it might seem.
- During menopause, the body becomes more insulin-resistant, making it more susceptible to blood sugar spikes caused by alcohol. Also not good.
Common reasons women turn to alcohol include stress, frustration, the need for reward, and social pressure, and all of these can be heightened when undergoing hormonal changes. Yet, alcohol will ultimately only worsen each of those things.
For more on the science of some of the above, plus tips on how to make positive changes with minimum discomfort, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- How To Reduce Or Quit Alcohol
- How To Reduce The Harm Of Drinking (Without Abstaining)
- Where Nutrition Meets Habits! ← our “Expert Insights” spotlight on Canu
- How To Reduce Your Alzheimer’s Risk Early ← particularly important at this life stage
Take care!
Share This Post
Related Posts
-
What Actually Causes High Cholesterol?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In 1968, the American Heart Association advised limiting egg consumption to three per week due to cholesterol concerns linked to cardiovascular disease. Which was reasonable based on the evidence available back then, but it didn’t stand the test of time.
Eggs are indeed high in cholesterol, but that doesn’t mean that those who eat them will also be high in cholesterol, because…
It’s not quite what many people think
Some quite dietary pointers to start with:
- Egg yolks are high in cholesterol but have a minimal impact on blood cholesterol.
- Saturated and trans fats (as found in fatty meats or dairy, and some processed foods) have a greater influence on LDL levels than dietary cholesterol.
And on the other hand:
- Unsaturated fats (e.g. from fish, nuts, seeds) have anti-inflammatory benefits
- Fiber-rich foods help lower LDL by affecting fat absorption in the digestive tract
A quick primer on LDL and other kinds of cholesterol:
- VLDL (Very Low-Density Lipoprotein):
- delivers triglycerides and cholesterol to muscle and fat cells for energy
- is converted into LDL after delivery
- LDL (Low-Density Lipoprotein):
- is called “bad cholesterol”, which we call that due to its role in arterial plaque formation
- in excess leads to inflammation, overworked macrophage activity, and artery narrowing
- HDL (High-Density Lipoprotein):
- known as “good cholesterol,” picks up excess LDL and returns it to the liver for excretion
- is anti-inflammatory, in addition to regulating LDL levels
There are other factors too, for example:
- Smoking and drinking increase LDL buildup and cause oxidative damage to lipids in general and the blood vessels through which they travel
- Regular exercise, meanwhile, can lower LDL and raise HDL
- Statins and other medications can help lower LDL and manage cholesterol when lifestyle changes and genetics require additional support—but they often come with serious side effects, and the usefulness varies from person to person.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
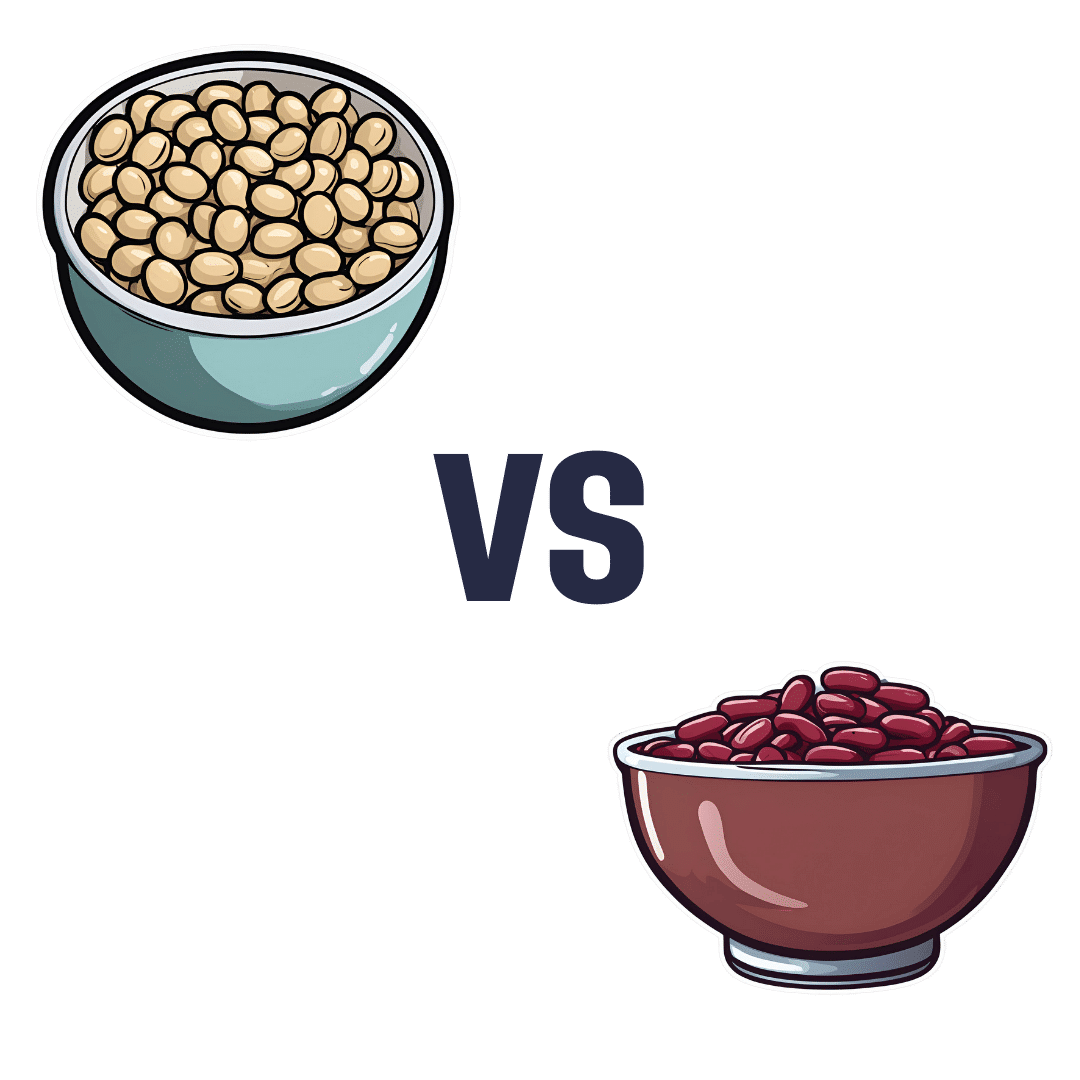
Soy Beans vs Kidney Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing soy beans to kidney beans, we picked the soy.
Why?
In terms of macros, soy has 2x the protein, while kidney beans have nearly 3x the carbs and very slightly more fiber. Ratio-wise, the “very slightly more fiber” does not offset the “nearly 3x the carbs” when it comes to glycemic index (though both are still good, really, but this is a head-to-head so the comparison is relevant), and 2x the protein is also quite a bonus, so this category’s an easy win for soy.
In the category of vitamins, soy beans have more of vitamins A, B2, B6, C, E, K, and choline, while kidney beans have more of vitamins B3, B5, and B9, thus making for a 7:3 win for soy.
When it comes to minerals, soy beans have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while kidney beans are not higher in any mineral. Another clear win for soy.
Adding up the three strong wins for soy, makes for an overall easy win for soy. Still, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Plant vs Animal Protein: Head to Head
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healthy Kids, Happy Kids – by Dr. Elisa Song
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you have young children or perhaps grandchildren, you probably care deeply about those children and their wellbeing, but there can often be a lot more guesswork than would be ideal, when it comes to ensuring they be and remain healthy.
Nevertheless, a lot of common treatments for children are based (whether parents know it or not—and often they dont) on what is most convenient for the parent, not necessarily what is best for the child. Dr. Song looks to correct that.
Rather than dosing kids with acetaminophen or even antibiotics, assuming eczema can be best fixed with a topical cream (treating the symptom rather than the cause, much?), and that some things like asthma “just are”, and “that’s unfortunate”, Dr. Song takes us on a tour of pediatric health, centered around the gut.
Why the gut? Well, it’s pretty central to us as adults, and it’s the same for kids, except one difference: their gut microbiome is changing even more quickly than ours (along with the rest of their body), and as such, is even more susceptible to little nudges for better or for worse, having a big impact in either direction. So, might as well make it a good one!
After an explanatory overview, most of the book is given over to recognizing and correcting what things can go wrong, including the top 25 acute childhood conditions, and the most critical chronic ones, and how to keep things on-track as a team (the child is part of the team! An important part!).
The style of the book is very direct and instructional; easy to understand throughout. It’s a lot like being in a room with a very competent pediatrician who knows her stuff and explains it well, thus neither patronizing nor mystifying.
Bottom line: if there are kids in your life, be they yours or your grandkids or someone else, this is a fine book for giving them the best foundational health.
Click here to check out Healthy Kids, Happy Kids, and take care of yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: