Prolonged Grief: A New Mental Disorder?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The issue is not whether certain mental conditions are real—they are. It is how we conceptualize them and what we think treating them requires.
The latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) features a new diagnosis: prolonged grief disorder—used for those who, a year after a loss, still remain incapacitated by it. This addition follows more than a decade of debate. Supporters argued that the addition enables clinicians to provide much-needed help to those afflicted by what one might simply consider a too much of grief, whereas opponents insisted that one mustn’t unduly pathologize grief and reject an increasingly medicalized approach to a condition that they considered part of a normal process of dealing with loss—a process which in some simply takes longer than in others.
By including a condition in a professional classification system, we collectively recognize it as real. Recognizing hitherto unnamed conditions can help remove certain kinds of disadvantages. Miranda Fricker emphasizes this in her discussion of what she dubs hermeneutic injustice: a specific sort of epistemic injustice that affects persons in their capacity as knowers1. Creating terms like ‘post-natal depression’ and ‘sexual harassment’, Fricker argues, filled lacunae in the collectively available hermeneutic resources that existed where names for distinctive kinds of social experience should have been. The absence of such resources, Fricker holds, put those who suffered from such experiences at an epistemic disadvantage: they lacked the words to talk about them, understand them, and articulate how they were wronged. Simultaneously, such absences prevented wrong-doers from properly understanding and facing the harm they were inflicting—e.g. those who would ridicule or scold mothers of newborns for not being happier or those who would either actively engage in sexual harassment or (knowingly or not) support the societal structures that helped make it seem as if it was something women just had to put up with.
For Fricker, the hermeneutical disadvantage faced by those who suffer from an as-of-yet ill-understood and largely undiagnosed medical condition is not an epistemic injustice. Those so disadvantaged are not excluded from full participation in hermeneutic practices, or at least not through mechanisms of social coercion that arise due to some structural identity prejudice. They are not, in other words, hermeneutically marginalized, which for Fricker, is an essential characteristic of epistemic injustice. Instead, their situation is simply one of “circumstantial epistemic bad luck”2. Still, Fricker, too, can agree that providing labels for ill-understood conditions is valuable. Naming a condition helps raise awareness of it, makes it discursively available and, thus, a possible object of knowledge and understanding. This, in turn, can enable those afflicted by it to understand their experience and give those who care about them another way of nudging them into seeking help.
Surely, if adding prolonged grief disorder to the DSM-5 were merely a matter of recognizing the condition and of facilitating assistance, nobody should have any qualms with it. However, the addition also turns intense grief into a mental disorder—something for whose treatment insurance companies can be billed. With this, significant forces of interest enter the scene. The DSM-5, recall, is mainly consulted by psychiatrists. In contrast to talk-therapists like psychotherapists or psychoanalysts, psychiatrists constitute a highly medicalized profession, in which symptoms—clustered together as syndromes or disorders—are frequently taken to require drugs to treat them. Adding prolonged grief disorder thus heralds the advent of research into various drug-based grief therapies. Ellen Barry of the New York Times confirms this: “naltrexone, a drug used to help treat addiction,” she reports, “is currently in clinical trials as a form of grief therapy”, and we are likely to see a “competition for approval of medicines by the Food and Drug Administration.”3
Adding diagnoses to the DSM-5 creates financial incentives for players in the pharmaceutical industry to develop drugs advertised as providing relief to those so diagnosed. Surely, for various conditions, providing drug-induced relief from severe symptoms is useful, even necessary to enable patients to return to normal levels of functioning. But while drugs may help suppress feelings associated with intense grief, they cannot remove the grief. If all mental illnesses were brain diseases, they might be removed by adhering to some drug regimen or other. Note, however, that ‘mental illness’ is a metaphor that carries the implicit suggestion that just like physical illnesses, mental afflictions, too, are curable by providing the right kind of physical treatment. Unsurprisingly, this metaphor is embraced by those who stand to massively benefit from what profits they may reap from selling a plethora of drugs to those diagnosed with any of what seems like an ever-increasing number of mental disorders. But metaphors have limits. Lou Marinoff, a proponent of philosophical counselling, puts the point aptly:
Those who are dysfunctional by reason of physical illness entirely beyond their control—such as manic-depressives—are helped by medication. For handling that kind of problem, make your first stop a psychiatrist’s office. But if your problem is about identity or values or ethics, your worst bet is to let someone reify a mental illness and write a prescription. There is no pill that will make you find yourself, achieve your goals, or do the right thing.
Much more could be said about the differences between psychotherapy, psychiatry, and the newcomer in the field: philosophical counselling. Interested readers may benefit from consulting Marinoff’s work. Written in a provocative, sometimes alarmist style, it is both entertaining and—if taken with a substantial grain of salt—frequently insightful. My own view is this: from Fricker’s work, we can extract reasons to side with the proponents of adding prolonged grief disorder to the DSM-5. Creating hermeneutic resources that allow us to help raise awareness, promote understanding, and facilitate assistance is commendable. If the addition achieves that, we should welcome it. And yet, one may indeed worry that practitioners are too eager to move from the recognition of a mental condition to the implementation of therapeutic interventions that are based on the assumption that such afflictions must be understood on the model of physical disease. The issue is not whether certain mental conditions are real—they are. It is how we conceptualize them and what we think treating them requires.
No doubt, grief manifests physically. It is, however, not primarily a physical condition—let alone a brain disease. Grief is a distinctive mental condition. Apart from bouts of sadness, its symptoms typically include the loss of orientation or a sense of meaning. To overcome grief, we must come to terms with who we are or can be without the loved one’s physical presence in our life. We may need to reinvent ourselves, figure out how to be better again and whence to derive a new purpose. What is at stake is our sense of identity, our self-worth, and, ultimately, our happiness. Thinking that such issues are best addressed by popping pills puts us on a dangerous path, leading perhaps towards the kind of dystopian society Aldous Huxley imagined in his 1932 novel Brave New World. It does little to help us understand, let alone address, the moral and broader philosophical issues that trouble the bereaved and that lie at the root not just of prolonged grief but, arguably, of many so-called mental illnesses.
Footnotes:
1 For this and the following, cf. Fricker 2007, chapter 7.
2 Fricker 2007: 152
3 Barry 2022
References:
Barry, E. (2022). “How Long Should It Take to Grieve? Psychiatry Has Come Up With an Answer.” The New York Times, 03/18/2022, URL = https://www.nytimes.com/2022/03/18/health/prolonged-grief-
disorder.html [last access: 04/05/2022])
Fricker, M. (2007). Epistemic Injustice. Power & the Ethics of knowing. Oxford/New York: Oxford University Press.
Huxley, A. (1932). Brave New World. New York: Harper Brothers.
Marinoff, L. (1999). Plato, not Prozac! New York: HarperCollins Publishers.
Professor Raja Rosenhagen is currently serving as Assistant Professor of Philosophy, Head of Department, and Associate Dean of Academic Affairs at Ashoka University. He earned his PhD in Philosophy from the University of Pittsburgh and has a broad range of philosophical interests (see here). He wrote this article a) because he was invited to do so and b) because he is currently nurturing a growing interest in philosophical counselling.
This article is republished from OpenAxis under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Kiwi Fruit vs Pineapple – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi fruit to pineapple, we picked the kiwi.
Why?
In terms of macros, they’re mostly quite comparable, being fruits made of mostly water, and a similar carb count (slightly different proportions of sugar types, but nothing that throws out the end result, and the GI is low for both). Technically kiwi has twice the protein, but they are fruits and “twice the protein” means “0.5g difference per 100g”. Aside from that, and more meaningfully, kiwi also has twice the fiber.
When it comes to vitamins, kiwi has more of vitamins A, B9, C, E, K, and choline, while pineapple has more of vitamins B1, B2, B3, B5, and B6. This would be a marginal (6:5) win for kiwi, but kiwi’s margins of difference are greater per vitamin, including 72x more vitamin E (with a cupful giving 29% of the RDA, vs a cupful of pineapple giving 0.4% of the RDA) and 57x more vitamin K (with a cupful giving a day’s RDA, vs a cupful of pineapple giving a little under 2% of the RDA). So, this is a fair win for kiwi.
In the category of minerals, things are clear: kiwi has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while pineapple has more manganese. An overwhelming win for kiwi.
Looking at their respective anti-inflammatory powers, pineapple has its special bromelain enzymes, which is a point in its favour, but when it comes to actual polyphenols, the two fruits are quite balanced, with kiwi’s flavonoids vs pineapple’s lignans.
Adding up the sections, it’s a clear win for kiwi—but pineapple is a very respectable fruit too (especially because of its bromelain content), so do enjoy both!
Want to learn more?
You might like to read:
Bromelain vs Inflammation & Much More
Take care!
Share This Post
-
7 Steps to Get Off Sugar and Carbohydrates – by Susan Neal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We will not keep the steps a mystery; abbreviated, they are:
- decide to really do this thing
- get knowledge and support
- clean out that pantry/fridge/etc and put those things behind you
- buy in healthy foods while starving your candida
- plan for an official start date, so that everything is ready
- change the way you eat (prep methods, timings, etc)
- keep on finding small ways to improve, without turning back
Particularly important amongst those are starving the candida (the fungus in your gut that is responsible for a lot of carb cravings, especially sugar and alcohol—which latter can be broken down easily into sugar), and changing the “how” of eating as well as the “what”; those are both things that are often overlooked in a lot of guides, but this one delivers well.
Walking the reader by the hand through things like that is probably the book’s greatest strength.
In the category of subjective criticism, the author does go off-piste a little at the end, to take a moment while she has our attention to talk about other things.
For example, you may not need “Appendix 7: How to Become A Christian and Disciple of Jesus Christ”.
Of course if that calls to you, then by all means, follow your heart, but it certainly isn’t a necessary step of quitting sugar. Nevertheless, the diversion doesn’t detract from the good dietary change advice that she has just spent a book delivering.
Bottom line: there’s no deep science here, but there’s a lot of very good, very practical advice, that’s consistent with good science.
Click here to check out 7 Steps to Get Off Sugar, and watch your health improve!
Share This Post
-
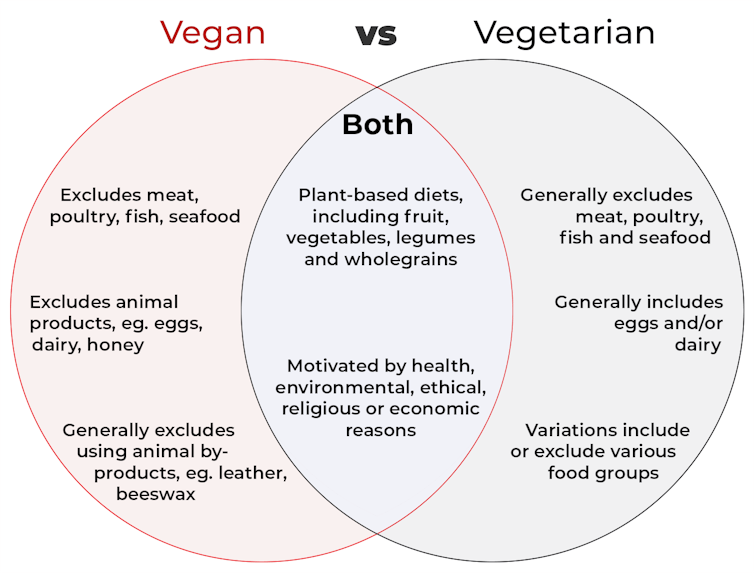
What’s the difference between vegan and vegetarian?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
Vegan and vegetarian diets are plant-based diets. Both include plant foods, such as fruits, vegetables, legumes and whole grains.
But there are important differences, and knowing what you can and can’t eat when it comes to a vegan and vegetarian diet can be confusing.
So, what’s the main difference?
Creative Cat Studio/Shutterstock What’s a vegan diet?
A vegan diet is an entirely plant-based diet. It doesn’t include any meat and animal products. So, no meat, poultry, fish, seafood, eggs, dairy or honey.
What’s a vegetarian diet?
A vegetarian diet is a plant-based diet that generally excludes meat, poultry, fish and seafood, but can include animal products. So, unlike a vegan diet, a vegetarian diet can include eggs, dairy and honey.
But you may be wondering why you’ve heard of vegetarians who eat fish, vegetarians who don’t eat eggs, vegetarians who don’t eat dairy, and even vegetarians who eat some meat. Well, it’s because there are variations on a vegetarian diet:
- a lacto-ovo vegetarian diet excludes meat, poultry, fish and seafood, but includes eggs, dairy and honey
- an ovo-vegetarian diet excludes meat, poultry, fish, seafood and dairy, but includes eggs and honey
- a lacto-vegetarian diet excludes meat, poultry, fish, seafood and eggs, but includes dairy and honey
- a pescatarian diet excludes meat and poultry, but includes eggs, dairy, honey, fish and seafood
- a flexitarian, or semi-vegetarian diet, includes eggs, dairy and honey and may include small amounts of meat, poultry, fish and seafood.
Are these diets healthy?
A 2023 review looked at the health effects of vegetarian and vegan diets from two types of study.
Observational studies followed people over the years to see how their diets were linked to their health. In these studies, eating a vegetarian diet was associated with a lower risk of developing cardiovascular disease (such as heart disease or a stroke), diabetes, hypertension (high blood pressure), dementia and cancer.
For example, in a study of 44,561 participants, the risk of heart disease was 32% lower in vegetarians than non-vegetarians after an average follow-up of nearly 12 years.
Further evidence came from randomised controlled trials. These instruct study participants to eat a specific diet for a specific period of time and monitor their health throughout. These studies showed eating a vegetarian or vegan diet led to reductions in weight, blood pressure, and levels of unhealthy cholesterol.
For example, one analysis combined data from seven randomised controlled trials. This so-called meta-analysis included data from 311 participants. It showed eating a vegetarian diet was associated with a systolic blood pressure (the first number in your blood pressure reading) an average 5 mmHg lower compared with non-vegetarian diets.
It seems vegetarian diets are more likely to be healthier, across a number of measures.
For example, a 2022 meta-analysis combined the results of several observational studies. It concluded a vegetarian diet, rather than vegan diet, was recommended to prevent heart disease.
There is also evidence vegans are more likely to have bone fractures than vegetarians. This could be partly due to a lower body-mass index and a lower intake of nutrients such as calcium, vitamin D and protein.
But it can be about more than just food
Many vegans, where possible, do not use products that directly or indirectly involve using animals.
So vegans would not wear leather, wool or silk clothing, for example. And they would not use soaps or candles made from beeswax, or use products tested on animals.
The motivation for following a vegan or vegetarian diet can vary from person to person. Common motivations include health, environmental, ethical, religious or economic reasons.
And for many people who follow a vegan or vegetarian diet, this forms a central part of their identity.
More than a diet: veganism can form part of someone’s identity. Shutterstock So, should I adopt a vegan or vegetarian diet?
If you are thinking about a vegan or vegetarian diet, here are some things to consider:
- eating more plant foods does not automatically mean you are eating a healthier diet. Hot chips, biscuits and soft drinks can all be vegan or vegetarian foods. And many plant-based alternatives, such as plant-based sausages, can be high in added salt
- meeting the nutrient intake targets for vitamin B12, iron, calcium, and iodine requires more careful planning while on a vegan or vegetarian diet. This is because meat, seafood and animal products are good sources of these vitamins and minerals
- eating a plant-based diet doesn’t necessarily mean excluding all meat and animal products. A healthy flexitarian diet prioritises eating more whole plant-foods, such as vegetables and beans, and less processed meat, such as bacon and sausages
- the Australian Dietary Guidelines recommend eating a wide variety of foods from the five food groups (fruit, vegetables, cereals, lean meat and/or their alternatives and reduced-fat dairy products and/or their alternatives). So if you are eating animal products, choose lean, reduced-fat meats and dairy products and limit processed meats.
Katherine Livingstone, NHMRC Emerging Leadership Fellow and Senior Research Fellow at the Institute for Physical Activity and Nutrition, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Human Connection In An All-Too-Busy World
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many of us, in many ways, have more discretionary time than ever… On paper.
But rather than the 8-hour block of work of yesteryear, nowadays the things that take our time often come in a series of short bursts that punctuate our day.
This means that while in theory, we have n hours of “free” time per day, we actually have 9 minutes here, 23 minutes there, 1 hour 6 minutes somewhere else, and so on.
Social commitments, meanwhile, tend to require not only that we have time in a block, but also, that the time around that block also be sufficiently free, for travelling, preparation, etc.
The result? “We must do this again, and not leave it so long next time!” we say, sincerely, to the friend whom we will next see again in approximately 17 months’ time.
The problem is how our many theoretically-small obligations reduce the rest of our time to “time confetti”, and that happens on the large scale like we saw above, as well as on the small scale of “Ah, I have an hour to relax between these two things” and then suddenly the time is gone, once again reduced to time confetti:
Time Confetti and the Broken Promise of Leisure
So, how to maintain human connection with people beyond those with whom we live?
Some is infinitely better than none
Let’s say you want to call a friend or relative. There may be generational differences in how much one is expected to arrange this by text first, vs just calling, but either way, you don’t have to have an open-ended block of time, and sometimes, it’s better if you don’t.
Establish, at the start of the call, “Before we get into catching up, how are we for time, by the way? For my part, I’ll have to go by such-and-such a time”, and then work with that.
The benefit of doing this is that you’ll both know enough about the time constraints to use the time appropriately; you won’t run out the clock on smalltalk before getting to something big, and you’ll both come away feeling satisfied that you shared and were shared-with in a meaningful fashion.
In contrast, guessing at time constraints can leave big things clipped off, or else result in someone “looking for a way to politely end this conversation that stopped being interesting a while ago but it’ll seem rude if I say I have to go now”, of the kind that results in someone not being so open to a call next time.
Don’t rush to dismiss texts as a medium for meaningful connection
When text messages were first a thing, you’ll remember how we were all working within a very short character limit and a cost-per-message. It was telegrams for the modern age, basically.
Nowadays, that isn’t so; we can write as much or as little as we like, and this has two benefits:
- We can have longer, meaningful conversations around the other stuff in our life. We can reply in seconds, or after making a cup of tea and thinking about it, or after our grocery-chopping trip, or whenever suits us. Suddenly, time confetti isn’t such a barrier to human connection. Writer’s example: my prime social time in this manner is when I’m cooking dinner (which is often about an hour). There’s no way I could have a phonecall while doing that; my bad hearing notwithstanding, I just have my hands full too often with much else going on. But texting? I can do that in the several-minute gaps between assorted culinary tasks, while I’m waiting for the kettle to boil or the onions to brown or whatever.
- Sometimes, the brevity makes it easier. A quick text saying “Hey, just to let you know I’m thinking of you, and hope your day is going well!”, or “Unrelated to anything: I was just thinking about how I’m glad to have you in my life; you’re a good friend, and I appreciate that more than I often remember to say. Anyway, that’s all; it was just on my mind. I hope your day is going well!”
(The cheery closing words in those last two text message examples help signify: “don’t worry, I’m fine and am not looking for anything from you”, which will help the recipient to relax, and counterintuitively, more likely to reply with some kind words of their own, knowing that they’re not signing up for a potentially deep talk when they also have time confetti issues going on)
Seize the moment (and also let it go)
You probably have many small interactions with strangers, most days. In the store, walking the dog, at the doctor’s office, etc. So, two things:
- Make smalltalk. And if you’re not one for traditional smalltalk topics (weather etc), or even if you are, a level-up is:
- Compliment sincerely. Straight out of “How To Win Friends And Influence People”, of course, but it creates a moment of genuine connection; you say a thing, their day is improved, they smile, you complete your business with a smile of your own and go about your day.
(of course, do steer clear of anything that could be interpreted as flirting, if that is not your intent, and really it should never be your intent when it comes to the captive audience of someone who will get fired if they’re not nice to you)
But, with a little practice, these little moments add up to a lot more human connection than if we treat the strangers with whom we interact as though they were merely part of the scenery.
Want more than that?
Check out:
How To Beat Loneliness & Isolation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Freekeh Tomato Feast
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fiber-dense freekeh stars in this traditional Palestinian dish, and the whole recipe is very gut-healthy, not to mention delicious and filling, as well as boasting generous amounts of lycopene and other phytonutrients:
You will need
- 1 cup dried freekeh (if avoiding gluten, substitute a gluten-free grain, or pseudograin such as buckwheat; if making such a substitution, then also add 1 tbsp nutritional yeast—for the flavor as well as the nutrients)
- 1 medium onion, thinly sliced
- 1 2oz can anchovies (if vegan/vegetarian, substitute 1 can kimchi)
- 1 14oz can cherry tomatoes
- 1 cup halved cherry tomatoes, fresh
- ½ cup black olives, pitted
- 1 5oz jar roasted peppers, chopped
- ½ bulb garlic, thinly sliced
- 2 tsp black pepper
- 1 tsp chili flakes
- 1 sprig fresh thyme
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Place a heavy-based (cast iron, if you have it) sauté pan over a medium heat. Add some olive oil, then the onion, stirring for about 5 minutes.
2) Add the anchovies, herbs and spices (including the garlic), and stir well to combine. The anchovies will probably soon melt into the onion; that’s fine.
3) Add the canned tomatoes (but not the fresh), followed by the freekeh, stirring well again to combine.
4) Add 2 cups boiling water, and simmer with the lid on for about 40 minutes. Stir occasionally and check the water isn’t getting too low; top it up if it’s getting dry and the freekeh isn’t tender yet.
5) Add the fresh chopped cherry tomatoes and the chopped peppers from the jar, as well as the olives. Stir for just another 2 minutes, enough to let the latest ingredients warm through.
6) Serve, adding a garnish if you wish:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Eat More (Of This) For Lower Blood Pressure
- Making Friends With Your Gut (You Can Thank Us Later)
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hormone Replacement
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I cant believe 10 Almonds addresses questions. Thanks. I see the word symptoms for menopause. I don’t know what word should replace it but maybe one should be used or is symptom accurate? And I recently read that there was a great disservice for women in my era as they were denied/scared of hormones replacement. Unnecessarily❞
You’d better believe it! In fact we love questions; they give us things to research and write about.
“Symptom” is indeed an entirely justified word to use, being:
- General: any phenomenon or circumstance accompanying something and serving as evidence of it.
- Medical: any phenomenon that arises from and accompanies a particular disease or disorder and serves as an indication of it.
If the question is more whether the menopause can be considered a disease/disorder, well, it’s a naturally occurring and ultimately inevitable change, yes, but then, so is cancer (it’s in the simple mathematics of DNA replication and mutation that, unless a cure for cancer is found, we will always eventually get cancer, if nothing else kills us first).
So, something being natural/inevitable isn’t a reason to not consider it a disease/disorder, nor a reason to not treat it as appropriate if it is causing us harm/discomfort that can be safely alleviated.
Moreover, and semantics aside, it is medical convention to consider menopause to be a medical condition, that has symptoms. Indeed, for example, the US’s NIH (and its constituent NIA, the National Institute of Aging) and the UK’s NHS, both list the menopause’s symptoms, using that word:
- NIA (NIH): What are the signs and symptoms of menopause?
- NHS: Common symptoms of menopause and perimenopause
With regard to fearmongering around HRT, certainly that has been rife, and there were some very flawed (and later soundly refuted) studies a while back that prompted this—and even those flawed studies were not about the same (bioidentical) hormones available today, in any case. So even if they had been correct (they weren’t), it still wouldn’t be a reason to not get treatment nowadays, if appropriate!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: