Shedding Some Obesity Myths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s shed some obesity myths!
There are a lot of myths and misconceptions surrounding obesity… And then there are also reactive opposite myths and misconceptions, which can sometimes be just as harmful!
To tackle them all would take a book, but in classic 10almonds style, we’re going to put a spotlight on some of the ones that might make the biggest difference:
True or False: Obesity is genetically pre-determined
False… With caveats.
Some interesting results have been found from twin studies and adoption studies, showing that genes definitely play some role, but lifestyle is—for most people—the biggest factor:
- The body-mass index of twins who have been reared apart
- An adoption study of human obesity
- Using a sibling-adoption design to parse genetic and environmental influences on children’s body mass index
In short: genes predispose; they don’t predetermine. But that predisposition alone can make quite a big difference, if it in turn leads to different lifestyle factors.
But upon seeing those papers centering BMI, let’s consider…
True or False: BMI is a good, accurate measure of health in the context of bodyweight
False… Unless you’re a very large group of thin white men of moderate height, which was the demographic the system was built around.
Bonus information: it was never intended to be used to measure the weight-related health of any individual (not even an individual thin white man of moderate height), but rather, as a tool to look at large-scale demographic trends.
Basically, as a system, it’s being used in a way it was never made for, and the results of that misappropriation of an epidemiological tool for individual health are predictably unhelpful.
To do a deep-dive into all the flaws of the BMI system, which are many, we’d need to devote a whole main feature just to that.
Update: we have now done so!
Here it is: When BMI Doesn’t Measure Up
True or False: Obesity does not meaningfully impact more general health
False… In more ways than one (but there are caveats)
Obesity is highly correlated with increased risk of all-cause mortality, and weight loss, correspondingly, correlates with a reduced risk. See for example:
So what are the caveats?
Let’s put it this way: owning a horse is highly correlated with increased healthy longevity. And while owning a horse may come with some exercise and relaxation (both of which are good for the health), it’s probably mostly not the horse itself that conveys the health benefits… it’s that someone who has the resources to look after a horse, probably has the resources to look after their own health too.
So sometimes there can be a reason for a correlation (it’s not a coincidence!) but the causative factor is partially (or in some cases, entirely) something else.
So how could this play out with obesity?
There’s a lot of discrimination in healthcare settings, unfortunately! In this case, it often happens that a thin person goes in with a medical problem and gets treated for that, while a fat person can go in with the same medical problem and be told “you should try losing some weight”.
Top tip if this happens to you… Ask: “what would you advise/prescribe to a thin person with my same symptoms?”
Other things may be more systemic, for example:
When a thin person goes to get their blood pressure taken, and that goes smoothly, while a fat person goes to get their blood pressure taken, and there’s not a blood pressure cuff to fit them, is the problem the size of the person or the size of the cuff? It all depends on perspective, in a world built around thin people.
That’s a trivial-seeming example, but the same principle has far-reaching (and harmful) implications in healthcare in general, e.g:
- Surgeons being untrained (and/or unwilling) to operate on fat people
- Getting a one-size-fits-all dose that was calculated using average weight, and now doesn’t work
- MRI machines are famously claustrophobia-inducing for thin people; now try not fitting in it in the first place
…and so forth. So oftentimes, obesity will be correlated with a poor healthcare outcome, where the problem is not actually the obesity itself, but rather the system having been set up with thin people in mind.
It would be like saying “Having O- blood type results in higher risks when receiving blood transfusions”, while omitting to add “…because we didn’t stock O- blood”.
True or False: to reduce obesity, just eat less and move more!
False… Mostly.
Moving more is almost always good for most people. When it comes to diet, quality is much more important than quantity. But these factors alone are only part of the picture!
But beyond diet and exercise, there are many other implicated factors in weight gain, weight maintenance, and weight loss, including but not limited to:
- Disrupted sleep
- Chronic stress
- Chronic pain
- Hormonal imbalances
- Physical disabilities that preclude a lot of exercise
- Mental health issues that add (and compound) extra levels of challenge
- Medications that throw all kinds of spanners into the works with their side effects
…and even just those first two things, diet and exercise, are not always so correlated to weight as one might think—studies have found that the difference for exercise especially is often marginal:
Read: Widespread misconceptions about obesity ← academic article in the Journal of the College of Family Physicians of Canada
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ginger Does A Lot More Than You Think
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ginger’s benefits go deep!
You are doubtlessly already familiar with what ginger is, so let’s skip right into the science.
The most relevant active compound in the ginger root is called gingerol, and people enjoy it not just for its taste, but also a stack of health reasons, such as:
- For weight loss
- Against nausea
- Against inflammation
- For cardiovascular health
- Against neurodegeneration
Quite a collection! So, what does the science say?
For weight loss
This one’s quite straightforward. It not only helps overall weight loss, but also specifically improves waist-hip ratio, which is a much more important indicator of health than BMI.
Against nausea & pain
Ginger has proven its effectiveness in many high quality clinical trials, against general nausea, post-surgery nausea, chemotherapy-induced nausea, and pregnancy-related nausea.
Source: Ginger on Human Health: A Comprehensive Systematic Review of 109 Randomized Controlled Trials
However! While it very clearly has been shown to be beneficial in the majority of cases, there are some small studies that suggest it may not be safe to take close to the time of giving birth, or in people with a history of pregnancy loss, or unusual vaginal bleeding, or clotting disorders.
See specifically: Ginger for nausea and vomiting of pregnancy
As a side note on the topic of “trouble down there”, ginger has also been found to be as effective as Novafen (a combination drug of acetaminophen (Tylenol), caffeine, and ibuprofen), in the task of relieving menstrual pain:
See: Effect of Ginger and Novafen on menstrual pain: A cross-over trial
Against inflammation & pain
Ginger has well-established anti-inflammatory (and, incidentally, which affects many of the same systems, antioxidant) effects. Let’s take a look at that first:
Read: Effect of Ginger on Inflammatory Diseases
Attentive readers will note that this means that ginger is not merely some nebulous anti-inflammatory agent. Rather, it also specifically helps alleviate delineable inflammatory diseases, ranging from colitis to Crohn’s, arthritis to lupus.
We’ll be honest (we always are!), the benefits in this case are not necessarily life-changing, but they are a statistically significant improvement, and if you are living with one of those conditions, chances are you’ll be glad of even things described in scientific literature as “modestly efficacious”.
What does “modestly efficacious” look like? Here are the numbers from a review of 593 patients’ results in clinical trials (against placebo):
❝Following ginger intake, a statistically significant pain reduction SMD = −0.30 ([95% CI: [(−0.50, −0.09)], P = 0.005]) with a low degree of inconsistency among trials (I2 = 27%), and a statistically significant reduction in disability SMD = −0.22 ([95% CI: ([−0.39, −0.04)]; P = 0.01; I2 = 0%]) were seen, both in favor of ginger.❞
To de-mathify that:
- Ginger reduced pain by 30%
- Ginger reduced disability by 22%
Read the source: Efficacy and safety of ginger in osteoarthritis patients: a meta-analysis of randomized placebo-controlled trials
Because (in part) of the same signalling pathways, it also has benefits against cancer (and you’ll remember, it also reduces the symptoms of chemotherapy).
See for example: Ginger’s Role in Prevention and Treatment of Gastrointestinal Cancer
For cardiovascular health
In this case, its benefits are mostly twofold:
- It significantly reduces triglycerides and LDL cholesterol, while increasing HDL cholesterol
- It significantly reduces fasting blood sugar levels and HbA1c levels (both risk factors for CVD)
Against neurodegeneration
This is in large part because it reduces inflammation, which we discussed earlier.
But, not everything passes the blood-brain barrier, so it’s worth noting when something (like gingerol) does also have an effect on brain health as well as the rest of the body.
You do not want inflammation in your brain; that is Bad™ and strongly associated with Alzheimer’s and Parkinson’s.
As well as reducing neuroinflammation, ginger has other relevant mechanisms too:
❝Its bioactive compounds may improve neurological symptoms and pathological conditions by modulating cell death or cell survival signaling molecules.
The cognitive enhancing effects of ginger might be partly explained via alteration of both the monoamine and the cholinergic systems in various brain areas.
Moreover, ginger decreases the production of inflammatory related factors❞
Check it out in full, as this is quite interesting:
Role of Ginger in the Prevention of Neurodegenerative Diseases
How much to take?
In most studies, doses of 1–3 grams/day were used.
Where to get it?
Your local supermarket, as a first port-of-call. Especially given the dose you want, it may be nicer for you to have a touch of sliced ginger root in your cooking, rather than taking 2–6 capsules per day to get the same dose.
Obviously, this depends on your culinary preferences, and ginger certainly doesn’t go with everything!
If you do want it as a supplement, here is an example product on Amazon, for your convenience.
Enjoy!
Share This Post
-
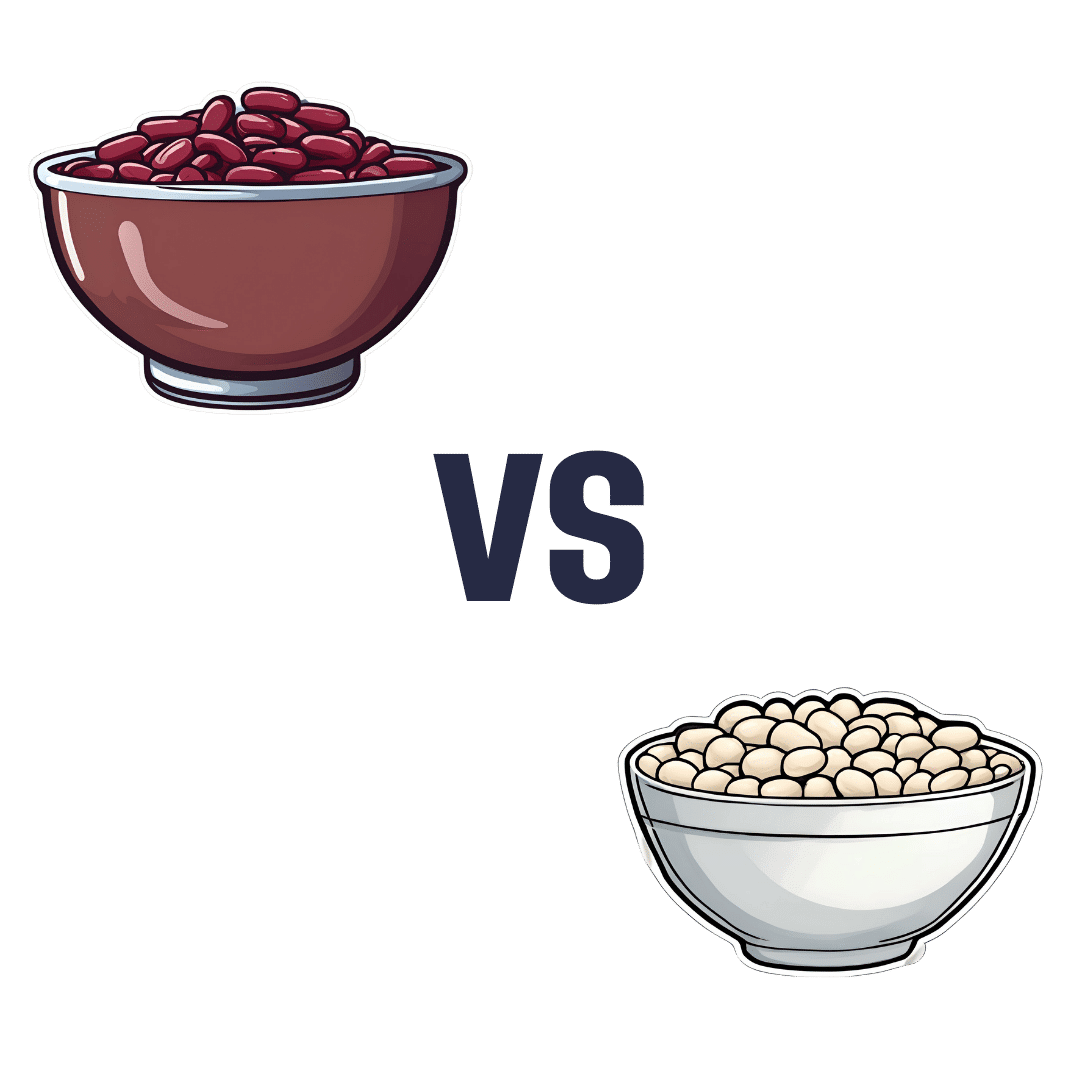
Kidney Beans vs White Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kidney beans to white beans, we picked the white.
Why?
It was close, and each has its strengths! Bear in mind, these are very closely-related beans. But as we say, there are distinguishing factors…
In terms of macros, kidney beans have very slightly more fiber and white beans have very slightly more protein. But both are close enough in both of those things to call this a tie in this category.
When it comes to vitamins, there are two ways of looking at this:
- kidney beans have more of vitamins B1, B2, B3, B6, B9, C, and K, while white beans have more vitamin B5, E, and choline
- kidney beans have slightly more of some vitamins that don’t usually see a deficiency, while white beans have 31x more vitamin E
Nevertheless, we’re sticking by our usual method of noting that this is a 7:3 win for kidney beans in this category; we just wanted to note that in practical health terms, an argument can be made for white beans on the vitamin front too.
In the category of minerals, kidney beans have slightly more phosphorus, while white beans have more calcium, copper, iron, magnesium, manganese, potassium, selenium, and zinc. An easy win for white beans this time.
(In case you’re wondering about the margin on phosphorus, it was 0.2x more, so we’re not seeing a situation like white beans’ 31x more vitamin E)
In short: both are great and both have their strengths. Enjoy both, together if you like! But if we have to pick one, we’re going with white beans.
Want to learn more?
You might like to read:
Take care!
Share This Post
-
Breaking The Age Code – by Dr. Becca Levy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a social psychologist, sets out to not only bust ageist expectations, but also boost life expectancy by 7.5 years.
How? By examining the extent to which how we think about our age affects our actual aging. Lest this sound wishy-washy, there are 52 pages of scientific references at the back.
We’ve written about this before at 10almonds, for example about the famous “Counterclockwise” study that saw reversals in biological markers of aging after a one-week intervention that consisted only of a (albeit rather intensive) mental reframe with regard to their age.
This book goes into such ideas much more than we can in a single article here, and in more ways, both on the personal level and the societal level.
The style is (despite its heavy leanings on hundreds of scientific studies) quite conversational in tone, with many personal anecdotes padding the pages a little, but it does get the message across and helps to illustrate things.
Bottom line: if you’d like a fresh take on aging, to make a big difference to yours, this book tackles that.
Click here to check out Breaking The Age Code, and break the age code!
Share This Post
Related Posts
-
Reishi Mushrooms: Which Benefits Do They Really Have?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reishi Mushrooms
Another Monday Research Review, another mushroom! If we keep this up, we’ll have to rename it “Mushroom Monday”.
But, there’s so much room for things to say, and these are fun guys to write about, as we check the science for any spore’ious claims…
Why do people take reishi?
Popular health claims for the reishi mushroom include:
- Immune health
- Cardiovascular health
- Protection against cancer
- Antioxidant qualities
- Reduced fatigue and anxiety
And does the science agree?
Let’s take a look, claim by claim:
Immune health
A lot of research for this has been in vitro (ie, with cell cultures in labs), but promising, for example:
Immunomodulating Effect of Ganoderma lucidum (Lingzhi) and Possible Mechanism
(that is the botanical name for reishi, and the Chinese name for it, by the way)
That’s not to say there are no human studies though; here it was found to boost T-cell production in stressed athletes:
Cardiovascular health
Here we found a stack of evidence for statistically insignificant improvements in assorted measures of cardiovascular health, and some studies where reishi did not outperform placebo.
Because the studies were really not that compelling, instead of taking up room (and your time) with them, we’re going to move onto more compelling, exciting science, such as…
Protection against cancer
There’s a lot of high quality research for this, and a lot of good results. The body of evidence here is so large that even back as far as 2005, the question was no longer “does it work” or even “how does it work”, but rather “we need more clinical studies to find the best doses”. Researchers even added:
❝At present, lingzhi is a health food supplement to support cancer patients, yet the evidence supporting the potential of direct in vivo anticancer effects should not be underestimated.❞
Check it out:
Anticancer effects of Ganoderma lucidum: a review of scientific evidence
Just so you know we’re not kidding about the weight of evidence, let’s drop a few extra sources:
- Ganoderma lucidum: a rational pharmacological approach to surmount cancer
- Ganoderma lucidum as an anti-cancer agent
- Extract from Ganoderma lucidum suppresses cervical cancer cell malignancy
- Ganoderma lucidum spore oil induces apoptosis of breast cancer cells
- Ganoderma lucidum enhances carboplatin chemotherapy effect
- Ganoderma lucidum inhibits prostate cancer cell migration
- Ganoderma lucidum fruiting body extracts inhibit colorectal cancer
- Inhibitory activity of medicinal mushroom Ganoderma lucidum on colorectal cancer
- Ganoderma lucidum (reishi mushroom) for cancer treatment
By the way, we shortened most of those titles for brevity, but almost all of the continued with “by” followed by a one-liner of how it does it.
So it’s not a “mysterious action” thing, it’s a “this is a very potent medicine and we know how it works” thing.
Antioxidant qualities
Here we literally only found studies to say no change was found, one that found a slight increase of antioxidant levels in urine. It’s worth noting that levels of a given thing (or its metabolites, in the case of some things) in urine are often quite unhelpful regards knowing what’s going on in the body, because we get to measure only what the body lost, not what it gained/kept.
So again, let’s press on:
Reduced fatigue and anxiety
Most of the studies for this that we could find pertained to health-related quality of life for cancer patients specifically, so (while they universally give glowing reports of reishi’s benefits to health and happiness of cancer patients), that’s a confounding factor when it comes to isolating its effects on reduction of fatigue and anxiety in people without cancer.
Here’s one that looked at it in the case of reduction of fatigue, anxiety, and other factors, in patients without cancer (but with neurathenia), in which they found it was “significantly superior to placebo with respect to the clinical improvement of symptoms”.
Summary:
- Reishi mushroom’s anti-cancer properties are very, very clear
- There is also good science to back immune health claims
- It also has been found to significantly reduce fatigue and anxiety in unwell patients (we’d love to see more studies on its benefits in otherwise healthy people, though)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Long-Covid Patients Are Frustrated That Federal Research Hasn’t Found New Treatments
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Erica Hayes, 40, has not felt healthy since November 2020 when she first fell ill with covid.
Hayes is too sick to work, so she has spent much of the last four years sitting on her beige couch, often curled up under an electric blanket.
“My blood flow now sucks, so my hands and my feet are freezing. Even if I’m sweating, my toes are cold,” said Hayes, who lives in Western Pennsylvania. She misses feeling well enough to play with her 9-year-old son or attend her 17-year-old son’s baseball games.
Along with claiming the lives of 1.2 million Americans, the covid-19 pandemic has been described as a mass disabling event. Hayes is one of millions of Americans who suffer from long covid. Depending on the patient, the condition can rob someone of energy, scramble the autonomic nervous system, or fog their memory, among many other http://symptoms.in/ addition to the brain fog and chronic fatigue, Hayes’ constellation of symptoms includes frequent hives and migraines. Also, her tongue is constantly swollen and dry.
“I’ve had multiple doctors look at it and tell me they don’t know what’s going on,” Hayes said about her tongue.
Estimates of prevalence range considerably, depending on how researchers define long covid in a given study, but the Centers for Disease Control and Prevention puts it at 17 million adults.
Despite long covid’s vast reach, the federal government’s investment in researching the disease — to the tune of $1.15 billion as of December — has so far failed to bring any new treatments to market.
This disappoints and angers the patient community, who say the National Institutes of Health should focus on ways to stop their suffering instead of simply trying to understand why they’re suffering.
“It’s unconscionable that more than four years since this began, we still don’t have one FDA-approved drug,” said Meighan Stone, executive director of the Long COVID Campaign, a patient-led advocacy organization. Stone was among several people with long covid who spoke at a workshop hosted by the NIH in September where patients, clinicians, and researchers discussed their priorities and frustrations around the agency’s approach to long-covid research.
Some doctors and researchers are also critical of the agency’s research initiative, called RECOVER, or Researching COVID to Enhance Recovery. Without clinical trials, physicians specializing in treating long covid must rely on hunches to guide their clinical decisions, said Ziyad Al-Aly, chief of research and development with the VA St Louis Healthcare System.
“What [RECOVER] lacks, really, is clarity of vision and clarity of purpose,” said Al-Aly, saying he agrees that the NIH has had enough time and money to produce more meaningful progress.
Now the NIH is starting to determine how to allocate an additional $662 million of funding for long-covid research, $300 million of which is earmarked for clinical trials. These funds will be allocated over the next four http://years.at/ the end of October, RECOVER issued a request for clinical trial ideas that look at potential therapies, including medications, saying its goal is “to work rapidly, collaboratively, and transparently to advance treatments for Long COVID.”
This turn suggests the NIH has begun to respond to patients. This has stirred cautious optimism among those who say that the agency’s approach to long covid has lacked urgency in the search for effective treatments.Stone calls this $300 million a down payment. She warns it’s going to take a lot more money to help people like Hayes regain some degree of health.“There really is a burden to make up this lost time now,” Stone said.
The NIH told KFF Health News and NPR via email that it recognizes the urgency in finding treatments. But to do that, there needs to be an understanding of the biological mechanisms that are making people sick, which is difficult to do with post-infectious conditions.
That’s why it has funded research into how long covid affects lung function, or trying to understand why only some people are afflicted with the condition.
Good Science Takes Time
In December 2020, Congress appropriated $1.15 billion for the NIH to launch RECOVER, raising hopes in the long-covid patient community.
Then-NIH Director Francis Collins explained that RECOVER’s goal was to better understand long covid as a disease and that clinical trials of potential treatments would come later.
According to RECOVER’s website, it has funded eight clinical trials to test the safety and effectiveness of an experimental treatment or intervention. Just one of those trials has published results.
On the other hand, RECOVER has supported more than 200 observational studies, such as research on how long covid affects pulmonary function and on which symptoms are most common. And the initiative has funded more than 40 pathobiology studies, which focus on the basic cellular and molecular mechanisms of long covid.
RECOVER’s website says this research has led to crucial insights on the risk factors for developing long covid and on understanding how the disease interacts with preexisting conditions.
It notes that observational studies are important in helping scientists to design and launch evidence-based clinical trials.
Good science takes time, said Leora Horwitz, the co-principal investigator for the RECOVER-Adult Observational Cohort at New York University. And long covid is an “exceedingly complicated” illness that appears to affect nearly every organ system, she said.
This makes it more difficult to study than many other diseases. Because long covid harms the body in so many ways, with widely variable symptoms, it’s harder to identify precise targets for treatment.
“I also will remind you that we’re only three, four years into this pandemic for most people,” Horwitz said. “We’ve been spending much more money than this, yearly, for 30, 40 years on other conditions.”
NYU received nearly $470 million of RECOVER funds in 2021, which the institution is using to spearhead the collection of data and biospecimens from up to 40,000 patients. Horwitz said nearly 30,000 are enrolled so far.
This vast repository, Horwitz said, supports ongoing observational research, allowing scientists to understand what is happening biologically to people who don’t recover after an initial infection — and that will help determine which clinical trials for treatments are worth undertaking.
“Simply trying treatments because they are available without any evidence about whether or why they may be effective reduces the likelihood of successful trials and may put patients at risk of harm,” she said.
Delayed Hopes or Incremental Progress?
The NIH told KFF Health News and NPR that patients and caregivers have been central to RECOVER from the beginning, “playing critical roles in designing studies and clinical trials, responding to surveys, serving on governance and publication groups, and guiding the initiative.”But the consensus from patient advocacy groups is that RECOVER should have done more to prioritize clinical trials from the outset. Patients also say RECOVER leadership ignored their priorities and experiences when determining which studies to fund.
RECOVER has scored some gains, said JD Davids, co-director of Long COVID Justice. This includes findings on differences in long covid between adults and kids.But Davids said the NIH shouldn’t have named the initiative “RECOVER,” since it wasn’t designed as a streamlined effort to develop treatments.
“The name’s a little cruel and misleading,” he said.
RECOVER’s initial allocation of $1.15 billion probably wasn’t enough to develop a new medication to treat long covid, said Ezekiel J. Emanuel, co-director of the University of Pennsylvania’s Healthcare Transformation Institute.
But, he said, the results of preliminary clinical trials could have spurred pharmaceutical companies to fund more studies on drug development and test how existing drugs influence a patient’s immune response.
Emanuel is one of the authors of a March 2022 covid roadmap report. He notes that RECOVER’s lack of focus on new treatments was a problem. “Only 15% of the budget is for clinical studies. That is a failure in itself — a failure of having the right priorities,” he told KFF Health News and NPR via email.
And though the NYU biobank has been impactful, Emanuel said there needs to be more focus on how existing drugs influence immune response.
He said some clinical trials that RECOVER has funded are “ridiculous,” because they’ve focused on symptom amelioration, for example to study the benefits of over-the-counter medication to improve sleep. Other studies looked at non-pharmacological interventions, such as exercise and “brain training” to help with cognitive fog.
People with long covid say this type of clinical research contributes to what many describe as the “gaslighting” they experience from doctors, who sometimes blame a patient’s symptoms on anxiety or depression, rather than acknowledging long covid as a real illness with a physiological basis.
“I’m just disgusted,” said long-covid patient Hayes. “You wouldn’t tell somebody with diabetes to breathe through it.”
Chimére L. Sweeney, director and founder of the Black Long Covid Experience, said she’s even taken breaks from seeking treatment after getting fed up with being told that her symptoms were due to her diet or mental health.
“You’re at the whim of somebody who may not even understand the spectrum of long covid,” Sweeney said.
Insurance Battles Over Experimental Treatments
Since there are still no long-covid treatments approved by the Food and Drug Administration, anything a physician prescribes is classified as either experimental — for unproven treatments — or an off-label use of a drug approved for other conditions. This means patients can struggle to get insurance to cover prescriptions.
Michael Brode, medical director for UT Health Austin’s Post-COVID-19 Program — said he writes many appeal letters. And some people pay for their own treatment.
For example, intravenous immunoglobulin therapy, low-dose naltrexone, and hyperbaric oxygen therapy are all promising treatments, he said.
For hyperbaric oxygen, two small, randomized controlled studies show improvements for the chronic fatigue and brain fog that often plague long-covid patients. The theory is that higher oxygen concentration and increased air pressure can help heal tissues that were damaged during a covid infection.
However, the out-of-pocket cost for a series of sessions in a hyperbaric chamber can run as much as $8,000, Brode said.
“Am I going to look a patient in the eye and say, ‘You need to spend that money for an unproven treatment’?” he said. “I don’t want to hype up a treatment that is still experimental. But I also don’t want to hide it.”
There’s a host of pharmaceuticals that have promising off-label uses for long covid, said microbiologist Amy Proal, president and chief scientific officer at the Massachusetts-based PolyBio Research Foundation. For instance, she’s collaborating on a clinical study that repurposes two HIV drugs to treat long covid.
Proal said research on treatments can move forward based on what’s already understood about the disease. For instance, she said that scientists have evidence — partly due to RECOVER research — that some patients continue to harbor small amounts of viral material after a covid infection. She has not received RECOVER funds but is researching antivirals.
But to vet a range of possible treatments for the millions suffering now — and to develop new drugs specifically targeting long covid — clinical trials are needed. And that requires money.
Hayes said she would definitely volunteer for an experimental drug trial. For now, though, “in order to not be absolutely miserable,” she said she focuses on what she can do, like having dinner with her http://family.at/ the same time, Hayes doesn’t want to spend the rest of her life on a beige couch.
RECOVER’s deadline to submit research proposals for potential long-covid treatments is Feb. 1.
This article is from a partnership that includes NPR and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Nature Provides Us With A Surprisingly Powerful Painkiller
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s well-known (at least to regular 10almonds-readers) that seeing nature, ideally green leaves and blue sky, improves our mood by stimulating production of serotonin.
See also: Neurotransmitter Cheatsheet
But it does a lot more.
Reducing the actual signals of pain
Researchers at the University of Vienna have discovered that viewing nature scenes (even if just on video) alleviates physical pain—not just in self-reported subjective assessments, but also by a reduction of the neural activity that signals pain:
❝Pain is like a puzzle, made up of different pieces that are processed differently in the brain. Some pieces of the puzzle relate to our emotional response to pain, such as how unpleasant we find it. Other pieces correspond to the physical signals underlying the painful experience, such as its location in the body and its intensity.
Unlike placebos, which usually change our emotional response to pain, viewing nature changed how the brain processed early, raw sensory signals of pain.
Thus, the effect appears to be less influenced by participants’ expectations, and more by changes in the underlying pain signals❞
This was tested against, varyingly, viewing an urban environment or viewing an indoor environment, neither of which gave the same benefits.
The setup of the experiment is relevant, so…
Matching soundscape accompanied each visual stimulus. The three pain runs had a total duration of 9 min each, during which one environment was accompanied by 16 painful and 16 non-painful shocks. Neuroimaging was used for all parts, and participants were exposed to all environments:
- First, a cue indicating the intensity of the next shock (red = painful, yellow = not painful) was presented for 2000 milliseconds (ms).
- Second, a variable interval of 3500 ± 1500 ms was shown.
- Third, a cue indicating the intensity of the shock was presented for 1000 ms, accompanied by an electrical shock with a duration of 500 ms.
- Fourth, a variable interval of 3500 ± 1500 ms followed.
- Fifth, after each third trial, participants rated the shock’s intensity and unpleasantness at 6000 ms each.
- Sixth, each trial ended with an intertrial interval (ITI) presented for 2000 ms.
They found that as well as the self-assessment reports being as expected (nature scenes reduced subjective experience of pain),
❝In summary, the multivoxel and region of interest analyses converged in showing that pain responses when exposed to nature as compared to urban or indoor stimuli were associated with a decrease in neural processes related to lower-level nociception-related features (NPS, thalamus), as well as in regions of descending modulatory circuitry associated with attentional alterations of pain that also encode sensory-discriminative aspects (S2, pINS).❞
In other words—to the extent that pain can be quantified objectively by neural imaging—the pain was also objectively reduced, much like with a chemical painkiller.
You can read the paper in full, here:
Nature exposure induces analgesic effects by acting on nociception-related neural processing
How to benefit from this
Well, first there is the obvious, “view nature“.
However, note the timescales involved in the testing periods: 2000 milliseconds is two seconds, and that was the intertrial interval used—the equivalent of a washout phase in an interventional trial (but a drug/supplement/diet washout is usually a number of weeks).
The fact that the test periods were a matter of seconds, and the intertrial period was also literally two seconds, this means:
It works quickly, and the effect disappears quickly, too.
In other words: if you want pain relief from nature, the good news is you can get it immediately while viewing nature, and the bad news is that you have to keep viewing nature to continue enjoying the painkilling effect.
So that’s a limitation, but it’s still clearly a very worthy option for a little respite from chronic pain now and again, for example.
Want to learn more?
We’ve written quite a bit about pain management, including:
- Before You Reach For That Tylenol…
- How To Stop Pain Spreading
- How To Dial Down Your Pain
- Managing Chronic Pain (Realistically!)
- Get The Right Help For Your Pain
- The 7 Approaches To Pain Management
- Science-Based Alternative Pain Relief (When Painkillers Aren’t Helping, These Things Might)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: