Oats vs Pearl Barley – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing oats to pearl barley, we picked the oats.
Why?
In terms of macronutrients first, pearl barley has about three times the carbs for only the same amount of protein and fiber—if it had been regular barley rather than pearl parley, it’d have about twice the fiber, but pearl barley has had the fibrous husk removed.
Vitamins really set the two part, though: oats have a lot more (60x more) vitamin A, and notably more of vitamins B1, B2, B3, B5, B6, and B9, as well as 6x more vitamin E. In contrast, pearl barley has a little more vitamin K and choline. An easy win for oats in this section.
In the category of minerals, oats have over 6x more calcium, 3x more iron, and a little more magnesium, manganese, and phosphorus. Meanwhile, pearl barley boats a little more copper, potassium, selenium, and zinc. So, a more moderate win for oats in this category.
They are both very good for the gut, unless you have a gluten intolerance/allergy, in which case, oats are the only answer here since pearl barley, as per barley in general, has gluten as its main protein (oats, meanwhile, do not contain gluten, unless by cross-contamination).
Adding up all the sections, this one’s a clear win for oats.
Want to learn more?
You might like to read:
- Eat More (Of This) For Lower Blood Pressure
- Making Friends With Your Gut (You Can Thank Us Later)
- Gluten: What’s The Truth?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fruit & Veg In The Fridge: Pros & Cons
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝What effect does refrigeration have on the nutritional value of fruit and vegetables??❞
It’s difficult to give a single definitive answer, because naturally there are a lot of different fruits and vegetables, and a lot of different climates. The answer may be different for tomatoes in Alaska vs bananas in Arizona!
However, we can still generalize at least somewhat
Refrigeration will generally slow down any degradation process, and in the case of fruit and vegetables, that can mean slowing down their “ripening” too, as applicable.
However…
Refrigeration will also impede helpful bioactivity too, and that includes quite a list of things.
Here’s a good study that’s quite illustrative; we’d summarize the conclusions but the rather long title already does that nicely:
So, this really is a case of “there are pros and cons, but probably more cons on balance”.
In practical terms, a good take-away from this can be twofold:
- don’t keep fruit and veg in the fridge unless the ambient temperature really requires it
- if the ambient temperature does require it, it’s best to get the produce in fresh each day if that’s feasible, to minimize time spent in the fridge
An extra thing not included there: often when it comes to the spoilage of fruit and veg, the problem is that it respires and oxidizes; reducing the temperature does lower the rate of those, but often a far better way is to remove the oxygen. So for example, if you get carried away and chop too many carrot batons for your hummus night, then putting them in a sealed container can go a long way to keeping them fresh.
See also: How Does the Nutritional Value of Fruits and Vegetables Change Over Time?
Enjoy!
Share This Post
-
Food for Thought – by Lorraine Perretta
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What are “brain foods”? If you think for a moment, you can probably list a few. What this book does is better.
As well as providing the promised 50 recipes (which themselves are varied, good, and easy), Perretta explains the science of very many brain-healthy ingredients. Not just that, but also the science of a lot of brain-unhealthy ingredients. In the latter case, probably things you already knew to stay away from, but still, it’s a good reminder of one more reason why.
Nor does she merely sort things into brain-healthy (or brain-unhealthy, or brain-neutral), but rather she gives lists of “this for memory” and “this against depression” and “this for cognition” and “this against stress” and so forth.
Perhaps the greatest value of this book is in that; her clear explanations with science that’s simplified but not dumbed down. The recipes are definitely great too, though!
Bottom line: if you’d like to eat more for brain health, this book will give you many ways of doing so
Click here to check out Food for Thought, and upgrade your recipes!
Share This Post
-
Which Gadgets Help, & Which Are A Waste Of Time?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I’m a 67- year old yoga teacher and runner. A lifelong runner, I started long distance running when I was 58. One of my friends loves rucking? I recently bought a rucking vest. Your thoughts? Any risks?
As a perk of my yoga instructor job I get cryotherapy, red light therapy, infrared sauna, and Normatec boots for a nominal fee. Even though they are almost free, I don’t take advantage of them as I can’t find evidence of their value and don’t want to waste my time. Do you recommend any of them?❞On rucking and rucking vests
First, for any unfamiliar, this is about walking/running/exercising in general, with a weighted backpack or weight vest.
As for whether this is beneficial, it depends on your goals. Once upon a very long time ago when this writer was a soldier, it was vitally important to for me be able to [fall from the sky and then] run about 2km carrying a certain (hefty) amount of weight and still be able to fight at the other end of it, or else I would die. Thus, between deployments, I’d often carry a sturdy rucksack with concrete slabs in it, to keep myself accustomed to that burden (funny story: someone once tried to steal that when I had put it down while doing something—the would-be thief fell over instantly and then ran away empty-handed). And, here’s the thing: this kind of training did for me what I needed it to do for me. As a 67-year-old yoga teacher, your needs are probably very different.
A common reason to use weight vests is in an effort against osteoporosis, but the evidence is lacking (or very weak, at best), as we wrote about a while back:
Weight Vests Against Osteoporosis: Do They Really Build Bone?
With regard to risks… Let’s put it this way: my old regiment, in addition to the usual soldierly problems like hearing damage and PTSD, has quite a reputation for producing veterans with spinal compression injuries. And that’s entirely because of the whole “running with a large amount of weight strapped to us” thing. So, you probably don’t want that.
If you are going to do that though, then:
- a weight best is a lot better than a backpack (better distribution of weight)
- start with low weight and work up, and don’t push your limits
We’re not the boss of you, so by all means do as you see fit, but unless there’s a special reason why being able to run with a heavy weight is important to you, then running with a light weight is already more than good enough.
About those job perks
Again, of course, it depends on what you hope to get out of them, but in some cases there is a lot of evidence for benefit.
On cryotherapy: Ice Baths: To Dip Or Not To Dip? ← there are definite benefits for most people!
On red light therapy: Red Light, Go! Casting Yourself In A Healthier Light ← there are some caveats re people who should not do this or at least should be very wary, but for most people, this does a lot of good, and is very well-evidenced to be beneficial
On infrared saunas: we’re unaware of any special evidence in favor of these. However, traditional saunas have plenty of well-evidenced benefits: Saunas: Health Benefits (& Caveats)
On Normatec boots: for the unfamiliar, this is a brand name for compression technology. Again, it depends on what you want to get out of it, though. If you are in good health, then what it’s generally being advertised for is to prevent/reduce exercise-induced muscle damage caused by the stress that endurance training can place on skeletal muscle. Just one problem—it doesn’t seem to work:
❝Athletes attempt to aid their recovery in various ways, one of which is through compression. Dynamic compression consists of intermittent pneumatic compression (IPC) devices, such as the NormaTec Recovery System and Recovery Pump
Clinical Question: What are the effects of IPC on the reduction of Exercise-Induced Muscle Damage (EIMD) in endurance athletes following prolonged exercise? Summary of Key Findings: The current literature was searched to identify the effects of IPC, and 3 studies were selected: 2 randomized controlled trials and 1 randomized cross-over study. Two studies investigated the effect of IPC on delayed onset muscle soreness and plasma creatine kinase in ultramarathoners. The other looked at the impact of IPC on delayed onset muscle soreness in marathoners, ultramarathoners, triathletes, and cyclists.
All studies concluded IPC was not an effective means of improving the reduction of EIMD in endurance-trained athletes.❞
However! If you have lipedema and/or lymphedema and want to manage that, then compression gear may help:
Take care!
Share This Post
Related Posts
-
Low-Dose Aspirin & Anemia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We recently wrote about…
How To Survive A Heart Attack When You’re Alone
…and one of the items was “if you have aspirin readily available, then after calling an ambulance is the time to take it—but don’t exert yourself trying to find some”.
But what of aspirin as a preventative?
Many people take low-dose aspirin daily as a way to reduce the risk of atherothrombosis specifically (and thus, indirectly, they hope to reduce the risk of heart attacks).
The science of how helpful this is both clear and complicated—that is to say, the stats are not ambiguous*, but there are complicating factors of which many people are unaware.
*it will reduce the overall risk of cardiovascular events, but will not affect CVD mortality; in other words, it may improve your recovery from minor cardiac events, but is not likely to save you from major ones.
And also, it has unwanted side effects that can constitute a more relevant threat for many people. We’ll share more on that at the end of today’s article, but first…
A newly identified threat from daily aspirin use
A large (n=313,508) study of older adults (median age 73) were sorted into those who used low-dose aspirin as a preventative, and those who did not.
The primary outcome was incidence of anemia sufficient to require treatment, and the secondary outcome was major bleeding. And, at least 1 in 5 of those who experienced anemia also experienced bleeding.
The bleeding issue was not “newly identified” and will not surprise many people; after all, the very reason that aspirin is taken as a CVD preventative is for its anti-clotting property of allowing blood to flow more freely.
The anemia, however, has been getting increasing scientific scrutiny lately, after long going unnoticed in the wild. Given that anemia also gives the symptom “dizziness”, this is also a significant threat for increasing the incidence of falls in the older population, too, which can of course lead to serious complications and ultimately death.
Here’s the paper itself:
Want to know more?
As promised, here’s what we wrote previously about some of aspirin’s other risks:
Aspirin, CVD Risk, & Potential Counter-Risks
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lucid Dreaming – by Stephen LaBerge Ph.D.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For any unfamiliar: lucid dreaming means being aware that one is dreaming, while dreaming, and exercising a degree of control over the dream. Superficially, this is fun. But if one really wants to go deeper into it, it can be a lot more:
Dr. Stephen LaBerge takes a science-based approach to lucid dreaming, and in this work provides not only step-by-step instructions of several ways of inducing lucid dreaming, but also, opens the reader’s mind to things that can be done there beyond the merely recreational:
In lucid dreams, he argues and illustrates, it’s possible to talk to parts of one’s own subconscious (Inception, anyone? Yes, this book came first) and get quite an amount of self-therapy done. And that hobby you wish you had more time to practice? The possibilities just became limitless. And who wouldn’t want that?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
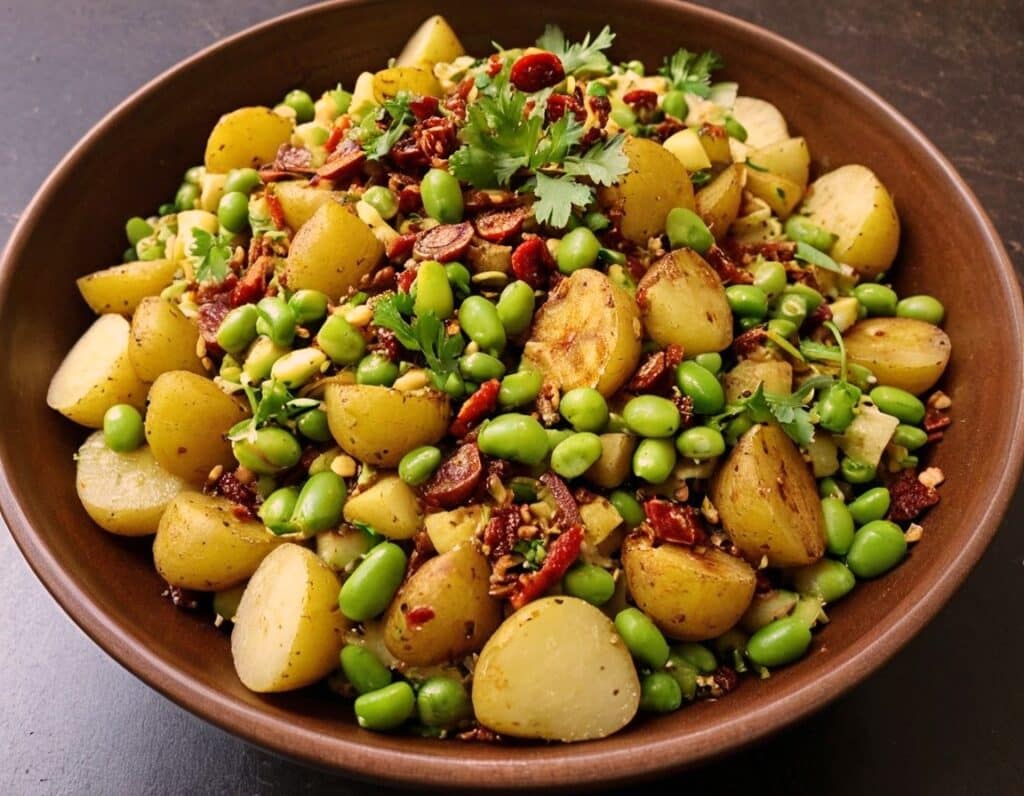
Chaat Masala Spiced Potato Salad With Beans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is an especially gut-healthy dish; the cooked-and-cooled potatoes are not rich with resistant starches (that’s good), the beans bring protein (as well as more fiber and micronutrients), and many of the spices bring their own benefits. A flavorful addition to your table!
You will need
- 1 lb new potatoes, boiled or steamed, with skin on, quartered, cooled ← this is a bit of a “mini recipe”, but we expect you can handle it
- 5 oz blanched broad beans
- 2 oz sun-dried tomatoes, chopped
- ¼ bulb garlic, crushed
- 1 tbsp extra virgin olive oil
- 2 tsp amchoor
- 2 tsp ground cumin
- 2 tsp ground coriander
- 1 tsp ground ginger
- 1 tsp ground asafoetida
- 1 tsp black pepper, coarse ground
- 1 tsp red chili powder
- 1 tsp ground turmeric
- ½ tsp MSG or 1 tsp low-sodium salt
- Juice of ½ lemon
And then…
- To garnish: finely chopped cilantro, or if you have the “cilantro tastes like soap” gene, then substitute with parsley
- To serve: a nice chutney; you can use our Spiced Fruit & Nut Chutney recipe
Method
(we suggest you read everything at least once before doing anything)
1) Mix all the ingredients from the main section, ensuring an even distribution on the spices.
2) Add the garnish, and serve with the chutney. That’s it. There was more work in the prep (and potentially, finding all the ingredients) today.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we scored all five today!
- Lycopene’s Benefits For The Gut, Heart, Brain, & More ← don’t underestimate those sun-dried tomatoes, either!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: