When You Know What You “Should” Do (But Knowing Isn’t The Problem)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When knowing what to do isn’t the problem
Often, we know what we need to do. Sometimes, knowing isn’t the problem!
The topic today is going to be a technique used by therapeutic service providers to help people to enact positive changes in their lives.
While this is a necessarily dialectic practice (i.e., it involves a back-and-forth dialogue), it’s still perfectly possible to do it alone, and that’s what we’ll be focussing on in this main feature.
What is Motivational Interviewing?
❝Motivational interviewing (MI) is a technique that has been specifically developed to help motivate ambivalent patients to change their behavior.❞
Read in full: Motivational Interviewing: An Evidence-Based Approach for Use in Medical Practice
It’s mostly used for such things as helping people reduce or eliminate substance abuse, or manage their weight, or exercise more, things like that.
However, it can be employed for any endeavour that requires motivation and sustained willpower to carry it through.
Three Phases
Motivational Interviewing traditionally has three phases:
- Exploring and understanding the issue at hand
- Guiding and deciding importance and goals
- Choosing and setting an action plan
In self-practice, maybe you can already know and understand what it is that you want/need to change.
If not, consider asking yourself such questions as:
- What does a good day look like? What does a bad day look like?
- If things are not good now, when were they good? What changed?
- If everything were perfect now, what would that look like? How would you know?
Once you have a clear idea of where you want to be, the next thing to know is: how much do you want it? And how confident are you in attaining it?
This is a critical process:
- Give your answers numerically on a scale from 0 to 10
- Whatever your score, ask yourself why it’s not lower. For example, if you scored your motivation 4 and your confidence 2, what factors made your motivation not a lower number? What factors made your confidence not a lower number?
- In the unlikely event that you gave yourself a 0, ask whether you can really afford to scrap the goal. If you can’t, find something, anything, to bring it to at least a 1.
- After you’ve done that, then you can ask yourself the more obvious question of why your numbers aren’t higher. This will help you identify barriers to overcome.
Now you’re ready to choose what to focus on and how to do it. Don’t bite off more than you can chew; it’s fine to start low and work up. You should revisit this regularly, just like you would if you had a counsellor helping you.
Some things to ask yourself at this stage of the motivational self-interviewing:
- What’s a good SMART goal to get you started?
- What could stop you from achieving your goal?
- How could you overcome that challenge?
- What is your backup plan, if you have to scale back your goal for some reason?
A conceptual example: if your goal is to stick to a whole foods Mediterranean diet, but you are attending a wedding next week, then now is the time to decide in advance 1) what personal lines-in-the-sand you will or will not draw 2) what secondary, backup plan you will make to not go too far off track.
The same example in practice: wedding menus often offer meat/fish/vegetarian options, so you might choose the fish or vegetarian, and as for sugar and alcohol, you might limit yourself to “a small slice of wedding cake only; coffee/cheese option instead of dessert”, and “alcohol only for toasts”.
Giving yourself the permission well in advance for small (clearly defined and boundaried!) diversions from the plan, will stop you from falling into the trap of “well, since today’s a cheat-day now…”
Secret fourth stage
The secret here is to keep going back and reassessing at regular intervals. Set your own calendar; you might want to start out weekly and then move to monthly when you’re more strongly on-track.
For this reason, it’s good to keep a journal with your notes from your self-interview sessions, the scores you gave yourself, the goals and plans you set, etc.
When conducting your regular review, be sure to examine what worked for you, and what didn’t (and why). That way, you can practice trial-and-improvement as you go.
Want to learn more?
We only have so much room here, but there are lots of resources out there.
Here’s a high-quality page that:
- explains motivational interviewing in more depth than we have room for here
- offers a lot of free downloadable resource packs and the like
Check it out: Motivational Interviewing Theory & Resources
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Common Sense Labs: Blood Labs Demystified – by Dr. Ken Berry & Kim Howerton
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most people, if given their test results as a set of numbers, will have no idea what they mean.
And a doctor or nurse saying “this is good”, “this is a bit low”, “this is very high” etc isn’t that much more informative, as it doesn’t really give a true feel for the information.
Dr. Berry produced this book to bridge that knowledge gap, and in his words, “put the power of health back in the hands of the people”. The book also covers what blood tests to recommend annually (finding common recommendations insufficient), and how to go about asking for those if your doctor might be keen to brush you off.
This is a short book (weighing in at a lithe 78 pages), but the information contained therein is very dense, and very convenient to have it all in one place.
As one Amazon reviewer wrote,
❝Someone said you can find the information on the Internet, but I would say good luck with that. It will be many many many hours compiling the gold that is in this book.❞
Writer’s anecdote: indeed, I recently had 14 blood tests done as part of a regular checkup (I’m pleased to report I could not be in better health), and while interpreting the results, I had to look up a lot of things (which were often in the wrong units*), and if I’d had this book already, it would have been a breeze, as it covers everything I had done!
*On which note, this book does provide results in US and International units, so you won’t be left wondering how to convert mmol/mol into mmol/L or mg/dL or such.
Bottom line: if you are a person who has blood, this book will at some point be of immense value to you, if not immediately!
Click here to check out Common Sense Labs, and understand what your blood is saying!
Share This Post
-
The Brain As A Work-In-Progress
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
And The Brain Goes Marching On!
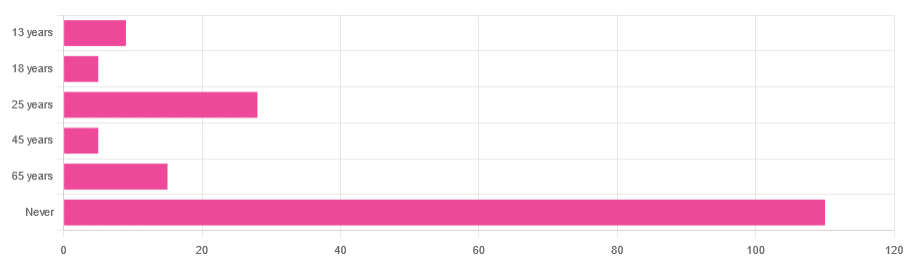
In Tuesday’s newsletter, we asked you “when does the human brain stop developing?” and got the above-depicted, below-described, set of responses:
- About 64% of people said “Never”
- About 16% of people said “25 years”
- About 9% of people said “65 years”
- About 5% of people said “13 years”
- About 3% of people said “18 years”
- About 3% of people said “45 years”
Some thoughts, before we get into the science:
An alternative wording for the original question was “when does the human brain finish developing”; the meaning is the same but the feeling is slightly different:
- “When does the human brain stop developing?” focuses attention on the idea of cessation, and will skew responses to later ages
- When does the human brain finish developing?” focuses on attention on a kind of “is it done yet?” and will skew responses to earlier ages
Ultimately, since we had to chose one word or another, we picked the shortest one, but it would have been interesting if we could have done an A/B test, and asked half one way, and half the other way!
Why we picked those ages
We picked those ages as poll options for reasons people might be drawn to them:
- 13 years: in English-speaking cultures, an important milestone of entering adolescence (note that the concept of a “teenager” is not precisely universal as most languages do not have “-teen” numbers in the same way; the concept of “adolescent” may thus be tied to other milestones)
- 18 years: age of legal majority in N. America and many other places
- 25 years: age popularly believed to be when the brain is finished developing, due to a study that we’ll talk about shortly (we guess that’s why there’s a spike in our results for this, too!)
- 45 years: age where many midlife hormonal changes occur, and many professionals are considered to have peaked in competence and start looking towards retirement
- 65 years: age considered “senior” in much of N. America and many other places, as well as the cut-off and/or starting point for a lot of medical research
Notice, therefore, how a lot of things are coming from places they really shouldn’t. For example, because there are many studies saying “n% of people over 65 get Alzheimer’s” or “n% of people over 65 get age-related cognitive decline”, etc, 65 becomes the age where we start expecting this—because of an arbitrary human choice of where to draw the cut-off for the study enrollment!
Similarly, we may look at common ages of legal majority, or retirement pensions, and assume “well it must be for a good reason”, and dear reader, those reasons are more often economically motivated than they are biologically reasoned.
So, what does the science say?
Our brains are never finished developing: True or False?
True! If we define “finished developing” as “we cease doing neurogenesis and neuroplasticity is no longer in effect”.
Glossary:
- Neurogenesis: the process of creating new brain cells
- Neuroplasticity: the process of the brain adapting to changes by essentially rebuilding itself to suit our perceived current needs
We say “perceived” because sometimes neuroplasticity can do very unhelpful things to us (e.g: psychological trauma, or even just bad habits), but on a biological level, it is always doing its best to serve our overall success as an organism.
For a long time it was thought that we don’t do neurogenesis at all as adults, but this was found to be untrue:
How To Grow New Brain Cells (At Any Age)
Summary of conclusions of the above: we’re all growing new brain cells at every age, even if we be in our 80s and with Alzheimer’s disease, but there are things we can do to enhance our neurogenic potential along the way.
Neuroplasticity will always be somewhat enhanced by neurogenesis (after all, new neurons get given jobs to do), and we reviewed a great book about the marvels of neuroplasticity including in older age:
Our brains are still developing up to the age of 25: True or False?
True! And then it keeps on developing after that, too. Now this is abundantly obvious considering what we just talked about, but see what a difference the phrasing makes? Now it makes it sound like it stops at 25, which this statement doesn’t claim at all—it only speaks for the time up to that age.
A lot of the popular press about “the brain isn’t fully mature until the age of 25” stems from a 2006 study that found:
❝For instance, frontal gray matter volume peaks at about age 11.0 years in girls and 12.1 years in boys, whereas temporal gray matter volume peaks at about age at 16.7 years in girls and 16.2 years in boys. The dorsal lateral prefrontal cortex, important for controlling impulses, is among the latest brain regions to mature without reaching adult dimensions until the early 20s.❞
Source: Structural Magnetic Resonance Imaging of the Adolescent Brain
There are several things to note here:
- The above statement is talking about the physical size of the brain growing
- Nowhere does he say “and stops developing at 25”
However… The study only looked at brains up to the age of 25. After that, they stopped looking, because the study was about “the adolescent brain” so there has to be a cut-off somewhere, and that was the cut-off they chose.
This is the equivalent of saying “it didn’t stop raining until four o’clock” when the reality is that four o’clock is simply when you gave up on checking.
The study didn’t misrepresent this, by the way, but the popular press did!
Another 2012 study looked at various metrics of brain development, and found:
- Synapse overproduction into the teens
- Cortex pruning into the late 20s
- Prefrontal pruning into middle age at least (they stopped looking)
- Myelination beyond middle age (they stopped looking)
Source: Experience and the developing prefrontal cortex ← check out figure 1, and make sure you’re looking at the human data not the rat data
So how’s the most recent research looking?
Here’s a 2022 study that looked at 123,984 brain scans spanning the age range from mid-gestation to 100 postnatal years, and as you can see from its own figure 1… Most (if not all) brain-things keep growing for life, even though most slow down at some point, they don’t stop:
Brain charts for the human lifespan ← check out figure 1; don’t get too excited about the ventricular volume column as that is basically “brain that isn’t being a brain”. Do get excited about the rest, though!
Want to know how not to get caught out by science being misrepresented by the popular press? Check out:
How Science News Outlets Can Lie To You (Yes, Even If They Cite Studies!)
Take care!
Share This Post
-
Banana Bread vs Bagel – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing banana bread to bagel, we picked the bagel.
Why?
Unlike most of the items we compare in this section, which are often “single ingredient” or at least highly standardized, today’s choices are rather dependent on recipe. Certainly, your banana bread and your bagels may not be the same as your neighbor’s. Nevertheless, to compare averages, we’ve gone with the FDA’s Food Central Database for reference values, using the most default average recipes available. Likely you could make either or both of them a little healthier, but as it is, this is how we’ve gone about making it a fair comparison. With that in mind…
In terms of macros, bagels have more than 2x the protein and about 4x the fiber, while banana bread has slightly higher carbs and about 7x more fat. You may be wondering: are the fats healthy? And the answer is, it could be better, could be worse. The FDA recipe went with margarine rather than butter, which lowered the saturated fat to being only ¼ of the total fat (it would have been higher, had they used butter) whereas bagels have no saturated fat at all—which characteristic is quite integral to bagels, unless you make egg bagels, which is rather a different beast. All in all, the macros category is a clear win for bagels, especially when we consider the carb to fiber ratio.
In the category of vitamins, bagels have on average more vitamin B1, B3, B5, and B9, while banana bread has on average more of vitamins A and C. A modest win for bagels.
When it comes to minerals, bagels are the more nutrient dense with more copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while banana bread is not higher in any minerals. An obvious and easy win for bagels.
Closing thoughts: while the micronutrient profile quite possibly differs wildly from one baker to another, something that will probably stay more or less the same regardless is the carb to fiber ratio, and protein to fat. As a result, we’d weight the macros category as the more universally relevant. Bagels won in all categories today, as it happened, but it’s fairly safe to say that, on average, a baker who makes bagels and banana bread with the same levels of conscientiousness for health (or lack thereof) will tend to make bagels that are healthier than banana bread, based on the carb to fiber ratio, and the protein to fat ratio.
Enjoy!
Want to learn more?
You might like to read:
- Should You Go Light Or Heavy On Carbs?
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Wholewheat Bread vs Seeded White – Which is Healthier?
Take care!
Share This Post
Related Posts
-
Before You Eat Breakfast: 3 Surprising Facts About Intermittent Fasting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. William Li is well-known for his advocacy of “eating to beat disease”, and/but today he has advice for us about not eating to beat disease. In moderation, of course, thus: intermittent fasting.
The easy way
Dr. Li explains the benefits of intermittent fasting; how it improves the metabolism and gives the body a chance to do much-needed maintainance, including burning off any excess fat we had hanging around.
However, rather than calling for us to do anything unduly Spartan, he points out that it’s already very natural for us to fast while sleeping, so we only need to add a couple of hours before and after sleeping (assuming an 8 hour sleep), to make it to a 12-hour fast for close to zero effort and probably no discomfort.
And yes, he argues that a 12-hour fast is beneficial, and even if 16 hours would be better, we do not need to beat ourselves up about getting to 16; what is more important is sustainability of the practice.
Dr. Li advocates for flexibility in fasting, and that it should be done by what manner is easiest, rather than trying to stick to something religiously (of course, if you do fast for religious reasons, that is another matter, and/but beyond the scope of this today).
For more information on each of these, as well as examples and tips, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Intermittent Fasting: What’s the truth?
- 16/8 Intermittent Fasting For Beginners
- Meal Timings & Health: How Important Is Breakfast?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
7 Ways To Boost Mitochondrial Health To Fight Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fatigue and a general lack of energy can be symptoms of many things, and for most of them, looking after our mitochondrial health can at least help, if not outright fix the issue.
The Seven Ways
Dr. Jonas Kuene suggests that we…
- Enjoy a good diet: especially, limiting simple sugars, reducing overall carbohydrate intake, and swapping seed oils for healthier oils like avocado oil and olive oil.
- Take supplements: including coenzyme Q10, alpha-lipoic acid, and vitamins
- Decrease exposure to toxins: limit alcohol consumption (10almonds tip: limit it to zero if you can), avoid foods that are likely high in heavy metals or pesticides, and check you’re not being overmedicated (there can be a bit of a “meds creep” over time if left unchecked, so it’s good to periodically do a meds review in case something is no longer needed)
- Practice intermittent fasting: Dr. Kuene suggests a modest 16–18 hours fast per week; doing so daily is generally considered good advice, for those for whom this is a reasonable option
- Build muscle: exercise in general is good for mitochondria, but body composition itself counts for a lot too
- Sleep: aiming for 7–9 hours, and if that’s not possible at night, add a nap during the day to make up the lost time
- Get near-infrared radiation: from the sun, and/or made-for-purpose IR health devices.
For more info on these (including the referenced science), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Coenzyme Q10 From Foods & Supplements
- How To Reduce Or Quit Alcohol
- Intermittent Fasting: What’s the truth?
- Build Muscle (Healthily!)
- Red Light, Go!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Stickers and wristbands aren’t a reliable way to prevent mosquito bites. Here’s why
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Protecting yourself and family from mosquito bites can be challenging, especially in this hot and humid weather. Protests from young children and fears about topical insect repellents drive some to try alternatives such as wristbands, patches and stickers.
These products are sold online as well as in supermarkets, pharmacies and camping stores. They’re often marketed as providing “natural” protection from mosquitoes.
But unfortunately, they aren’t a reliable way to prevent mosquito bites. Here’s why – and what you can try instead.
Why is preventing mosquito bites important?
Mosquitoes can spread pathogens that make us sick. Japanese encephalitis and Murray Valley encephalitis viruses can have potentially fatal outcomes. While Ross River virus won’t kill you, it can cause potentially debilitating illnesses.
Health authorities recommend preventing mosquito bites by: avoiding areas and times of the day when mosquitoes are most active; covering up with long sleeved shirts, long pants, and covered shoes; and applying a topical insect repellent (a cream, lotion, or spray).
I don’t want to put sticky and smelly repellents on my skin!
While for many people, the “sting” of a biting mosquitoes is enough to prompt a dose of repellent, others are reluctant. Some are deterred by the unpleasant feel or smell of insect repellents. Others believe topical repellents contain chemicals that are dangerous to our health.
However, many studies have shown that, when used as recommended, these products are safe to use. All products marketed as mosquito repellents in Australia must be registered by the Australian Pesticides and Veterinary Medicines Authority; a process that provides recommendations for safe use.
How do topical repellents work?
While there remains some uncertainty about how the chemicals in topical insect repellents actually work, they appear to either block the sensory organs of mosquitoes that drive them to bite, or overpower the smells of our skin that helps mosquitoes find us.
Diethytolumide (DEET) is a widely recommended ingredient in topical repellents. Picaridin and oil of lemon eucalyptus are also used and have been shown to be effective and safe.
How do other products work?
“Physical” insect-repelling products, such as wristbands, coils and candles, often contain a botanically derived chemical and are often marketed as being an alternative to DEET.
However, studies have shown that devices such as candles containing citronella oil provide lower mosquito-bite prevention than topical repellents.
A laboratory study in 2011 found wristbands infused with peppermint oil failed to provide full protection from mosquito bites.
Even as topical repellent formulations applied to the skin, these botanically derived products have lower mosquito bite protection than recommended products such as those containing DEET, picaridin and oil of lemon eucalyptus.
Wristbands infused with DEET have shown mixed results but may provide some bite protection or bite reduction. DEET-based wristbands or patches are not currently available in Australia.
There is also a range of mosquito repellent coils, sticks, and other devices that release insecticides (for example, pyrethroids). These chemicals are primarily designed to kill or “knock down” mosquitoes rather than to simply keep them from biting us.
What about stickers and patches?
Although insect repellent patches and stickers have been available for many years, there has been a sudden surge in their marketing through social media. But there are very few scientific studies testing their efficacy.
Our current understanding of the way insect repellents work would suggest these small stickers and patches offer little protection from mosquito bites.
At best, they may reduce some bites in the way mosquito coils containing botanical products work. However, the passive release of chemicals from the patches and stickers is likely to be substantially lower than those from mosquito coils and other devices actively releasing chemicals.
One study in 2013 found a sticker infused with oil of lemon eucalyptus “did not provide significant protection to volunteers”.
Clothing impregnated with insecticides, such as permethrin, will assist in reducing mosquito bites but topical insect repellents are still recommended for exposed areas of skin.
Take care when using these products
The idea you can apply a sticker or patch to your clothing to protect you from mosquito bites may sound appealing, but these devices provide a false sense of security. There is no evidence they are an equally effective alternative to the topical repellents recommended by health authorities around the world. It only takes one bite from a mosquito to transmit the pathogens that result in serious disease.
It is also worth noting that there are some health warnings and recommendations for their use required by Australian Pesticides and Veterinary Medicines Authority. Some of these products warn against application to the skin (recommending application to clothing only) and to keep products “out of reach of children”. This is a challenge if attached to young children’s clothing.
Similar warnings are associated with most other topical and non-topical mosquito repellents. Always check the labels of these products for safe use recommendations.
Are there any other practical alternatives?
Topical insect repellents are safe and effective. Most can be used on children from 12 months of age and pose no health risks. Make sure you apply the repellent as a thin even coat on all exposed areas of skin.
But you don’t need “tropical strength” repellents for short periods of time outdoors; a range of formulations with lower concentrations of repellent will work well for shorter trips outdoors. There are some repellents that don’t smell as strong (for example, children’s formulations, odourless formulations) or formulations that may be more pleasant to use (for example, pump pack sprays).
Finally, you can always cover up. Loose-fitting long-sleeved shirts, long pants, and covered shoes will provide a physical barrier between you and mosquitoes on the hunt for your or your family’s blood this summer.
Cameron Webb, Clinical Associate Professor and Principal Hospital Scientist, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: