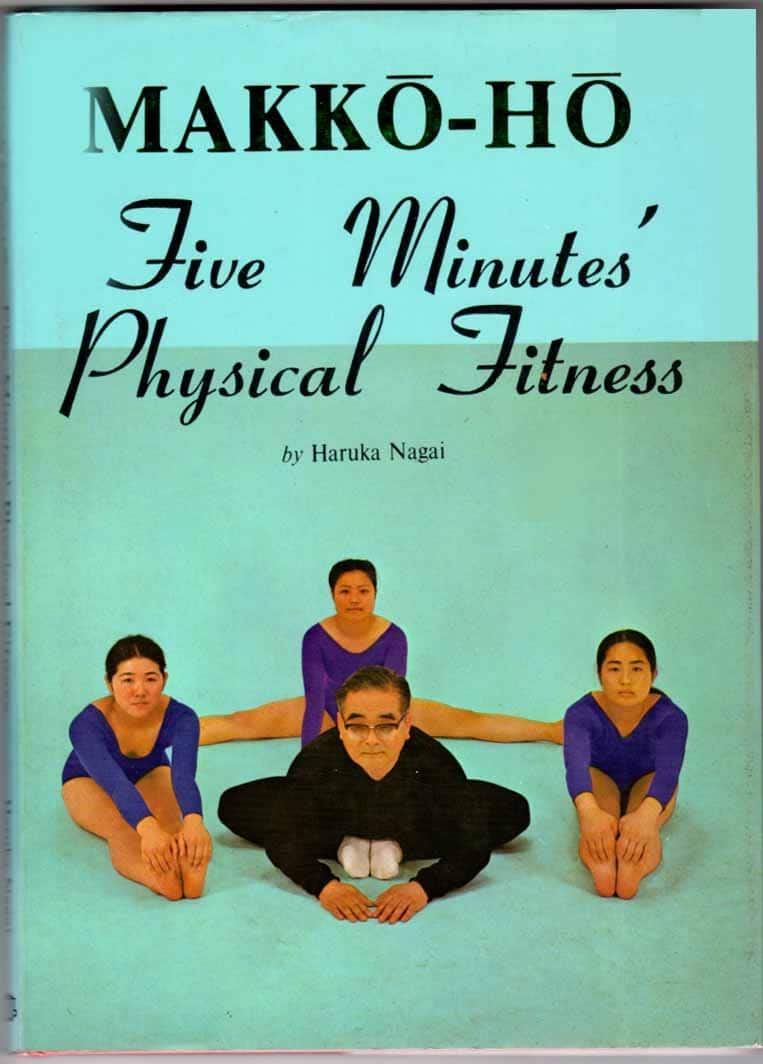
Makkō-Hō – by Haruka Nagai
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all heard the claims, “Fluent in 3 Months!”, “Russian in Two Weeks!”, “Overnight Mandarin Chinese”, “15-Minute Arabic!”, “Instant Italian!”.
We see the same in the world of health and fitness too. So how does this one’s claim of “five minutes’ physical fitness” hold up?
Well, it is 5 minutes per day. And indeed, the author writes:
❝The total time [to do these exercises], then, is only one minute and thirty seconds. This series I call one round. When it has been completed, execute another complete round. You should find the exercises easier to do the second time. Executed this way, the exercsies will prove very effective, though they take only three minutes in all. After you have leaned back into the final position, you must remain in that posture for one minute. That brings the total time to four minutes. Even when [some small additions] are added, it takes only five minutes at most.❞
The exercises themselves are from makkō-hō, which is a kind of Japanese dynamic yoga. They involve repetitions of (mostly) moving stretches with good form, and are excellent for mobility and general health, keeping us supple and robust as we get older.
The text descriptions are clear, as are the diagrams and photos. The language is a little dated, as this book was written in the 1970s, but the techniques themselves are timeless.
Bottom line: consider it a 5-minute anti-aging regimen. And, as Nagai says, “the person who cannot find 5 minutes out of 24 hours, was never truly interested in their health”.
Click here to check out Makkō-Hō and schedule your five minutes!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Self-Care That’s Not Just Self-Indulgence
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Self-Care That’s Not Just Self-Indulgence
Self-care is often seen as an excuse for self-indulgence. Worse, it’s often used as an excuse for self-indulgence—in ways that can end up making us feel worse.
It’s a bit like dietary “cheat days”. If your diet needs cheat days, your diet probably isn’t right for you!
How to recognize the difference between self-care and self-indulgence?
Statistically, the majority of our subscribers are parents (whose children are now mostly grown up, but still, the point is that parenting experience has been gleaned), and/or are or have been caregivers of some form or other.
When a small child is ill, we (hopefully!) look after them carefully:
- We don’t expect too much of them, but…
- …we do expect them to adhere to things consistent with their recovery.
Critically: an important part of self-care is that it actually should be care.
Let’s spell something out: neglect is not care!
How this works for physical and mental health
If you overdo it in physical exercise, it’s right and correct to take a break to recover, and during that time, do things that will hasten one’s recovery. For example:
Overdone It? How To Speed Up Recovery After Exercise
But it’s well-known that if you just do nothing, your condition will likely deteriorate. Also, “a break to recover” is going to be as short as is necessary to recover. Then you’ll ease back into exercise, but you will get back to it.
For mental health it’s just the same. If we for whatever reason need to take a step back, it’s right and correct to do take a break to recover, and during that time, do things that will hasten one’s recovery.
Sometimes, if for example it’s just a case of burnout, rest is the best medicine, and even rest can be an active process. See for example:
How To Rest More Efficiently (Yes, Really)
So the question to ask, when it comes to self-care vs self-indulgence, is:
“Is this activity helping me to get better?”
Some examples:
Probably not great self-care activities:
- Oversleeping (unless you were sleep-deprived, in which case, it’s better to get an earlier night than a later morning, if possible)
- Overeating (comfort-eating is a thing, but your actual problems will still be there)
- Mindless activities (mindless scrolling, TV-watching, game-playing, etc)
Probably better self-care activities:
- Enjoyable physical activity (whatever that may be for you)
- Preparing your favorite food, and then enjoying it mindfully
- Engaging in a personal project that might not be that important, but it’s fulfilling to you (hobbies etc can fall into this category)
- Scheduling some time, and committing some resources, to tackling whatever problem(s) you are facing that’s prompting you to need this self-care.
- Doing the tasks you want to hide away from, but making them fun.
What’s your go-to self-care? We love to hear from you, so feel free to hit “reply” to this email, or use the handy feedback form at the bottom!
Share This Post
-
Stimulant Users Are Caught in Fatal ‘Fourth Wave’ of Opioid Epidemic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In Pawtucket, Rhode Island, near a storefront advertising “free” cellphones, J.R. sat in an empty back stairwell and showed a reporter how he tries to avoid overdosing when he smokes crack cocaine. KFF Health News is identifying him by his initials because he fears being arrested for using illegal drugs.
It had been several hours since his last hit, and the chatty, middle-aged man’s hands moved quickly. In one hand, he held a glass pipe. In the other, a lentil-size crumb of cocaine.
Or at least J.R. hoped it was cocaine, pure cocaine — uncontaminated by fentanyl, a potent opioid that was linked to about 75% of all overdose deaths in Rhode Island in 2022. He flicked his lighter to “test” his supply. He believed that if it had a “cigar-like sweet smell,” he said, it would mean that the cocaine was laced with fentanyl. He put the pipe to his lips and took a tentative puff. “No sweet,” he said, reassured.
But this method offers only false and dangerous reassurance. A mistake can be fatal.
It is impossible to tell whether a drug contains fentanyl by the taste or smell. “Somebody can believe that they can smell it or taste it, or see it … but that’s not a scientific test,” said Josiah “Jody” Rich, an addiction specialist and researcher who teaches at Brown University. “People are going to die today because they buy some cocaine that they don’t know has fentanyl in it.”
The first wave of the long-running and devastating opioid epidemic began in the United States with the abuse of prescription painkillers in the early 2000s. The second wave involved an increase in heroin use, starting around 2010. The third wave began when powerful synthetic opioids such as fentanyl started appearing in the supply around 2015. Now experts are observing a fourth phase of the deadly epidemic.
The mix of stimulants such as cocaine and methamphetamines with fentanyl — a synthetic opioid 50 times as powerful as heroin — is driving what experts call the opioid epidemic’s “fourth wave.” The mixture of stimulants and fentanyl presents powerful challenges to efforts to reduce overdoses because many users of stimulants don’t know they are at risk of ingesting opioids, so they don’t take overdose precautions.
The only way to know whether cocaine or other stimulants contain fentanyl is to use drug-checking tools such as fentanyl test strips — a best practice for what’s known as “harm reduction,” now embraced by federal health officials in combating drug overdose deaths. Fentanyl test strips cost as little as $2 for a two-pack online, but many front-line organizations also give them out free.
Nationwide, illicit stimulants mixed with fentanyl were the most common drugs found in fentanyl-related overdoses, according to a study published in 2023 in the scientific journal Addiction. The stimulant in the fatal mixture tends to be cocaine in the Northeast, and methamphetamine in the West and much of the Midwest and South.
“The No. 1 thing that people in the U.S. are dying from in terms of drug overdoses is the combination of fentanyl and a stimulant,’’ said Joseph Friedman, a researcher at UCLA and the study’s lead author. “Black and African Americans are disproportionately affected by this crisis to a large magnitude, especially in the Northeast.”
Friedman was also the lead author of another new study, published in the American Journal of Psychiatry, that shows the fourth wave of the opioid epidemic is driving up the mortality rate among older Black Americans (ages 55-64) and, more recently, Hispanic people. Friedman said part of the reason street fentanyl is so deadly is that there’s no way to tell how potent it is. Hospitals have safely used medical-grade fentanyl for surgical pain because the potency is strictly regulated, but “the potency fluctuates wildly in the illicit market” Friedman said.
Studies of street drugs, he said, show that in illicit drugs the potency can vary from 1% to 70% fentanyl.
“Imagine ordering a mixed drink in a bar and it contains one to 70 shots,” Friedman said, “and the only way you know is to start drinking it. … There would be a huge number of alcohol overdose deaths.”
Drug-checking technology can provide a rough estimate of fentanyl concentration, he said, but to get a precise measure requires sending drugs to a laboratory.
It’s not clear how much of the latest trend in polydrug use — in which users mix substances, such as cocaine and fentanyl, for example — is accidental versus intentional. It can vary for individual users: a recent study from Millennium Health found that most people who use fentanyl do so at times intentionally and other times unintentionally.
People often use stimulants to power through the rapid withdrawal from fentanyl, Friedman said. And the high-risk practice of using cocaine or meth with heroin, known as “speedballing,” has been around for decades. Other factors include manufacturers’ adding the cheap synthetic opioid to a stimulant to stretch their supply, or dealers mixing up bags.
Researchers say many people still think they are using unadulterated cocaine or crack — a misconception that can be deadly. “Folks who are using stimulants, and not intentionally using opioids, are unprepared to respond to an opioid overdose,” said Brown University epidemiologist Jaclyn White Hughto, “because they don’t perceive themselves to be at risk.” Hughto is a principal investigator in a new, unpublished study called “Preventing Overdoses Involving Stimulants.”
Hughto and the team surveyed more than 260 people in Rhode Island and Massachusetts who use drugs, including some who manufacture and distribute stimulants such as cocaine. More than 60% of the people they interviewed in Rhode Island had bought or used stimulants that they later found out had fentanyl in them. And many of the people interviewed in the study also use drugs alone. That means that if they do overdose, they may not be found until it’s too late.
In 2022, Rhode Island had the fourth-highest rate of overdose deaths involving cocaine in 2022, after Washington, D.C., Delaware, and Vermont, according to the Centers for Disease Control and Prevention.
The fourth wave is also hitting stimulant users who choose pills over what they perceive as more dangerous drugs such as cocaine in an effort to avoid fentanyl. That’s what happened to Jennifer Dubois’ son Cliffton.
Dubois was a single mother raising two Black sons. The older son, Cliffton, had been struggling with addiction since he was 14, she said. Cliffton also had been diagnosed with attention-deficit/hyperactivity disorder and a mood disorder.
In March 2020, Cliffton had checked into a rehab program as the pandemic ramped up, Dubois said. Because of the lockdown at rehab, Cliffton was upset about not being able to visit with his mother. “He said, ‘If I can’t see my mom, I can’t do treatment,’” Dubois recalled. “And I begged him” to stay in treatment.
But soon after, Cliffton left the rehab program. He showed up at her door. “And I just cried,” she said.
Dubois’ younger son was living at home. She didn’t want Cliffton doing drugs around his younger brother. So she gave Cliffton an ultimatum: “If you want to stay home, you have to stay drug-free.”
Cliffton went to stay with family friends, first in Atlanta and later in Woonsocket, an old mill city that has Rhode Island’s highest rate of drug overdose deaths.
In August 2020, Cliffton overdosed but was revived. Cliffton later confided that he’d been snorting cocaine in a car with a friend, Dubois said. Hospital records show he tested positive for fentanyl.
“He was really scared,” Dubois said. After the overdose, he tried to “leave the cocaine and the hard drugs alone,” she said. “But he was taking pills.” Eight months later, on April 17, 2021, Cliffton was found unresponsive in the bedroom of a family member’s home.
The night before, Cliffton had bought counterfeit Adderall, according to the police report. What he didn’t know was that the Adderall pill was laced with fentanyl. “He thought by staying away from the street drugs and just taking pills, he was doing better,” Dubois said.
A fentanyl test strip could have saved his life.
This article is from a partnership that includes The Public’s Radio, NPR, and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
Heal Your Stressed Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Rochelle Walsh, therapist, explains the problem and how to fix it:
Not all brain damage is from the outside
Long-term stress and burnout cause brain damage; it’s not just a mindset issue—it impacts the brain physiologically. To compound matters, it also increases the risk of neurodegenerative diseases. While the brain can indeed grow new neurons and regenerate itself, chronic stress damages specific regions, and inhibits that.
There are some effects of chronic stress that can seem positive—the amygdalae and hypothalamus are seen to grow larger and stronger, for instance—but this is, unfortunately, “all the better to stress you with”. In compensation for this, chronic stress deprioritizes the pre-frontal cortex and hippocampi, so there goes your reasoning and memory.
This often results in people not managing chronic stress well. Just like a weak heart and lungs might impede the exercise that could make them stronger, the stressed brain is not good at permitting you to do the things that would heal it—preferring to keep you on edge all day, worrying and twitchy, mind racing and body tense. It also tends to lead to autoimmune diseases, due to the increased inflammation (because the body’s threat-detection system as at “jumping at own shadow” levels so it’s deploying every defense it has, including completely inappropriate ones).
Notwithstanding the “Heal Your Stressed Brain” thumbnail, she doesn’t actually go into this in detail and bids us sign up for her masterclass. We at 10almonds however like to deliver, so you can find useful advice and free resources in our links-drop at the bottom of this article.
Meanwhile, if you’d like to hear more about the neurological woes described above, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Meditation That You’ll Actually Enjoy
- How To Manage/Reduce Chronic Stress
- Lower Your Cortisol! (Here’s Why & How)
- How Healthy People Regulate Their Emotions
- Sleep: Yes, You Really Do Still Need It!
- Give Your Adrenal Glands A Chance
- The Stress Prescription (Against Aging!)
Take care!
Share This Post
Related Posts
-
Debunking the myth that vaccines cause autism
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The myth that autism is linked to childhood vaccines first appeared in a 1998 study by British physician Dr. Andrew Wakefield. The study was later retracted, and Wakefield was discredited. But nearly three decades after the study’s publication, the myth persists, championed by activists, political leaders, and even potential health officials.
There is overwhelming evidence that there is no link between vaccines and autism. “No one has any real or solid evidence that vaccines cause autism,” says Catherine Lord, a psychologist and autism researcher at the University of California, Los Angeles.
Here are just some of the many reasons that we know vaccines don’t cause autism.
The Wakefield study has been thoroughly discredited
In 1998, the Lancet published a study describing a small group of children who reportedly had bowel inflammation and developed autism within a month of getting the measles, mumps, and rubella (MMR) vaccine. The study proposed that the vaccination triggered bowel inflammation and developmental delays, including autism. Lead author Andrew Wakefield coined the term “autistic enterocolitis” to describe the condition he and his colleagues claimed to have discovered.
The study received significant media attention and immediate criticism from scientists, who pointed out the study’s small size, lack of controls, and insufficient evidence to support its conclusions.
Subsequent research published over the next few years refuted Wakefield’s findings. A 1999 Lancet study found no link between autism and the MMR vaccine, and a 2001 study found no evidence of a link or the existence of so-called autistic enterocolitis.
In 2010, the Lancet finally retracted Wakefield’s fraudulent study, noting that “several elements” of the study were “incorrect” and that the experiments carried out on children had not been approved by an ethics board. The journal’s editor called the paper’s conclusions “utterly false.”
A few months later, Wakefield was stripped of his medical license by the United Kingdom’s General Medical Council. The council deemed Wakefield “dishonest and irresponsible” and concluded that he conducted unethical experiments on children.
The committee’s investigation also revealed that, less than a year before he published his study claiming that the MMR vaccine was linked to bowel inflammation that triggered autism, Wakefield filed a patent for a standalone measles vaccine and inflammatory bowel disease treatment.
Thimerosal was removed from childhood vaccines in 2001—with no effect on autism rates
A 2003 study published by a conservative group known for promoting anti-science myths—including that HIV doesn’t cause AIDS—first proposed that the preservative thimerosal in childhood vaccines is linked to autism. This supposed link was subsequently disproven.
Thimerosal is added in small amounts to some vaccines to prevent dangerous bacterial and fungal contamination. The substance contains ethylmercury, a form of mercury that the body quickly and safely processes in small doses.
Ethylmercury is different from methylmercury, a far more dangerous form of mercury that is toxic at low doses. By contrast, the small amount of thimerosal in some vaccines is harmless to humans and is equal to the amount of mercury in a can of tuna.
The preservative was removed from childhood vaccines as a precautionary measure in 2001. With the exception of some flu shots, no childhood vaccine contains the preservative and hasn’t for more than two decades. Autism rates have not decreased as a result of thimerosal being removed from childhood immunization vaccines. While some types of the annual flu vaccine contain thimerosal, you can get one without it.
Extensive research also shows that neither thimerosal nor methylmercury at any dose is linked to autism. A 2008 study of statewide California data found that autism rates “increased consistently for children born from 1989 through 2003, inclusive of the period when exposure to [thimerosal-containing vaccines] has declined.”
Autism rates are the same in vaccinated and unvaccinated children
Vaccine opponents often falsely claim that vaccinated children are more likely than unvaccinated children to develop autism. Decades of research disprove this false claim.
A 2002 analysis of every child born in Denmark over eight years found that children who received MMR vaccines were no more likely to be diagnosed with autism than unvaccinated children.
A 2015 study of over 95,000 U.S. siblings found that MMR vaccination is not associated with increased autism diagnosis. This was true even among the siblings of children with autism, who are seven times more likely to develop autism than children without an autistic sibling.
And a 2018 study found some evidence that children with autism—and their siblings—were more likely to be unvaccinated or under-vaccinated than children without autism.
Vaccination also has no impact on autism rates at the population level, regardless of the age at which children get vaccinated.
“In comparing countries that have different timing and levels of vaccination … there’s no difference in autism,” says Lord. “You can look at different countries with different rates of autism, and there’s no relationship between the rates of autism and vaccinations.”
Countries such as Taiwan, Tunisia, Turkey, and Morocco, which have some of the world’s lowest autism rates, have childhood immunization rates that are nearly identical to countries with the highest autism rates, including Sweden, Japan, Brunei, and Singapore.
Improved awareness and diagnosis play a role in rising autism rates
Autism was first described in 1911 when it was considered to be a form of severe schizophrenia. Over a century later, our understanding of autism has changed drastically, as have diagnostic standards.
A 2013 scientific article describing how medical and social perceptions of autism have evolved explains that “the diagnoses of schizophrenia, psychosis and autism in children were largely interchangeable during the 1940s and 1950s.” Beginning in the 1960s, methods of diagnosing autism improved, “increasing the number of children who were considered to display autistic traits.”
The autism diagnosis was changed to autism spectrum disorder in 2013. “This category is now very broad, which was an intentional choice to help provide services to the greatest number of people who might need them,” writes Gideon Meyerowitz-Katz, an epidemiologist and creator of the popular Health Nerd blog.
“Rather than the severe intellectual disability of the 1940s and 50s, [autism spectrum disorder] is a group of behaviours that can be any severity as long as they are persistent and impact people’s daily functioning in a significant way.”
For more information about autism, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
L-Theanine: What’s The Tea?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
L-Theanine: What’s The Tea?
We’ve touched previously on l-theanine, when this newsletter was new, and we had only a few hundred subscribers and the carefully organized format wasn’t yet what it is today.
So now it’s time to give this potent dietary compound / nutritional supplement the “Monday Research Review” treatment…
What is it?
L-theanine is an amino acid found in tea. The human body can’t produce it, and/but it’s not essential for humans. It does have a lot of benefits, though. See for example:
L-Theanine as a Functional Food Additive: Its Role in Disease Prevention and Health Promotion
How does it work?
L-theanine works by moderating and modulating the brain’s neurotransmitters.
This sounds fancy, but basically it means: it doesn’t actually add anything in the manner of a drug, but it changes how we use what we have naturally.
What does it do? Read on…
It increases mental focus
It has been believed that l-theanine requires the presence of caffeine to achieve this (i.e., it’s a combination-only effect). For example:
But as it turns out, when a group of researchers actually checked… This isn’t true, as Foxe et al. write:
❝We asked whether either compound alone, or both in combination, would affect performance of the task in terms of reduced error rates over time, and whether changes in alpha-band activity would show a relationship to such changes in performance. When treated with placebo, participants showed a rise in error rates, a pattern that is commonly observed with increasing time-on-task, whereas after caffeine and theanine ingestion, error rates were significantly reduced. The combined treatment did not confer any additional benefits over either compound alone, suggesting that the individual compounds may confer maximal benefits at the dosages employed❞
It promotes a calmly wakeful feeling of serenity
Those are not words typically found in biopharmaceutical literature, but they’re useful here to convey:
- L-theanine promotes relaxation without causing drowsiness
- L-theanine promotes mental alertness without being a stimulant
Here is where l-theanine really stands out from caffeine. If both substances promote mental focus, but one of them does it by making us “wired” and the other does it while simultaneously promoting calm, it makes the choice between them clearer!
Read more: L-theanine, a natural constituent in tea, and its effect on mental state
It relieves stress and anxiety
Building on from the above, but there’s more: l-theanine relieves stress and anxiety in people experiencing stressful situations, without any known harmful side effects… This is something that sets it apart from a lot of anxiolytic (antianxiety) drugs!
Here’s what a big systematic review of clinical trials had to say:
Theanine consumption, stress and anxiety in human clinical trials: A systematic review
L-theanine has other benefits too
We’ve talked about some of the most popular benefits of l-theanine, and we can’t make this newsletter too long, but research also suggests that it…
- Supports healthy weight management
- Reduces inflammation
- Supports immune health
- Helps fight cancer
- May extend lifespan ← this one’s a C. elegans study, but despite being a tiny worm, they actually function very similarly to humans on a cellular level; it’s why they’re used so much for anti-aging research
If you’re interested in this topic, we recommend also reading our previous article on l-theanine—pardon that we hadn’t really nailed down our style yet—but there’s a bunch of useful information about how l-theanine makes caffeine “better” in terms of benefits. We also talk dosage, and reference some other studies we didn’t have room to include today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Curing Hiccups And Headaches At Home With Actual Science
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Quick fixes for bodily annoyances
Do you ever find yourself desperately trying to cure hiccups, and advice on the Internet is like “breathe in through your ears while drinking vinegar upside-down through your nose”?
If so, you’re not alone. So, today we’re going to look at some science-based approaches to dealing with common bodily annoyances.
Hiccups
Unfortunately, most popular advices simply don’t work, and the only near-guaranteed way to cure these is with anti-convulsive medications whose side-effects may be worse than the hiccups.
However, before you head to the pharmacy, there is one breathing exercise that has a very simple scientific underpinning: 4:4 breathing. If you’re unfamiliar, it’s just:
- Breathe slowly in through your nose to a count of four
- Hold your breath for a count of four
- Breathe slowly out through your nose to a count of four
- Hold your breath for a count of four
…and repeat. The slower the better. At first, your hiccups will interrupt this, but just “keep calm and carry on”.
The reason this can work is that breathing is an autonomic function (e.g., it happens without us thinking about it) that, unlike most other autonomic functions, we can all control directly. By taking control of one, others will tend to fall into line with it.
For example, it is normal that your heart rate will tend to slow or quicken as your breathing slows or quickens, respectively.
Your hiccups? Autonomic function. Actually a very, very old evolutionary left-over trait, that’s only useful for protecting lungs while breathing underwater. In other words, it’s the bodily function thinks you’re a fish (or a tadpole-like amphibious creature) in the process of developing lungs. Unfortunately, because hiccuping doesn’t harm our chances of passing on our genes, it never got naturally de-selected so we still have it.
Anyway, the bottom line is: take control of your breathing in the aspects you can directly control, and the aspects you can’t directly control will fall into line. You may need to give it some minutes, don’t give up too quickly.
Headaches
If you ever get a headache and you don’t have painkillers or perhaps they’re not helping or you have another reason for not wanting to take them, there’s “one quick trick” that can cure most headaches in seconds.
First, the limitation: this will only cure headaches that have been caused by increased localized blood pressure in the forehead. However, that’s more than half of most common headaches.
Next, how it works…
We’re mentioning this first, because understanding how it works will give you more confidence in using it.
Your body has a wonderful homeostatic system, which is the system by which your body maintains its “Goldilocks zones” of not too hot or cold, not to acidine or alkaline, not too hydrated or dehydrated, blood pressure not too high or too low, etc. Sometimes, however, it can get confused, and needs a nudge back to where it should be.
One of the ways it maintains blood pressure is biofeedback from receptors in blood vessel walls, called baroreceptors. They are what it sounds like; they measure blood pressure internally.
In certain places, there are clusters of baroreceptors in one place. And if we press on that one place, the body will think “Oh no! Super high blood pressure in this bit!” and reduce the blood pressure immediately.
This is called the baroreflex, and that’s what you need to cure a hypertensive headache.
So, what to do:
With your thumb, carefully feel the upper inside corner of your eye socket. So, at the top, and about ¼ of the way out from the bridge of your nose. You should feel a groove. No, not like the Emperor’s New, but, an actual groove in your eye socket. That’s the supraorbital notch (or foramen), and it allows the supraorbital artery, veins, and nerve to run through.
Press it firmly (you can do both sides at once, assuming you have two thumbs) for about three seconds, and then massage it gently. Repeat as necessary, but it shouldn’t take more than about three goes to have cured the headache.
As a bonus, this is a great party trick for curing other people’s headaches, when the need arises!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: