How To Kill Laziness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Laziness Is A Scooby-Doo Villain.
Which means: to tackle it requires doing a Scooby-Doo unmasking.
You know, when the mystery-solving gang has the “ghost” or “monster” tied to a chair, and they pull the mask off, to reveal that there was no ghost etc, and in fact it was a real estate scammer or somesuch.
Social psychologist Dr. Devon Price wrote about this (not with that metaphor though) in a book we haven’t reviewed yet, but will one of these days:
Laziness Does Not Exist – by Dr. Devon Price (book)
In the meantime, and perhaps more accessibly, he gave a very abridged summary for Medium:
Medium | Laziness Does Not Exist… But unseen barriers do (11mins read)
Speaking of barriers, Medium added a paywall to that (the author did not, in fact, arrange the paywall as Medium claim), so in case you don’t have an account, he kindly made the article free on its own website, here:
Devon Price | Laziness Does Not Exist… But unseen barriers do (same article; no paywall)
He details problems that people get into (ranging from missed deadlines to homelessness), that are easily chalked up to laziness, but in fact, these people are not lazily choosing to suffer, and are usually instead suffering from all manner of unchosen things, ranging from…
- imposter syndrome / performance anxiety,
- perfectionism (which can overlap a lot with the above),
- social anxiety and/or depression (these also can overlap for some people),
- executive dysfunction in the brain, and/or
- just plain weathering “the slings and arrows of outrageous fortune [and] the heartache and the thousand natural shocks that flesh is heir to”, to borrow from Shakespeare, in ways that aren’t always obviously connected—these things can be great or small, it could be a terminal diagnosis of some terrible disease, or it could be a car breakdown, but the ripples spread.
And nor are you, dear reader, choosing to suffer (even if sometimes it appears otherwise)
Unless you’re actually a masochist, at least, in which case, you do you. But for most of us, what can look like laziness or “doing it to oneself” is usually a case of just having one or more of the above-mentioned conditions in place.
Which means…
That grace we just remembered above to give to other people?
Yep, we should give that to ourselves too.
Not as a free pass, but in the same way we (hopefully) would with someone else, and ask: is there some problem I haven’t considered, and is there something that would make this easier?
Here are some tools to get you started:
- Imposter Syndrome (And Why Almost Everyone Has It)
- Perfectionism, And How To Make Yours Work For You
- How To Set Anxiety Aside
- Mental Health First-Aid (To Get Yourself Or A Loved One Through Depression)
- Procrastination, And How To Pay Off The To-Do List Debt
- Take This Two-Minute Executive Dysfunction Test
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Your Sleep Position Changes Dementia Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is not just about sleep duration or even about sleep quality… It really is about which way your body is positioned.
Goodnight, glymphatic system
The association between sleeping position and dementia risk is about glymphatic drainage, which is largely powered by gravity (and thus dependent on which way around your head and neck are oriented), and very important for clearing toxins out of the brain—including beta-amyloid proteins.
This becomes particularly important when the glymphatic system becomes less efficient in midlife, often 15–20 years before cognitive decline symptoms appear.
The video’s thumbnail headline, “SCIENTISTS REVEAL: THE WAY YOUR SLEEP CAN CAUSE DEMENTIA” is overstated and inaccurate, but our adjusted headline “how your sleep position changes dementia risk” is actually representative of the paper on which this video was based; we’ll quote from the paper itself here:
❝This paper concludes that 1. glymphatic clearance plays a major role in Alzheimer’s pathology; 2. the vast majority of waste clearance occurs during sleep; 3. dementias are associated with sleep disruption, alongside an age-related decline in AQP4 polarization; and 4. lifestyle choices such as sleep position, alcohol intake, exercise, omega-3 consumption, intermittent fasting and chronic stress all modulate* glymphatic clearance. Lifestyle choices could therefore alter Alzheimer’s disease risk through improved glymphatic clearance, and could be used as a preventative lifestyle intervention for both healthy brain ageing and Alzheimer’s disease.❞
…and specifically, they found:
❝Glymphatic transport is most efficient in the right lateral sleeping position, with more CSF clearance occurring compared to supine and prone. The average person changes sleeping position 11 times per night, but there was no difference in the number of position changes between neurodegenerative and control groups, making the percentage of time spent in supine position the risk factor, not the number of position changes❞
Read the paper in full here: The Sleeping Brain: Harnessing the Power of the Glymphatic System through Lifestyle Choices
*saying “modulate” here is not as useful as it could be, because they modulate it differently: side-sleeping improves clearance; back sleeping decreases it; front-sleeping isn’t great either. Alcohol intake reduces clearance, exercise (especially cardiovascular exercise) improves it; omega-3 consumption improves it up a degree and does depend on omega-3/6 ratios, intermittent fasting improves it, and chronic stress worsens it.
And for a more pop-science presentation, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Clean Your Brain (Glymphatic Health Primer)
Take care!
Share This Post
-
Stop Checking Your Likes – by Susie Moore
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You might think this one’s advice is summed up sufficiently by the title, that there’s no need for a book! But…
There’s a lot more to this than “stop comparing the worst out-takes of your life to someone else’s highlight reel”, and there’s a lot more to this than “just unplug”.
Instead, Susie Moore discusses the serious underlying real emotional considerations of the need for approval (and even just acceptance) by our community, as well the fear of missing out.
It’s not just about how social media is designed to hijack various parts of our brain, or how The Alogorithm™ is out to personally drag your soul through Hell for a few more clicks; it’s also about the human element that would exist even without that. Who remembers MySpace? No algorithm in those days, but oh the drama potential for those “top 8 friends” places. And if you think that kind of problem is just for young people 20 years ago, you have mercifully missed the drama that older generations can get into on Facebook.
Along with the litany of evil, though, Moore also gives practical advice on how to overcome those things, how to “see the world through comedy-colored glasses”, how to ask “what’s missing, really?”, and how to make your social media experience work for you, rather than it merely using you as fuel. ← link is to our own related article!
Bottom line: if social media sucks a lot of your time, there may be more to it than just “social media sucks in general”, and there are ways to meet your emotional needs without playing by corporations’ rules to do so.
Click here to check out Stop Checking Your Likes, and breathe easy!
Share This Post
-
Lobster vs Crab – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing lobster to crab, we picked the crab.
Why?
Generally speaking, most seafood is healthy in moderation (assuming it’s well-prepared, not poisonous, and you don’t have an allergy), and for most people, these two sea creatures are indeed considered a reasonable part of a healthy balanced diet.
In terms of macros, they’re comparable in protein, and technically crab has about 2x the fat, but in both cases it’s next to nothing, so 2x almost nothing is still almost nothing. And, if we break down the lipids profiles, crab has a sufficiently smaller percentage of saturated fat (compared to monounsaturated and polyunsaturated), that crab actually has less saturated fat than lobster. In balance, the category of macros is either a tie or a slight win for crab, depending on your personal priorities.
When it comes to vitamins, crab wins easily with more of vitamins A, B1, B2, B6, B9, B12, and C, in most cases by considerable margins (we’re talking multiples of what lobster has). Lobster, meanwhile, has more of vitamin B3 (tiny margin) and vitamin B5 (pantothenic acid, as in, the vitamin that’s in basically everything edible, and thus almost impossible to be deficient in unless literally starving).
The minerals scene is more balanced; lobster has more calcium, copper, manganese, and selenium, while crab has more iron, magnesium, phosphorus, potassium, and zinc. The margins are comparable from one creature to another, so all in all the 4:5 score means a modest win for crab.
Both of these creatures are good sources of omega-3 fatty acids, but crab is better.
Lobster and crab are both somewhat high in cholesterol, but crab is the relatively lower of the two.
In short: for most people most of the time, both are fine to enjoy in moderation, but if picking one, crab is the healthier by most metrics.
Want to learn more?
You might like to read:
Shrimp vs Caviar – Which is Healthier?
Take care!
Share This Post
Related Posts
-
Pelvic Floor Exercises (Not Kegels!) To Prevent Urinary Incontinence
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a common threat, and if you think it couldn’t happen to you, then well, just wait. Happily, Dr. Christine Pieton, PT, DPT, a sport & women’s health physical therapist, has advice:
On the ball!
Or rather, we’re going to be doing ball-squeezing here, if you’ll pardon the expression. You will need a soccer-ball sized ball to squeeze.
Ball-squeeze breathing: lie on your back, ball between your knees, and inhale deeply, expanding your torso. Exhale, pressing your knees into the ball, engaging your abdominal muscles from lower to upper. Try to keep your spine long and avoid your pelvis tucking under during the exhalation.
Ball-squeeze bridge: lie on your back, ball between your knees, inhale to prepare, and then exhale, pressing up into a bridge, maintaining a firm pressure on the ball. Inhale as you lower yourself back down.
Ball-squeeze side plank: lie on your side this time, ball between your knees, supporting forearm under your shoulder, as in the video thumbnail. Inhale to prepare, and then exhale, lifting your hip a few inches off the mat. Inhale as you lower yourself back down.
Ball-squeeze bear plank: get on your hands and knees, ball between your thighs. Lengthen your spine, inhale to prepare, and exhale as you bring your knees just a little off the floor. Inhale as you lower yourself back down.
For more details and tips on each of these, plus a visual demonstration, plus an optional part 2 video with more exercises that aren’t ball-squeezes this time, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Psst… A Word To The Wise About UTIs
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Brain As A Work-In-Progress
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
And The Brain Goes Marching On!
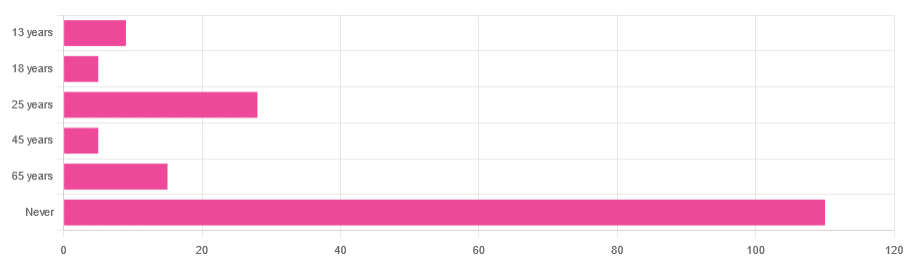
In Tuesday’s newsletter, we asked you “when does the human brain stop developing?” and got the above-depicted, below-described, set of responses:
- About 64% of people said “Never”
- About 16% of people said “25 years”
- About 9% of people said “65 years”
- About 5% of people said “13 years”
- About 3% of people said “18 years”
- About 3% of people said “45 years”
Some thoughts, before we get into the science:
An alternative wording for the original question was “when does the human brain finish developing”; the meaning is the same but the feeling is slightly different:
- “When does the human brain stop developing?” focuses attention on the idea of cessation, and will skew responses to later ages
- When does the human brain finish developing?” focuses on attention on a kind of “is it done yet?” and will skew responses to earlier ages
Ultimately, since we had to chose one word or another, we picked the shortest one, but it would have been interesting if we could have done an A/B test, and asked half one way, and half the other way!
Why we picked those ages
We picked those ages as poll options for reasons people might be drawn to them:
- 13 years: in English-speaking cultures, an important milestone of entering adolescence (note that the concept of a “teenager” is not precisely universal as most languages do not have “-teen” numbers in the same way; the concept of “adolescent” may thus be tied to other milestones)
- 18 years: age of legal majority in N. America and many other places
- 25 years: age popularly believed to be when the brain is finished developing, due to a study that we’ll talk about shortly (we guess that’s why there’s a spike in our results for this, too!)
- 45 years: age where many midlife hormonal changes occur, and many professionals are considered to have peaked in competence and start looking towards retirement
- 65 years: age considered “senior” in much of N. America and many other places, as well as the cut-off and/or starting point for a lot of medical research
Notice, therefore, how a lot of things are coming from places they really shouldn’t. For example, because there are many studies saying “n% of people over 65 get Alzheimer’s” or “n% of people over 65 get age-related cognitive decline”, etc, 65 becomes the age where we start expecting this—because of an arbitrary human choice of where to draw the cut-off for the study enrollment!
Similarly, we may look at common ages of legal majority, or retirement pensions, and assume “well it must be for a good reason”, and dear reader, those reasons are more often economically motivated than they are biologically reasoned.
So, what does the science say?
Our brains are never finished developing: True or False?
True! If we define “finished developing” as “we cease doing neurogenesis and neuroplasticity is no longer in effect”.
Glossary:
- Neurogenesis: the process of creating new brain cells
- Neuroplasticity: the process of the brain adapting to changes by essentially rebuilding itself to suit our perceived current needs
We say “perceived” because sometimes neuroplasticity can do very unhelpful things to us (e.g: psychological trauma, or even just bad habits), but on a biological level, it is always doing its best to serve our overall success as an organism.
For a long time it was thought that we don’t do neurogenesis at all as adults, but this was found to be untrue:
How To Grow New Brain Cells (At Any Age)
Summary of conclusions of the above: we’re all growing new brain cells at every age, even if we be in our 80s and with Alzheimer’s disease, but there are things we can do to enhance our neurogenic potential along the way.
Neuroplasticity will always be somewhat enhanced by neurogenesis (after all, new neurons get given jobs to do), and we reviewed a great book about the marvels of neuroplasticity including in older age:
Our brains are still developing up to the age of 25: True or False?
True! And then it keeps on developing after that, too. Now this is abundantly obvious considering what we just talked about, but see what a difference the phrasing makes? Now it makes it sound like it stops at 25, which this statement doesn’t claim at all—it only speaks for the time up to that age.
A lot of the popular press about “the brain isn’t fully mature until the age of 25” stems from a 2006 study that found:
❝For instance, frontal gray matter volume peaks at about age 11.0 years in girls and 12.1 years in boys, whereas temporal gray matter volume peaks at about age at 16.7 years in girls and 16.2 years in boys. The dorsal lateral prefrontal cortex, important for controlling impulses, is among the latest brain regions to mature without reaching adult dimensions until the early 20s.❞
Source: Structural Magnetic Resonance Imaging of the Adolescent Brain
There are several things to note here:
- The above statement is talking about the physical size of the brain growing
- Nowhere does he say “and stops developing at 25”
However… The study only looked at brains up to the age of 25. After that, they stopped looking, because the study was about “the adolescent brain” so there has to be a cut-off somewhere, and that was the cut-off they chose.
This is the equivalent of saying “it didn’t stop raining until four o’clock” when the reality is that four o’clock is simply when you gave up on checking.
The study didn’t misrepresent this, by the way, but the popular press did!
Another 2012 study looked at various metrics of brain development, and found:
- Synapse overproduction into the teens
- Cortex pruning into the late 20s
- Prefrontal pruning into middle age at least (they stopped looking)
- Myelination beyond middle age (they stopped looking)
Source: Experience and the developing prefrontal cortex ← check out figure 1, and make sure you’re looking at the human data not the rat data
So how’s the most recent research looking?
Here’s a 2022 study that looked at 123,984 brain scans spanning the age range from mid-gestation to 100 postnatal years, and as you can see from its own figure 1… Most (if not all) brain-things keep growing for life, even though most slow down at some point, they don’t stop:
Brain charts for the human lifespan ← check out figure 1; don’t get too excited about the ventricular volume column as that is basically “brain that isn’t being a brain”. Do get excited about the rest, though!
Want to know how not to get caught out by science being misrepresented by the popular press? Check out:
How Science News Outlets Can Lie To You (Yes, Even If They Cite Studies!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
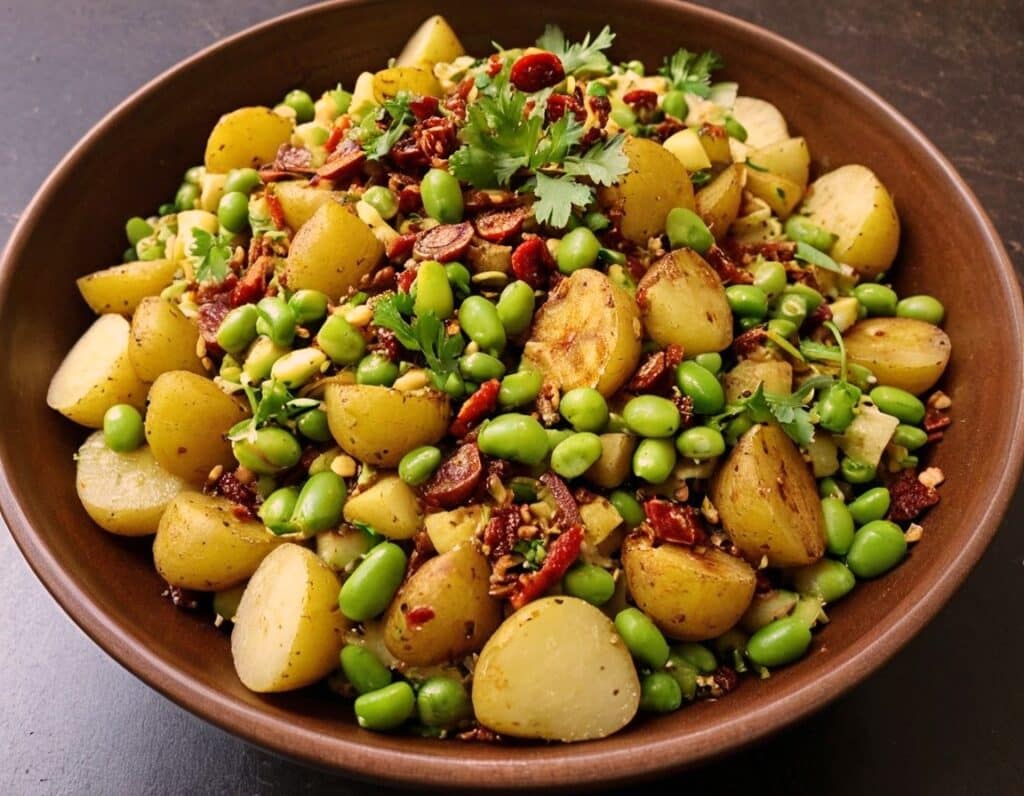
Chaat Masala Spiced Potato Salad With Beans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is an especially gut-healthy dish; the cooked-and-cooled potatoes are not rich with resistant starches (that’s good), the beans bring protein (as well as more fiber and micronutrients), and many of the spices bring their own benefits. A flavorful addition to your table!
You will need
- 1 lb new potatoes, boiled or steamed, with skin on, quartered, cooled ← this is a bit of a “mini recipe”, but we expect you can handle it
- 5 oz blanched broad beans
- 2 oz sun-dried tomatoes, chopped
- ¼ bulb garlic, crushed
- 1 tbsp extra virgin olive oil
- 2 tsp amchoor
- 2 tsp ground cumin
- 2 tsp ground coriander
- 1 tsp ground ginger
- 1 tsp ground asafoetida
- 1 tsp black pepper, coarse ground
- 1 tsp red chili powder
- 1 tsp ground turmeric
- ½ tsp MSG or 1 tsp low-sodium salt
- Juice of ½ lemon
And then…
- To garnish: finely chopped cilantro, or if you have the “cilantro tastes like soap” gene, then substitute with parsley
- To serve: a nice chutney; you can use our Spiced Fruit & Nut Chutney recipe
Method
(we suggest you read everything at least once before doing anything)
1) Mix all the ingredients from the main section, ensuring an even distribution on the spices.
2) Add the garnish, and serve with the chutney. That’s it. There was more work in the prep (and potentially, finding all the ingredients) today.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we scored all five today!
- Lycopene’s Benefits For The Gut, Heart, Brain, & More ← don’t underestimate those sun-dried tomatoes, either!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: