What Grief Does To Your Body (And How To Manage It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Grief Does To The Body (And How To Manage It)
In life, we will almost all lose loved ones and suffer bereavement. For most people, this starts with grandparents, eventually moves to parents, and then people our own generation; partners, siblings, close friends. And of course, sometimes and perhaps most devastatingly, we can lose people younger than ourselves.
For something that almost everyone suffers, there is often very little in the way of preparation given beforehand, and afterwards, a condolences card is nice but can’t do a lot for our mental health.
And with mental health, our physical health can go too, if we very understandably neglect it at such a time.
So, how to survive devastating loss, and come out the other side, hopefully thriving? It seems like a tall order indeed.
First, the foundations:
You’re probably familiar with the stages of grief. In their most commonly-presented form, they are:
- Denial
- Anger
- Bargaining
- Depression
- Acceptance
You’ve probably also heard/read that we won’t always go through them in order, and also that grief is deeply personal and proceeds on its own timescale.
It is generally considered healthy to go through them.
What do they look like?
Naturally this can vary a lot from person to person, but examples in the case of bereavement could be:
- Denial: “This surely has not really happened; I’ll carry on as though it hasn’t”
- Anger: “Why didn’t I do xyz differently while I had the chance?!”
- Bargaining: “I will do such-and-such in their honor, and this will be a way of expressing the love I wish I could give them in a way they could receive”
- Depression: “What is the point of me without them? The sooner I join them, the better.”
- Acceptance: “I was so lucky that we had the time together that we did, and enriched each other’s lives while we could”
We can speedrun these or we can get stuck on one for years. We can bounce back and forth. We can think we’re at acceptance, and then a previous stage will hit us like a tonne of bricks.
What if we don’t?
Assuming that our lost loved one was indeed a loved one (as opposed to someone we are merely societally expected to mourn), then failing to process that grief will tend to have a big impact on our life—and health. These health problems can include:
As you can see, three out of five of those can result in death. The other two aren’t great either. So why isn’t this taken more seriously as a matter of health?
Death is, ironically, considered something we “just have to live with”.
But how?
Coping strategies
You’ll note that most of the stages of grief are not enjoyable per se. For this reason, it’s common to try to avoid them—hence denial usually being first.
But, that is like not getting a lump checked out because you don’t want a cancer diagnosis. The emotional reasoning is understandable, but it’s ultimately self-destructive.
First, have a plan. If a death is foreseen, you can even work out this plan together.
But even if that time has now passed, it’s “better late than never” to make a plan for looking after yourself, e.g:
- How you will try to get enough sleep (tricky, but sincerely try)
- How you will remember to eat (and ideally, healthily)
- How you will still get exercise (a walk in the park is fine; see some greenery and get some sunlight)
- How you will avoid self-destructive urges (from indirect, e.g. drinking, to direct, e.g. suicidality)
- How you will keep up with the other things important in your life (work, friends, family)
- How you will actively work to process your grief (e.g. journaling, or perhaps grief counselling)
Some previous articles of ours that may help:
- How To Keep On Keeping On ← this is about looking after general health when motivation is low
- The Mental Health First-Aid You’ll Hopefully Never Need ← this is about managing depression
- How To Stay Alive (When You Really Don’t Want To) ← this is about managing suicidality
- Life After Death? (Your Life; A Loved One’s Death) ← this is about bereavement and romance
If it works, it works
If we are all unique, then any relationship between any two people is uniqueness squared. Little wonder, then, that our grief may be unique too. And it can be complicated further:
- Sometimes we had a complicated relationship with someone
- Sometimes the circumstances of their death were complicated
There is, for that matter, such a thing as “complicated grief”:
Read more: Complicated grief and prolonged grief disorder (Medical News Today)
We also previously reviewed a book on “ambiguous loss”, exploring grieving when we cannot grieve in the normal way because someone is gone and/but/maybe not gone.
For example, if someone is in a long-term coma from which they may never recover, or if they are missing-presumed-dead. Those kinds of situations are complicated too.
Unusual circumstances may call for unusual coping strategies, so how can we discern what is healthy and what isn’t?
The litmus test is: is it enabling you to continue going about your life in a way that allows you to fulfil your internal personal aspirations and external social responsibilities? If so, it’s probably healthy.
Look after yourself. And if you can, tell your loved ones you love them today.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Be 7.5x More Likely To Develop Chronic Fatigue Syndrome
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what is it?
Many more people have chronic fatigue, which is the symptom of being exhausted all the time, than have chronic fatigue syndrome (CFS) which is the illness of myalgic encephalomyelitis (ME).
This is because fatigue can be a symptom of many, many other conditions, and can be heavily influenced by lifestyle factors too.
A lot of the advice for dealing with chronic fatigue is often the same in both cases, but some will be different, because for example:
- If your fatigue is from some other condition, that condition probably impacts what lifestyle factors you are (and are not) able to change, too
- If your fatigue is from lifestyle factors, that hopefully means you can change those and enjoy less fatigue…
- But if it’s not from lifestyle factors, as in ME/CFS, then advice to “exercise more” etc is not going to help so much.
There are ways to know the difference though:
Check out: Do You Have Chronic Fatigue Syndrome?
The chronic disease pipeline
While it had been strongly suspected that COVID infection could lead to CFS, with long COVID having chronic fatigue as one of its characteristic symptoms, a research team led by Dr. Suzanne Vernon has now established the nature of the relationship.
It was a large (n=13,224) longitudinal observational cohort study of people with no pre-existing ME/CFS, grouped according to their COVID infection status:
- acute infected, enrolled within 30 days of infection or enrolled as uninfected who became infected (n=4,515)
- post-acute infected, enrolled greater than 30 days after infection (n=7,270)
- uninfected (n=1,439).
(to be clear, that last means “never infected”, or else they would be in group 2)
Note: people who had COVID and were hospitalized for it were excluded from the study, so this risk is the risk represented by even just more “moderate” infections.
What they found:
❝The proportion of all RECOVER-Adult participants that met criteria for ME/CFS following SARS-CoV-2 infection was 4.5% (531 of 11,785) compared to 0.6% (9 of 1439) in uninfected participants.❞
There are then different numbers if we look per 100 person-years, as the study also did—in which case, we get a re-modelled increase in risk of 5x instead of 7.5x, but a) that’s still not good b) the “here-and-now” figures of 4.5% vs 0.6% are also relevant.
Read in full: Incidence and Prevalence of Post-COVID-19 Myalgic Encephalomyelitis: A Report from the Observational RECOVER-Adult Study
The killer nobody wants to talk about anymore
Of course, as we all know the pandemic is over, because politicians declared it so, which is very reassuring.
Nevertheless, COVID is currently the still 4th leading cause of death in the US, placing it higher than stroke, Alzheimer’s, diabetes, and others.
See also: Emergency or Not, Covid Is Still Killing People. Here’s What Doctors Advise to Stay Safe
So, while it’s very good to take care of our hearts, brains, blood sugars, and so forth, let’s at the very least continue to keep on top of our vaccinations, avoid enclosed crowded spaces where possible, etc.
And for extra boosts to one’s chances: Why Some People Get Sick More (And How To Not Be One Of Them)
What if I do get (or already have) long COVID and/or ME/CFS?
Well, that is definitely going to suck, but there are still some things that can be done.
Here’s a big one: How To Eat To Beat Chronic Fatigue ← this will not, of course, cure you, but it’s a way of getting maximum nutrition for minimum effort, given that for someone with chronic fatigue, effort is a very finite resource that must be used sparingly
Finally, here are some further resources:
Support For Long COVID & Chronic Fatigue
Take care!
Share This Post
-
The Whys and Hows of Cutting Meats Out Of Your Diet
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it’s time to tell the meat to beat it…
Meat in general, and red meat and processed meat in particular, have been associated with so many health risks, that it’s very reasonable to want to reduce, if not outright eliminate, our meat consumption.
First, in case anyone’s wondering “what health risks?”
The aforementioned culprits tend to turn out to be a villain in the story of every second health-related thing we write about here. To name just a few:
- Processed Meat Consumption and the Risk of Cancer: A Critical Evaluation of the Constraints of Current Evidence from Epidemiological Studies
- Red Meat Consumption (Heme Iron Intake) and Risk for Diabetes and Comorbidities?
- Health Risks Associated with Meat Consumption: A Review of Epidemiological Studies
- Associations of Processed Meat, Unprocessed Red Meat, Poultry, or Fish Intake With Incident Cardiovascular Disease and All-Cause Mortality
- Meat consumption: Which are the current global risks? A review of recent (2010-2020) evidences
Seasoned subscribers will know that we rarely go more than a few days without recommending the very science-based Mediterranean Diet which studies find beneficial for almost everything we write about. The Mediterranean Diet isn’t vegetarian per se—by default it consists of mostly plants but does include some fish and a very small amount of meat from land animals. But even that can be improved upon:
- A Pesco-Mediterranean Diet With Intermittent Fasting
- Mediterranean, vegetarian and vegan diets as practical outtakes of EAS and ACC/AHA recommendations for lowering lipid profile
- A Mediterranean Low-Fat Vegan Diet to Improve Body Weight and Cardiometabolic Risk Factors: A Randomized, Cross-over Trial
So that’s the “why”; now for the “how”…
It’s said that with a big enough “why” you can always find a “how”, but let’s make things easy!
Meatless Mondays
One of the biggest barriers to many people skipping the meat is “what will we even eat?”
The idea of “Meatless Mondays” means that this question need only be answered once a week, and in doing that a few Mondays in a row, you’ll soon find you’re gradually building your repertoire of meatless meals, and finding it’s not so difficult after all.
Then you might want to expand to “meat only on the weekends”, for example.
Flexitarian
This can be met with derision, “Yes and I’m teetotal, apart from wine”, but there is a practical aspect here:
The idea is “I will choose vegetarian options, unless it’s really inconvenient for me to do so”, which wipes out any difficulty involved.
After doing this for a while, you might find that as you get more used to vegetarian stuff, it’s almost never inconvenient to eat vegetarian.
Then you might want to expand it to “I will choose vegan options, unless it’s really inconvenient for me to do so”
Like-for-like substitutions
Pretty much anything that can come from an animal, one can get a plant-based version of it nowadays. The healthiness (and cost!) of these substitutions can vary, but let’s face it, meat is neither the healthiest nor the cheapest thing out there these days either.
If you have the money and don’t fancy leaping to lentils and beans, this can be a very quick and easy zero-effort change-over. Then once you’re up and running, maybe you can—at your leisure—see what all the fuss is about when it comes to tasty recipes with lentils and beans!
That’s all we have time for today, but…
We’re thinking of doing a piece making your favorite recipes plant-based (how to pick the right substitutions so the meal still tastes and “feels” the same), so let us know if you’d like that? Feel free to mention your favorite foods/meals too, as that’ll help us know what there’s a market for!
You can do that by hitting reply to any of our emails, or using the handy feedback widget at the bottom!
Curious to know more while you wait?
Check out: The Vegan Diet: A Complete Guide for Beginners ← this is a well-sourced article from Healthline, who—just like us—like to tackle important health stuff in an easy-to-read, well-sourced format
Share This Post
-
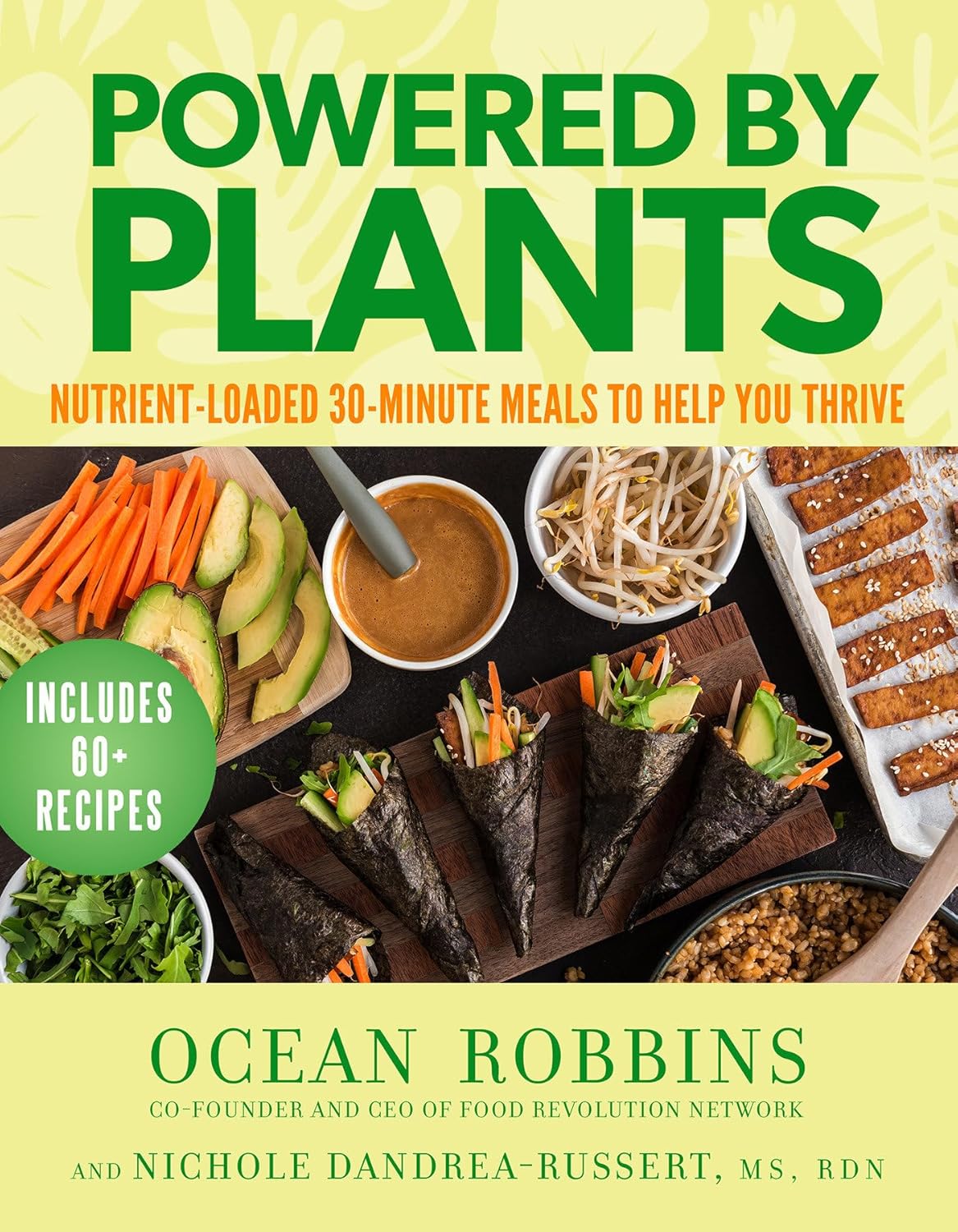
Powered by Plants – by Ocean Robbins & Nichole Dandrea-Russert
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Of the two authors, the former is a professional public speaker, and the latter is a professional dietician. As a result, we get a book that is polished and well-presented, while actually having a core of good solid science (backed up with plenty of references).
There’s an introductory section that’s all about the “notable nutrients”, that will be focused on in the ingredients choices for the recipes in the rest of the book.
The recipes themselves are simple enough to do quickly, yet interesting enough that you’ll want to do them, and certainly they contain all the plant-based nutrient-density you might expect.
Bottom line: if you’d like to expand your plant-based cooking with a focus on nutrition and ease without sacrificing fun, then this is a great cookbook for that.
Click here to check out Powered by Plants, and get powered by plants!
Share This Post
Related Posts
-
PCOS Repair Protocol – by Tamika Woods
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
PCOS (Polycystic Ovary Syndrome) affects about 1 in 5 women, and the general position of the medical establishment is “Oh dear, how sad; never mind”.
…which leaves a lot of people suffering with symptoms with little to no help.
This book looks to address that, and while it doesn’t claim to cure PCOS, it offers a system for managing (including: reducing) the symptoms. The author, a clinical nutritionist by academic background, tackles this in large part via being mindful about what one eats, in the context of the gut and endocrine system specifically.
It’s not just “have a gut healthy diet and eat foods with these nutrients”, though (although yes: also that). Rather, the author walks us through in-depth quizzes and lab testing advice, to advise the reader on how to understand the root cause of your PCOS symptoms, and then address each of those with an individualized management plan.
The style is on the low-end of pop-science, notwithstanding the clinically-informed content. For those who like a very chatty informal approach, you’ll find this one perfect. For those who don’t, well, you won’t find this one perfect, but you will most likely find it informative all the same.
Bottom line: if you or someone you care about (do you know 5 women?) has PCOS, the information in here could make a difference.
Click here to check out PCOS Repair Protocol, and suffer less!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hardcore Self Help: F**k Anxiety – by Dr. Robert Duff
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed other anxiety books before, so what makes this one different? Mostly, it’s the style.
Aside from swearing approximately once every two lines (so you might want to skip this one if that would bother you), Dr. Duff’s writing is very down-to-earth in other ways too, making it unpretentiously comfortable and accessible without failing to draw upon the wealth of good-practice, evidence-based advice he has to offer.
To that end, he talks about what anxiety is and isn’t, and goes over various approaches, explaining them in a “about” fashion, and also a “how to” fashion, covering areas such as CBT, somatic therapies, social support, when talk therapy is most likely to help.
The book is a quick read (a modest 74 pages), and it’s refreshing that it hasn’t been padded unnecessarily, unlike a lot of books that could have been a fraction of the size without losing value.
Bottom line: if you (or perhaps someone you care about) would benefit from a straight-to-the-point, no-BS approach to dealing with anxiety (that’s actually evidence-based, not just a “get over it” dismissal), then this is the book for you.
Click here to check out Hardcore Self Help: F**k Anxiety, and indeed do just that!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Getting to Neutral – by Trevor Moawad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We all know that a pessimistic outlook is self-defeating… And yet, toxic positivity can also be a set-up for failure! At some point, reckless faith in the kindly nature of the universe will get crushed, badly. Sometimes that point is a low point in life… sometimes it’s six times a day. But one thing’s for sure: we can’t “just decide everything will go great!” because the world just doesn’t work that way.
That’s where Trevor Moawad comes in. “Getting to neutral” is not a popular selling point. Everyone wants joy, abundance, and high after high. And neutrality itself is often associated with boredom and soullessness. But, Moawad argues, it doesn’t have to be that way.
This book’s goal—which it accomplishes well—is to provide a framework for being a genuine realist. What does that mean?
“I’m not a pessimist; I’m a realist” – every pessimist ever.
^Not that. That’s not what it means. What it means instead is:
- Hope for the best
- Prepare for the worst
- Adapt as you go
…taking care to use past experiences to inform future decisions, but without falling into the trap of thinking that because something happened a certain way before, it always will in the future.
To be rational, in short. Consciously and actively rational.
Feel the highs! Feel the lows! But keep your baseline when actually making decisions.
Bottom line: this book is as much an antidote to pessimism and self-defeat, as it is to reckless optimism and resultant fragility. Highly recommendable.
Click here to check out “Getting to Neutral” and start creating your best, most reason-based life!
PS: in this book, Moawad draws heavily from his own experiences of battling adversity in the form of cancer—of which he died, before this book’s publication. A poignant reminder that he was right: we won’t always get the most positive outcome of any given situation, so what matters the most is making the best use of the time we have.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: