How to be kind to yourself (without going to a day spa)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“I have to be hard on myself,” Sarah told me in a recent telehealth psychology session. “I would never reach my potential if I was kind and let myself off the hook.”
I could empathise with this fear of self-compassion from clients such as Sarah (not her real name). From a young age, we are taught to be kind to others, but self-kindness is never mentioned.
Instead, we are taught success hinges on self-sacrifice. And we need a healthy inner critic to bully us forward into becoming increasingly better versions of ourselves.
But research shows there doesn’t have to be a trade-off between self-compassion and success.
Self-compassion can help you reach your potential, while supporting you to face the inevitable stumbles and setbacks along the way.
What is self-compassion?
Self-compassion has three key ingredients.
1. Self-kindness
This involves treating yourself with the same kindness you would extend towards a good friend – via your thoughts, feelings and actions – especially during life’s difficult moments.
For instance, if you find yourself fixating on a minor mistake you made at work, self-kindness might involve taking a ten-minute walk to shift focus, and reminding yourself it is OK to make mistakes sometimes, before moving on with your day.
2. Mindfulness
In this context, mindfulness involves being aware of your own experience of stress or suffering, rather than repressing or avoiding your feelings, or over-identifying with them.
Basically, you must see your stress with a clear (mindful) perspective before you can respond with kindness. If we avoid or are consumed by our suffering, we lose perspective.
3. Common humanity
Common humanity involves recognising our own experience of suffering as something that unites us as being human.
For instance, a sleep-deprived parent waking up (for the fourth time) to feed their newborn might choose to think about all the other parents around the world doing exactly the same thing – as opposed to feeling isolated and alone.
It’s not about day spas, or booking a manicure
When Sarah voiced her fear that self-compassion would prevent her success, I explained self-compassion is distinct from self-indulgence.
“So is self-compassion just about booking in more mani/pedis?” Sarah asked.
Not really, I explained. A one-off trip to a day spa is unlikely to transform your mental health.
Instead, self-compassion is a flexible psychological resilience factor that shapes our thoughts, feelings and actions.
It’s associated with a suite of benefits to our wellbeing, relationships and health.

baranq/Shutterstock
What does the science say?
Over the past 20 years, we’ve learned self-compassionate people enjoy a wide range of benefits. They tend to be happier and have fewer psychological symptoms of distress.
Those high on self-compassion persevere following a failure. They say they are more motivated to overcome a personal weakness than those low on self-compassion, who are more likely to give up.
So rather than feeling trapped by your inadequacies, self-compassion encourages a growth mindset, helping you reach your potential.
However, self-compassion is not a panacea. It will not change your life circumstances or somehow make life “easy”. It is based on the premise that life is hard, and provides practical tools to cope.
It’s a factor in healthy ageing
I research menopause and healthy ageing and am especially interested in the value of self-compassion through menopause and in the second half of life.
Because self-compassion becomes important during life’s challenges, it can help people navigate physical symptoms (for instance, menopausal hot flushes), life transitions such as divorce, and promote healthy ageing.
I’ve also teamed up with researchers at Autism Spectrum Australia to explore self-compassion in autistic adults.
We found autistic adults report significantly lower levels of self-compassion than neurotypical adults. So we developed an online self-compassion training program for this at-risk population.
Three tips for self-compassion
You can learn self-compassion with these three exercises.
1. What would you say to a friend?
Think back to the last time you made a mistake. What did you say to yourself?
If you notice you’re treating yourself more like an enemy than a friend, don’t beat yourself up about it. Instead, try to think about what you might tell a friend, and direct that same friendly language towards yourself.
2. Harness the power of touch
Soothing human touch activates the parasympathetic “relaxation” branch of our nervous system and counteracts the fight or flight response.
Specifically, self-soothing touch (for instance, by placing both hands on your heart, stroking your forearm or giving yourself a hug) reduces cortisol responses to psychosocial stress.

http://krakenimages.com/Shutterstock
3. What do I need right now?
Sometimes, it can be hard to figure out exactly what self-compassion looks like in a given moment. The question “what do I need right now” helps clarify your true needs.
For example, when I was 37 weeks pregnant, I woke up bolt awake one morning at 3am.
Rather than beating myself up about it, or fretting about not getting enough sleep, I gently placed my hands on my heart and took a few deep breaths. By asking myself “what do I need right now?” it became clear that listening to a gentle podcast/meditation fitted the bill (even though I wanted to addictively scroll my phone).
Lydia Brown, Senior Lecturer in Psychology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Almonds vs Pecans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing almonds to pecans, we picked the almonds.
Why?
In terms of macros, almonds have more protein, carbs, and fiber, as well as the lower glycemic index. A strong start for almonds here, though pecans have more fat (and the healthy blend of fats is quite comparable from one nut to the other).
In the category of vitamins, almonds have more of vitamins B2, B3, B9, E, and choline, while pecans have more of vitamins A, B1, B5, B6, and K. Numerically that’s a tie, though the biggest margins of difference are for vitamins A and E, respectively, and we might want to prioritize almonds’ extra vitamin E, over pecans’ extra vitamin A, given that vitamin A is more easily found in large quantities in many foods, whereas vitamin E is not quite so abundant generally. So in short, either a tie or a slight win for almonds here.
When it comes to minerals, both contain a lot of goodness, but almonds have more calcium, iron, magnesium, phosphorus, potassium, and selenium, while pecans have more copper, manganese, and zinc. A clear win for almonds, though as we say, pecans are also great for this, just not as great as almonds.
As a side-note, both of these nuts have been found to have anticancer properties against breast cancer cell lines. In all likelihood this means they help against other cancers too, but breast cancer is what the extant research has been for.
So, naturally, enjoy either or both (in fact, both is ideal). But if you want to choose one for nutritional density, it’s almonds.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Share This Post
-
Triple Life Threat – by Donald R. Lyman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book takes a similar approach to “How Not To Die” (which we featured previously), but focussed specifically on three things, per the title: chronic pulmonary obstructive disease (CPOD), diabetes (type 2), and Alzheimer’s disease.
Lyman strikes a great balance of being both information-dense and accessible; there’s a lot of reference material in here, and the reader is not assumed to have a lot of medical knowledge—but we’re not patronized either, and this is an informative manual, not a sensationalized scaremongering piece.
All in all… if you have known risk factors for one or more of three diseases this book covers, the information within could well be a lifesaver.
Share This Post
-
The Whys and Hows of Cutting Meats Out Of Your Diet
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it’s time to tell the meat to beat it…
Meat in general, and red meat and processed meat in particular, have been associated with so many health risks, that it’s very reasonable to want to reduce, if not outright eliminate, our meat consumption.
First, in case anyone’s wondering “what health risks?”
The aforementioned culprits tend to turn out to be a villain in the story of every second health-related thing we write about here. To name just a few:
- Processed Meat Consumption and the Risk of Cancer: A Critical Evaluation of the Constraints of Current Evidence from Epidemiological Studies
- Red Meat Consumption (Heme Iron Intake) and Risk for Diabetes and Comorbidities?
- Health Risks Associated with Meat Consumption: A Review of Epidemiological Studies
- Associations of Processed Meat, Unprocessed Red Meat, Poultry, or Fish Intake With Incident Cardiovascular Disease and All-Cause Mortality
- Meat consumption: Which are the current global risks? A review of recent (2010-2020) evidences
Seasoned subscribers will know that we rarely go more than a few days without recommending the very science-based Mediterranean Diet which studies find beneficial for almost everything we write about. The Mediterranean Diet isn’t vegetarian per se—by default it consists of mostly plants but does include some fish and a very small amount of meat from land animals. But even that can be improved upon:
- A Pesco-Mediterranean Diet With Intermittent Fasting
- Mediterranean, vegetarian and vegan diets as practical outtakes of EAS and ACC/AHA recommendations for lowering lipid profile
- A Mediterranean Low-Fat Vegan Diet to Improve Body Weight and Cardiometabolic Risk Factors: A Randomized, Cross-over Trial
So that’s the “why”; now for the “how”…
It’s said that with a big enough “why” you can always find a “how”, but let’s make things easy!
Meatless Mondays
One of the biggest barriers to many people skipping the meat is “what will we even eat?”
The idea of “Meatless Mondays” means that this question need only be answered once a week, and in doing that a few Mondays in a row, you’ll soon find you’re gradually building your repertoire of meatless meals, and finding it’s not so difficult after all.
Then you might want to expand to “meat only on the weekends”, for example.
Flexitarian
This can be met with derision, “Yes and I’m teetotal, apart from wine”, but there is a practical aspect here:
The idea is “I will choose vegetarian options, unless it’s really inconvenient for me to do so”, which wipes out any difficulty involved.
After doing this for a while, you might find that as you get more used to vegetarian stuff, it’s almost never inconvenient to eat vegetarian.
Then you might want to expand it to “I will choose vegan options, unless it’s really inconvenient for me to do so”
Like-for-like substitutions
Pretty much anything that can come from an animal, one can get a plant-based version of it nowadays. The healthiness (and cost!) of these substitutions can vary, but let’s face it, meat is neither the healthiest nor the cheapest thing out there these days either.
If you have the money and don’t fancy leaping to lentils and beans, this can be a very quick and easy zero-effort change-over. Then once you’re up and running, maybe you can—at your leisure—see what all the fuss is about when it comes to tasty recipes with lentils and beans!
That’s all we have time for today, but…
We’re thinking of doing a piece making your favorite recipes plant-based (how to pick the right substitutions so the meal still tastes and “feels” the same), so let us know if you’d like that? Feel free to mention your favorite foods/meals too, as that’ll help us know what there’s a market for!
You can do that by hitting reply to any of our emails, or using the handy feedback widget at the bottom!
Curious to know more while you wait?
Check out: The Vegan Diet: A Complete Guide for Beginners ← this is a well-sourced article from Healthline, who—just like us—like to tackle important health stuff in an easy-to-read, well-sourced format
Share This Post
Related Posts
-
Water Water Everywhere, But Which Is Best To Drink?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Well Well Well…
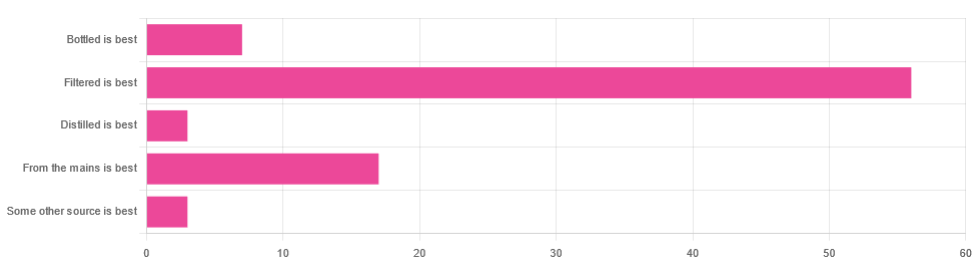
In Tuesday’s newsletter, we asked you for your (health-related) opinion on drinking water—with the understanding that this may vary from place to place. We got the above-depicted, below-described, set of responses:
- About 65% said “Filtered is best”
- About 20% said “From the mains is best”
- About 8% said “Bottled is best”
- About 3% said “Distilled is best”
- About 3% said “Some other source is best”
Of those who said “some other source is best”, one clarified that their preferred source was well water.
So what does the science say?
Fluoridated water is bad for you: True or False?
False, assuming a normal level of consumption. Rather than take up more space today though, we’ll link to what we previously wrote on this topic:
You may be wondering: but what if my level of consumption is higher than normal?
Let’s quickly look at some stats:
- The maximum permitted safety level varies from place to place, but is (for example) 2mg/l in the US, 1.5mg/l in Canada & the UK.
- The minimum recommended amount also varies from place to place, but is (for example) 0.7mg/l in Canada and the US, and 1mg/l in the UK.
It doesn’t take grabbing a calculator to realize that if you drink twice as much water as someone else, then depending on where you are, water fluoridated to the minimum may give you more than the recommended maximum.
However… Those safety margins are set so much lower than the actual toxicity levels of fluoride, that it doesn’t make a difference.
For example: your writer here takes a medication that has the side effect of causing dryness of the mouth, and consequently she drinks at least 3l of water per day in a climate that could not be described as hot (except perhaps for about 2 weeks of the year). She weighs 72kg (that’s about 158 pounds), and the toxicity of fluoride (for ill symptoms, not death) is 0.2mg/kg. So, she’d need 14.4mg of fluoride, which even if the water fluoridation here were 2mg/l (it’s not; it’s lower here, but let’s go with the highest figure to make a point), would require drinking more than 7l of water faster than the body can process it.
For more about the numbers, check out:
Acute Fluoride Poisoning from a Public Water System
Bottled water is the best: True or False?
False, if we consider “best” to be “healthiest”, which in turn we consider to be “most nutrients, with highest safety”.
Bottled water generally does have higher levels of minerals than most local mains supply water does. That’s good!
But you know what else is generally has? Microplastics and nanoplastics. That’s bad!
We don’t like to be alarmist in tone; it’s not what we’re about here, but the stats on bottled water are simply not good; see:
We Are Such Stuff As Bottles Are Made Of
You may be wondering: “but what about bottled water that comes in glass bottles?”
Indeed, water that comes in glass bottles can be expected to have lower levels of plastic than water that comes in plastic bottles, for obvious reasons.
However, we invite you to consider how likely you believe it to be that the water wasn’t stored in plastic while being processed, shipped and stored, before being portioned into its final store-ready glass bottles for end-consumer use.
Distilled water is the best: True or False?
False, generally, with caveats:
Distilled water is surely the safest water anywhere, because you know that you’ve removed any nasties.
However, it’s also devoid of nutrients, because you also removed any minerals it contained. Indeed, if you use a still, you’ll be accustomed to the build-up of these minerals (generally simplified and referenced as “limescale”, but it’s a whole collection of minerals).
Furthermore, that loss of nutrients can be more than just a “something good is missing”, because having removed certain ions, that water could now potentially strip minerals from your teeth. In practice, however, you’d probably have to swill it excessively to cause this damage.
Nevertheless, if you have the misfortune of living somewhere like Flint, Michigan, then a water still may be a fair necessity of life. In other places, it can simply be useful to have in case of emergency, of course.
Here’s an example product on Amazon if you’d like to invest in a water still for such cases.
PS: distilled water is also tasteless, and is generally considered bad, tastewise, for making tea and coffee. So we really don’t recommend distilling your water unless you have a good reason to do so.
Filtered water is the best: True or False?
True for most people in most places.
Let’s put it this way: it can’t logically be worse than whatever source of water you put into it…
Provided you change the filter regularly, of course.
Otherwise, after overusing a filter, at best it won’t be working, and at worst it’ll be adding in bacteria that have multiplied in the filter over however long you left it there.
You may be wondering: can water filters remove microplastics, and can they remove minerals?
The answer in both cases is: sometimes.
- For microplastics it depends on the filter size and the microplastic size (see our previous article for details on that).
- For minerals, it depends on the filter type. Check out:
The H2O Chronicles | 5 Water Filters That Remove Minerals
One other thing to think about: while most water filtration jugs are made of PFAS-free BPA-free plastics for obvious reasons, for greater peace of mind, you might consider investing in a glass filtration jug, like this one ← this is just one example product on Amazon; by all means shop around and find one you like
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Reduce Cortisol Levels Naturally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cortisol is a hormone that is important for us (we’d struggle to get up in the morning without it, for a start), but in this modern world we often have too much of it, too much of the time. How can we rebalance it? Dr. Mindy Pelz explains:
Lifestyle adjustments
A note in advance: the video makes frequent reference to things that “spike cortisol levels”, but this is probably intended as a stand-in for “raise cortisol levels”. Because, unlike for some things, in the case of cortisol, spikes aren’t usually a problem (indeed, they can be beneficial, and this is a large part of why cold showers and ice baths can be healthy; it’s an artificially induced cortisol spike, and this hormesis has an assortment of healthy benefits, each related to improving our body’s ability to switch quickly between states as appropriate); rather, it’s chronically high cortisol levels that are the problem. However, the video discusses things that can increase resting cortisol levels, so where she says “spike”, we suggest to read “raise”.
Dr. Pelz, an advocate of intermittent fasting, mentions that done incorrectly and/or for the same way for too long, fasting can raise cortisol levels and thus sabotage our efforts—so varying our fasting style can help avoid that. For example, 16:8, 5:2, longer fasts less frequently, etc.
On the topic of food, she also warns us of the dangers of ultra-processed food, harmful oils, and foods with added sugar, as these can all raise cortisol levels.
When it comes to exercise, she notes that intense exercise without adequate recovery can raise cortisol levels, so again it’s good to mix up one’s methods, vary one’s exercise routine, and allow each well-worked muscle-group adequate rest afterwards.
Dr. Pelz also talks mindset, and has her own interesting way of framing the well-established science that chronic stress means chronically high stress hormone (cortisol) levels; Dr. Pelz prefers to see it as negative vs positive thoughts, environments, etc.
Any discussion of cortisol management would be incomplete without discussing the importance of good quality sleep. Dr. Pelz doesn’t mention this at all in her video, but it’s important to bear in mind too!
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Lower Your Cortisol! (Here’s Why & How)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ideal Blood Pressure Numbers Explained
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Maybe I missed it but the study on blood pressure did it say what the 2 numbers should read ideally?❞
We linked it at the top of the article rather than including it inline, as we were short on space (and there was a chart rather than a “these two numbers” quick answer), but we have a little more space today, so:
Category Systolic (mm Hg) Diastolic (mm Hg) Normal < 120 AND < 80 Elevated 120 – 129 AND < 80 Stage 1 – High Blood Pressure 130 – 139 OR 80 – 89 Stage 2 – High Blood Pressure 140 or higher OR 90 or higher Hypertensive Crisis Above 180 AND/OR Above 120 To oversimplify for a “these two numbers” answer, under 120/80 is generally considered good, unless it is under 90/60, in which case that becomes hypotension.
Hypotension, the blood pressure being too low, means your organs may not get enough oxygen and if they don’t, they will start shutting down.
To give you an idea how serious this, this is the closed-circuit equivalent of the hypovolemic shock that occurs when someone is bleeding out onto the floor. Technically, bleeding to death also results in low blood pressure, of course, hence the similarity.
So: just a little under 120/80 is great.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: