How Not To Die – by Dr. Michael Greger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed this book some years ago, but we’re revisiting it now because:
- It really is a book that should be in every healthspan-enjoyer’s collection
- Our book reviews back then were not as comprehensive as now (though we still generally try to fit into the “it takes about one minute to read this review” idea, sometimes we’ll spend a little extra time).
Dr. Greger (of “Dr. Greger’s Daily Dozen” fame) outlines for us in cold hard facts and stats what’s most likely to be our cause of death. While this is not a cheery premise for a book, he then sets out to work back from there—what could have prevented those specific things?
Thus, while the book doesn’t confer immortality (the title is not “how to not die”, after all), it does teach us how not to die—i.e, from heart disease, lung diseases, brain diseases, digestive cancers, infections, diabetes, high blood pressure, liver disease, blood cancers, kidney disease, breast cancer, suicidal depression, prostate cancer, Parkinson’s disease, and even iatrogenic causes.
This it does with a lot of solid science, explained for the layperson, and/but without holding back when it comes to big words, and a lot of them, at that. If you want to add in daily exercises, just lifting the book could be a start; weighing in at 678 pages, it’s an information-dense tome that’s more likely to be sifted through than read cover-to-cover.
The style is thus dense science somewhat editorialized for lay readability, and well-evidenced with around 3,000 citations. That’s not a typo; there are 178 pages of bibliography at the back with about 15–20 scientific references per page.
In terms of practical use, he does also devote chapters to that, it’s not just all textbook. Indeed, he discusses the reasonings behind the items, portion sizes, and quantities of his “daily dozen” foods, so that the reader will understand how much bang-for-buck they deliver, and then it’ll seem a lot less like an arbitrary list, and more likely to be adopted and maintained.
Bottom line: if you care about not getting life-threatening illnesses (which at the end of the day, come to most people at some point), then this book is a must-read.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Ways To Naturally Boost The “Ozempic Effect”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Jason Fung is perhaps most well-known for his work in functional medicine for reversing diabetes, and he’s once again giving us sound advice about metabolic hormone-hacking with dietary tweaks:
All about incretin
As you may gather from the thumbnail, this video is about incretin, a hormone group (the most well-known of which is GLP-1, as in GLP-1 agonists like semaglutide drugs such as Ozempic, Wegovy, etc) that slows down stomach emptying, which means a gentler blood sugar curve and feeling fuller for longer. It also acts on the hypothalmus, controlling appetite via the brain too (signalling fullness and reducing hunger).
Dr. Fung recommends 5 ways to increase incretin levels:
- Enjoy dietary fat: healthy kinds, please (e.g. nuts, seeds, eggs, etc—not fried foods), but this increases incretin levels more than carbs
- Enjoy protein: again, prompts higher incretin levels of promotes satiety
- Enjoy fiber: this is more about slowing digestion, but when it’s fermented in the gut into short-chain fatty acids, those too increase incretin secretion
- Enjoy bitter foods: these don’t actually affect incretin levels, but they can bind to incretin receptors, making the body “believe” that you got more incretin (think of it like a skeleton key that fits the lock that was designed to be opened by a different key)
- Enjoy turmeric: for its curcumin content, which increases GLP-1 levels specifically
For more information on each of these, here’s Dr. Fung himself:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Semaglutide for Weight Loss?
- Ozempic vs Five Natural Supplements
- How To Prevent And Reverse Type 2 Diabetes ← this was our “Expert Insights” feature on Dr. Fung’s work
Take care!
Share This Post
-
To Err Is Human; To Forgive, Healthy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Forgive (And Why)
There’s an old saying that holding onto a grudge is like drinking poison and expecting the other person to die. If only it were so simple and easy as just choosing to let go!
But it’s not, is it?
When people have wronged us and/or wronged our loved ones, it’s hard to forgive, especially if they have not changed. For that matter, it can be hard to forgive ourselves for mistakes that we made, too.
Either way, “drinking that poison” can be close to literal, in terms of what harboring such anger and resentment can do for our cortisol levels.
So, what to do about it?
If you have a dialogue with the person, our previous article on communication may help a lot.
If you don’t, there are various other angles that can be taken:
The Unsent Letter
You can even send it, if you like, but it’s not the point here. The idea is to write to the person, expressing your grievances. But, (as per the above-linked article on communication) try to focus at least as much on your feelings as their actions. “When you did/said x, I felt y”, etc.
This is important for helping you process your feelings. If you send the letter, it’s also important for the other person to be able to understand your feelings.
Sometimes, we feel the things we do so strongly because we don’t have an outlet for them. Pouring out our emotions in such a fashion, on the other hand, means (to labor the metaphor) they’re no longer bottled up. Even just in and of itself, that can provide us a lot of relief.
And when we the negative emotions are no longer such high pressure, it can be easier to let go of them.
Mindfulness
Following on from the above idea, a good strategy can be simply sitting and feeling everything you need to feel, noticing it without judgement, like a curious observer.
Sometimes what we need is just to be heard, and that starts with hearing ourselves.
Compassion
There’s a Buddhist exercise that involves actively feeling compassion for three people: a loved one, a stranger, and an enemy. Many people report that it’s actually harder to feel compassion for a random stranger, than an enemy. Why? Because we don’t know them; we don’t know what’s good and bad about them in our estimation.
If you’re reading this because you want to be able to gain the peace of being able to forgive someone (even if that someone is yourself), then in at least some respect right now, that person is in the “enemy” category. So how do we unpack that?
To err is human. Everybody screws up sometimes. And also, everyone has a reason (or a complex of reasons) for acting the way they do. This does not mean that those reasons excuse the behavior, but it can explain it.
You don’t get angry at a storm for soaking you through. Even if you might not understand the physics of it in the way a meteorologist might, you understand that there were things that led to that, and you were just in the wrong place at the wrong time.
So why do we get angry at someone else for wronging us? Even if we might not understand the personal background of it in the way their psychologist or therapist might, we (hopefully) understand that there were things that caused them to be the way they were, and we were just in the wrong place at the wrong time.
And ourselves? We probably know, when we made a mistake, why we made it. Maybe we were afraid, insecure, reactive, forgetful, or too focused on some other thing. Whatever it was, we did our best at the time and, apparently, our best wasn’t as good as we’d like.
If we didn’t deserve forgiveness, we wouldn’t be critical of our past selves in the first place.
And, the science is very clear that it’s important for our health for other reasons besides cortisol management, too.
And as for others? They did the best they knew how. Maybe they were afraid, insecure, reactive, forgetful, or too focused on some other thing. Same story, different character.
Remembering that can be key to “accepting the apology we never received”.
Forgiving without forgetting
Developing the ability to forgive is a useful tool for our own mental health. It doesn’t mean we must or even should make ourselves a doormat.
“I forgive you” does not have to mean a clean slate; it means remembering that the thing happened, and just not holding on to the anger/resentment associated with it.
It may be water under the bridge now, but it might have been a devastatingly destructive wave at the time, and continuing to acknowledge truth that is sensible. Just, from a position of peace now, hopefully.
Share This Post
-
Are Waist Trainers Just A Waste, And Are Posture Fixers A Quick Fix?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are Waist Trainers Just A Waste, And Are Posture Fixers A Quick Fix?
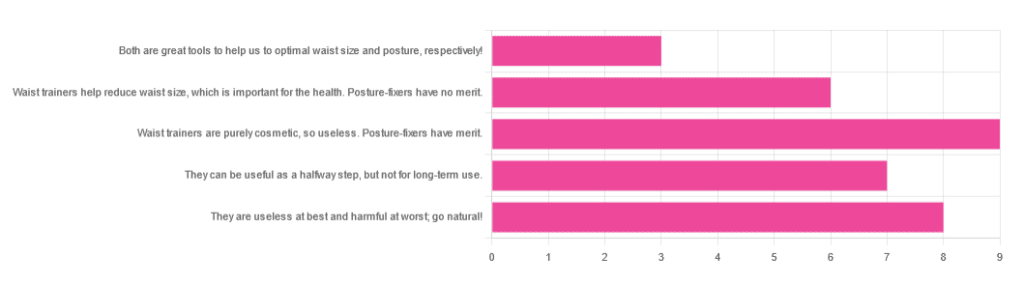
Yesterday, we asked you for your opinions on waist trainers and posture-fixing harnesses, and got the above-depicted, below-described set of results:
- The most popular response was “Waist trainers are purely cosmetic, so useless. Posture-fixers have merit”, with a little over a quarter of the votes.
- The least popular response was “Both are great tools to help us to optimal waist size and posture, respectively!”
- The other three answers each got a little under a quarter of the vote. In terms of discrete data, these were all 7±1, so basically, there was nothing in it.
The sample size was smaller than usual—perhaps the cluster of American holiday dates yesterday and today kept people busy! But, pressing on…
What does the science say?
Waist trainers are purely cosmetic, so, useless. True or False?
True, simply. Honestly, they’re not even that great for cosmetic purposes. They will indeed cinch in your middle, and this shape will be retained for a (very) short while after uncinching, because your organs have been squished inwards and may take a short while to get back to where they are supposed to be.
The American Board of Cosmetic Surgery may not be an unbiased source, but we’re struggling to find scientists who will even touch one of these, so, let’s see what these doctors have to say:
- Waist training can damage vital organs
- You will be slowly suffocating yourself
- Waist training simply doesn’t work
- You cannot drastically change your body shape with a piece of fabric*
Read: ABCS | 4 Reasons to Throw Your Waist Trainer in the Trash
*”But what about foot-binding?”—feet have many bones, whose growth can be physically restricted. Your waist has:
- organs: necessary! (long-term damage possible, but they’re not going away)
- muscles: slightly restrictable! (temporary restriction; no permanent change)
- fat: very squeezable! (temporary muffin; no permanent change)
Posture correctors have merit: True or False?
True—probably, and as a stepping-stone measure only.
The Ergonomics Health Association (a workplace health & safety organization) says:
❝Looking at the clinical evidence of posture correctors, we can say without a doubt that they do work, just not for everyone and not in the same way for all patients.❞
Source: Do Posture Correctors Work? Here’s What Our Experts Think
That’s not very compelling, so we looked for studies, and found… Not much, actually. However, what we did find supported the idea that “they probably do help, but we seriously need better studies with less bias”:
That is also not a compelling title, but here is where it pays to look at the studies and not just the titles. Basically, they found that the results were favorable to the posture-correctors—the science itself was just trash:
❝ The overall findings were that posture-correcting shirts change posture and subjectively have a positive effect on discomfort, energy levels and productivity.
The quality of the included literature was poor to fair with only one study being of good quality. The risk of bias was serious or critical for the included studies. Overall, this resulted in very low confidence in available evidence.❞
Since the benefit of posture correctors like this one is due to reminding the wearer to keep good posture, there is a lot more (good quality!) science for wearable biofeedback tech devices, such as this one:
Spine Cop: Posture Correction Monitor and Assistant
Take care!
Share This Post
Related Posts
-
The Immunostimulant Superfood
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Eat These Greens!
Chlorella vulgaris, henceforth “chlorella”, is a simple green algae that has a lot of health benefits.
Note: most of the studies here are for Chlorella vulgaris specifically. However, some are for other species of the Chlorella genus, of which Chlorella vulgaris is by far the most common, hence the name (vulgaris = common). The relevant phytochemical properties appear to be the same regardless.
Superfood
While people generally take it as a supplement rather than a food item in any kind of bulk, it is more than 50% protein and contains all 9 essential amino acids.
As you might expect of a green superfood, it’s also full of many antioxidants, most of them carotenoids, and these pack a punch, for example against cancer:
It also has a lot of vitamins and minerals, and even omega-3.
Which latter also means it helps improve lipids and is thus particularly…
Heart healthy
❝Daily consumption of Chlorella supplements provided the potential of health benefits reducing serum lipid risk factors, mainly triglycerides and total cholesterol❞
Its heart-healthy benefits don’t stop at lipids though, and include blood pressure management, as in this study that found…
❝GABA-rich Chlorella significantly decreased high-normal blood pressure and borderline hypertension, and is a beneficial dietary supplement for prevention of the development of hypertension. ❞
About that GABA, if you’re curious about that, check out:
GABA Against Stress, Anxiety, & More
May remove heavy metals
We’re going with “may” for this one as we could only find animal studies so far (probably because most humans don’t have megadoses of heavy metals in them, which makes testing harder).
Here’s an example animal study, though:
Enhanced elimination of tissue methyl mercury in [Chlorella]-fed mice
Immunostimulant
This one’s clearer, for example in this 8-week study (with humans) that found…
❝Serum concentrations of interferon-γ (p<0.05) and interleukin-1β (p<0.001) significantly increased and that of interleukin-12 (p<0.1) tended to increase in the Chlorella group.
The increments of these cytokines after the intervention were significantly bigger in the Chlorella group than those in the placebo group. In addition, NK cell activities (%) were significantly increased in Chlorella group, but not in Placebo group.
The increments of NK cell activities (%) were also significantly bigger in the Chlorella group than the placebo group.
Additionally, changed levels of NK cell activity were positively correlated with those of serum interleukin-1β (r=0.280, p=0.047) and interferon-γ (r=0.271, p<0.005).❞
tl;dr = it boosts numerous different kinds of immune cells
PS, if you click though to the study, you may be momentarily alarmed by the first paragraph of the abstract that says “However, there were no direct evidences for the effect of Chlorella supplementation on immune/inflammation response in healthy humans“
this is from the “Background” section of the abstract, so what they are saying is “before we did this study, nobody had done this yet”.
So, be assured that the results are worthwhile and compelling.
Is it safe?
Based on the studies, it has a good safety profile. However, as it boosts the immune system, you may want to check with your doctor if you have an autoimmune disorder, and/or you are on immunosuppressants.
And in general, of course always check with your doctor/pharmacist if unsure about any potential drug interactions.
Want some?
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Forks Over Knives: Flavor! – by Darshana Thacker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s important to not have to choose too much between health and flavor, because the outcome will never be a good one, either for your health or your happiness. And what’s bad for your happiness will ultimately not work out and thus will be bad for your general health, so, the question becomes: how to get both?
This book handles that nicely, delivering plant-based dishes that are also incidentally oil-free, and also either gluten-free or else there’s an obvious easy substitution to make it such. The flavor here comes from the ingredients as a whole, including the main ingredients as well as seasonings.
On the downside, occasionally those ingredients may be a little obscure if you don’t live in, say, San Francisco, and the ingredients weren’t necessarily chosen for cooking on a budget, either.
However, in most cases for most people it will, at worse, inspire you to try using an ingredient you don’t usually use—so that’s a good result.
The recipes are very clear and easy to follow, although not all are illustrated, and the “ready in…” times are about as accurate as they are for any cookbook, that is to say, it’s the time in which it conceivably can be done if (like the author, a head chef) you have a team of sous-chefs who have done a bunch of prep for you (e.g. sweet potato does not normally come in ½” dice; it comes in sweet potatoes) and laid everything out in little bowls mise-en-place style, and also you know the procedure well enough to not have to stop, hesitate, check anything, wash anything, wait for water to boil or anything else to heat up, or so forth. In other words, if you’re on your own in your home kitchen with normal domestic appliances, it’s going to take a little longer than for a professional in a professional kitchen with professional help.
But don’t let that detract from the honestly very good recipes.
Bottom line: if you’d like to level-up your plant-based cooking, this will definitely make your dishes that bit better!
Click here to check out Forks Over Knives: Flavor!, and dig in!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
ADHD… As An Adult?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ADHD—not just for kids!
Consider the following:
- If a kid has consistent problems paying attention, it’s easy and common to say “Aha, ADHD!”
- If a young adult has consistent problems paying attention, it’s easy and common to say “Aha, a disinterested ne’er-do-well!”
- If an older adult has consistent problems paying attention, it’s easy and common to say “Aha, a senior moment!”
Yet, if we recognize that ADHD is fundamentally a brain difference in children (and we do; there are physiological characteristics that we can test), and we can recognize that as people get older our brains typically have less neuroplasticity (ability to change) than when we are younger rather than less, then… Surely, there are just as many adults with ADHD as kids!
After all, that rather goes with the linear nature of time and the progressive nature of getting older.
So why do kids get diagnoses so much more often than adults?
Parents—and schools—can find children’s ADHD challenging, and it’s their problem, so they look for an explanation, and ADHD isn’t too difficult to find as a diagnosis.
Meanwhile, adults with ADHD have usually developed coping mechanisms, have learned to mask and/or compensate for their symptoms, and we expect adults to manage their own problems, so nobody’s rushing to find an explanation on their behalf.
Additionally, the stigma of neurodivergence—especially something popularly associated with children—isn’t something that many adults will want for themselves.
But, if you have an ADHD brain, then recognizing that (even if just privately to yourself) can open the door to much better management of your symptoms… and your life.
So what does ADHD look like in adults?
ADHD involves a spread of symptoms, and not everyone will have them all, or have them in the same magnitude. However, very commonly most noticeable traits include:
- Lack of focus (ease of distraction)
- Conversely: high focus (on the wrong things)
- To illustrate: someone with ADHD might set out to quickly tidy the sock drawer, and end up Marie Kondo-ing their entire wardrobe… when they were supposed to doing something else
- Conversely: high focus (on the wrong things)
- Poor time management (especially: tendency to procrastinate)
- Forgetfulness (of various kinds—for example, forgetting information, and forgetting to do things)
Want To Take A Quick Test? Click Here ← this one is reputable, and free. No sign in required; the test is right there.
Wait, where’s the hyperactivity in this Attention Deficit Hyperactivity Disorder?
It’s often not there. ADHD is simply badly-named. This stems from how a lot of mental health issues are considered by society in terms of how much they affect (and are observable by) other people. Since ADHD was originally noticed in children (in fact being originally called “Hyperkinetic Reaction of Childhood”), it ended up being something like:
“Oh, your brain has an inconvenient relationship with dopamine and you are driven to try to correct that by shifting attention from boring things to stimulating things? You might have trouble-sitting-still disorder”
Hmm, this sounds like me (or my loved one); what to do now at the age of __?
Some things to consider:
- If you don’t want medication (there are pros and cons, beyond the scope of today’s article), you might consider an official diagnosis not worth pursuing. That’s fine if so, because…
- More important than whether or not you meet certain diagnostic criteria, is whether or not the strategies recommended for it might help you.
- Whether or not you talk to other people about it is entirely up to you. Maybe it’s a stigma you’d rather avoid… Or maybe it’ll help those around you to better understand and support you.
- Either way, you might want to learn more about ADHD in adults. Today’s article was about recognizing it—we’ll write more about managing it another time!
In the meantime… We recommended a great book about this a couple of weeks ago; you might want to check it out:
Click here to see our review of “The Silent Struggle: Taking Charge of ADHD in Adults”!
Note: the review is at the bottom of that page. You’ll need to scroll past the video (which is also about ADHD) without getting distracted by it and forgetting you were there to see about the book. So:
- Click the above link
- Scroll straight to the review!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: