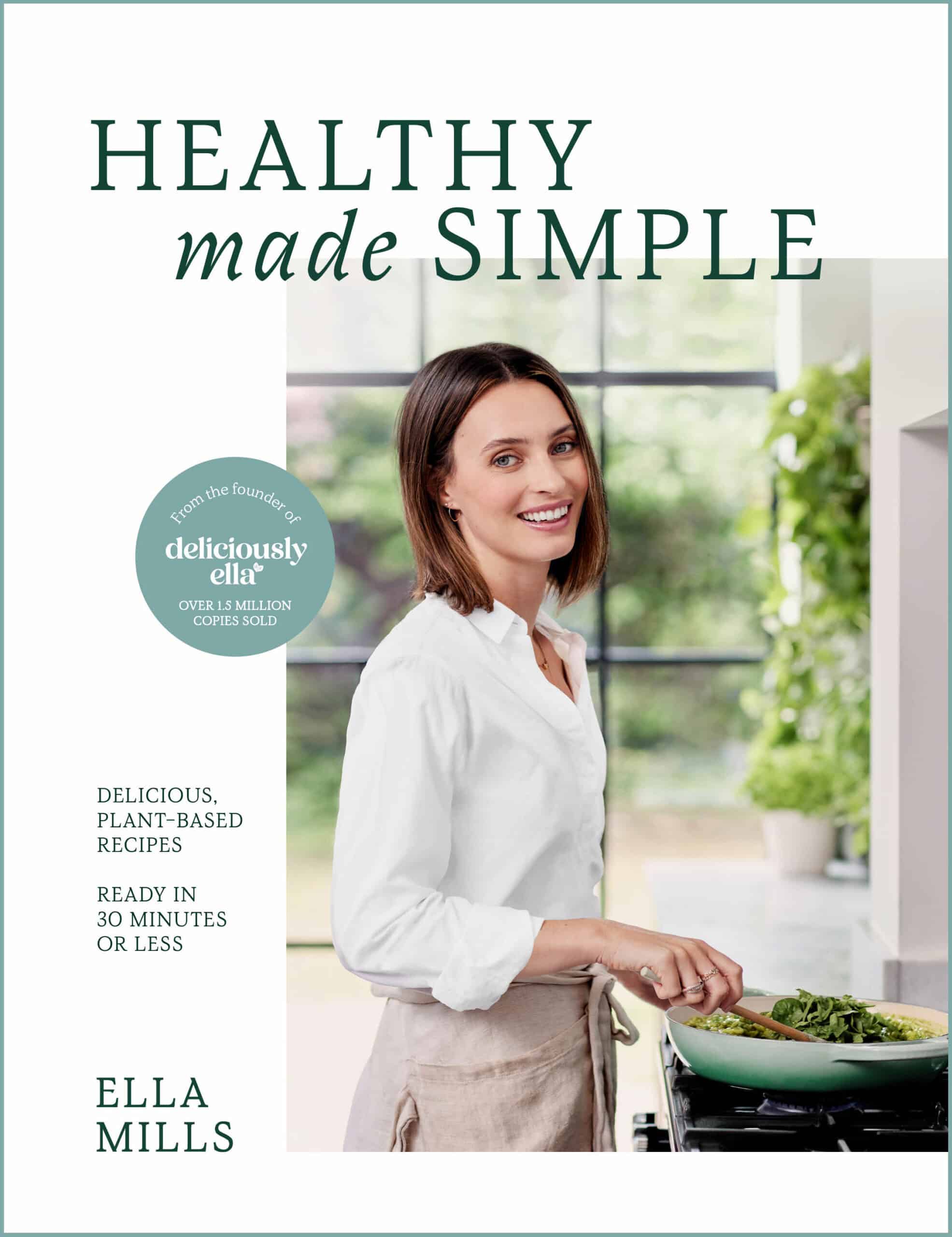
Healthy Made Simple – by Ella Mills
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Often, cookbooks leave a gap between “add the beans to the rice, then microwave” and “delicately embarrass the green-shooted scallions with assiduous garlic before adding to the matelote of orrazata flamed in Sapient Pear Brandy”. This book fills that gap:
It has dishes good for entertaining, and dishes good for eating on a Tuesday night after a long day. Sometimes, they’re even the same dishes.
It has a focus on what’s pleasing, easy, healthy, and consistent with being cooked in a real home kitchen for real people.
The book offers 75 recipes that:
- Take under 30 minutes to make*
- Contain 10 ingredients or fewer
- Have no more than 5 steps
- Are healthy and packed with goodness
- Are delicious and flavorful
*With a selection for under 15 minutes, too!
A strength of the book is that it’s based on practical, real-world cooking, and as such, there are sections such as “Prep-ahead [meals]”, and “cook once, eat twice”, etc.
Just because one is cooking with simple fresh ingredients doesn’t mean that everything bought today must be used today!
Bottom line: if you’d like simple, healthy recipe ideas that lend themselves well to home-cooking and prepping ahead / enjoying leftovers the next day, this is an excellent book for you.
Click here to check out Healthy Made Simple, enjoy the benefits to your health, the easy way!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Avoid Carer Burnout (Without Dropping Care)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Avoid Carer Burnout
Sometimes in life we find ourselves in a caregiving role.
Maybe we chose it. For example, by becoming a professional carer, or even just by being a parent.
Oftentimes we didn’t. Sometimes because our own parents now need care from us, or because a partner becomes disabled.
Philosophical note: an argument could be made for that latter also having been a pre-emptive choice; we probably at some point said words to the effect of “in sickness and in health”, hopefully with free will, and hopefully meant it. And of course, sometimes we enter into a relationship with someone who is already disabled.
But, we are not a philosophy publication, and will henceforth keep to the practicalities.
First: are you the right person?
Sometimes, a caregiving role might fall upon you unasked-for, and it’s worth considering whether you are really up for it. Are you in a position to be that caregiver? Do you want to be that caregiver?
It may be that you do, and would actively fight off anyone or anything that tried to stop you. If so, great, now you only need to make sure that you are actually in a position to provide the care in question.
It may be that you do want to, but your circumstances don’t allow you to do as good a job of it as you’d like, or it means you have to drop other responsibilities, or you need extra help. We’ll cover these things later.
It may be that you don’t want to, but you feel obliged, or “have to”. If that’s the case, it will be better for everyone if you acknowledge that, and find someone else to do it. Nobody wants to feel a burden, and nobody wants someone providing care to be resentful of that. The result of such is two people being miserable; that’s not good for anyone. Better to give the job to someone who actually wants to (a professional, if necessary).
So, be honest (first with yourself, then with whoever may be necessary) about your own preferences and situation, and take steps to ensure you’re only in a caregiving role that you have the means and the will to provide.
Second: are you out of your depth?
Some people have had a life that’s prepared them for being a carer. Maybe they worked in the caring profession, maybe they have always been the family caregiver for one reason or another.
Yet, even if that describes you… Sometimes someone’s care needs may be beyond your abilities. After all, not all care needs are equal, and someone’s condition can (and more often than not, will) deteriorate.
So, learn. Learn about the person’s condition(s), medications, medical equipment, etc. If you can, take courses and such. The more you invest in your own development in this regard, the more easily you will handle the care, and the less it will take out of you.
And, don’t be afraid to ask for help. Maybe the person knows their condition better than you, and certainly there’s a good chance they know their care needs best. And certainly, there are always professionals that can be contacted to ask for advice.
Sometimes, a team effort may be required, and there’s no shame in that either. Whether it means enlisting help from family/friends or professionals, sometimes “many hands make light work”.
Check out: Caregiver Action Network: Organizations Near Me
A very good resource-hub for help, advice, & community
Third: put your own oxygen mask on first
Like the advice to put on one’s own oxygen mask first before helping others (in the event of a cabin depressurization in an airplane), the rationale is the same here. You can’t help others if you are running on empty yourself.
As a carer, sometimes you may have to put someone else’s needs above yours, both in general and in the moment. But, you do have needs too, and cannot neglect them (for long).
One sleepless night looking after someone else is… a small sacrifice for a loved one, perhaps. But several in a row starts to become unsustainable.
Sometimes it will be necessary to do the best you can, and accept that you cannot do everything all the time.
There’s a saying amongst engineers that applies here too: “if you don’t schedule time for maintenance, your equipment will schedule it for you”.
In other words: if you don’t give your body rest, your body will break down and oblige you to rest. Please be aware this goes for mental effort too; your brain is just another organ.
So, plan ahead, schedule breaks, find someone to take over, set up your cared-for-person with the resources to care for themself as well as possible (do this anyway, of course—independence is generally good so far as it’s possible), and make the time/effort to get you what you need for you. Sleep, distraction, a change of scenery, whatever it may be.
Lastly: what if it’s you?
If you’re reading this and you’re the person who has the higher care needs, then firstly:all strength to you. You have the hardest job here; let’s not forget that.
About that independence: well-intentioned people may forget that, so don’t be afraid to remind them when “I would prefer to do that myself”. Maintaining independence is generally good for the health, even if sometimes it is more work for all concerned than someone else doing it for you. The goal, after all, is your wellbeing, so this shouldn’t be cast aside lightly.
On the flipside: you don’t have to be strong all the time; nobody should.
Being disabled can also be quite isolating (this is probably not a revelation to you), so if you can find community with other people with the same or similar condition(s), even if it’s just online, that can go a very, very long way to making things easier. Both practically, in terms of sharing tips, and psychologically, in terms of just not feeling alone.
See also: How To Beat Loneliness & Isolation
Share This Post
-
Foods For Managing Hypothyroidism (incl. Hashimoto’s)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Foods for Managing Hypothyroidism
For any unfamiliar, hypothyroidism is the condition of having an underactive thyroid gland. The thyroid gland lives at the base of the front of your neck, and, as the name suggests, it makes and stores thyroid hormones. Those are important for many systems in the body, and a shortage typically causes fatigue, weight gain, and other symptoms.
What causes it?
This makes a difference in some cases to how it can be treated/managed. Causes include:
- Hashimoto’s thyroiditis, an autoimmune condition
- Severe inflammation (end result is similar to the above, but more treatable)
- Dietary deficiencies, especially iodine deficiency
- Secondary endocrine issues, e.g. pituitary gland didn’t make enough TSH for the thyroid gland to do its thing
- Some medications (ask your pharmacist)
We can’t do a lot about those last two by leveraging diet alone, but we can make a big difference to the others.
What to eat (and what to avoid)
There is nuance here, which we’ll go into a bit, but let’s start by giving the
one-linetwo-line summary that tends to be the dietary advice for most things:- Eat a nutrient-dense whole-foods diet (shocking, we know)
- Avoid sugar, alcohol, flour, processed foods (ditto)
What’s the deal with meat and dairy?
- Meat: avoid red and processed meats; poultry and fish are fine or even good (unless fried; don’t do that)
- Dairy: limit/avoid milk; but unsweetened yogurt and cheese are fine or even good
What’s the deal with plants?
First, get plenty of fiber, because that’s important to ease almost any inflammation-related condition, and for general good health for most people (an exception is if you have Crohn’s Disease, for example).
If you have Hashimoto’s, then gluten (as found in wheat, barley, and rye) may be an issue, but the jury is still out, science-wise. Here’s an example study for “avoid gluten” and “don’t worry about gluten”, respectively:
- The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Women with Hashimoto’s Thyroiditis
- Doubtful Justification of the Gluten-Free Diet in the Course of Hashimoto’s Disease
So, you might want to skip it, to be on the safe side, but that’s up to you (and the advice of your nutritionist/doctor, as applicable).
A word on goitrogens…
Goitrogens are found in cruciferous vegetables and soy, both of which are very healthy foods for most people, but need some extra awareness in the case of hypothyroidism. This means there’s no need to abstain completely, but:
- Keep serving sizes small, for example a 100g serving only
- Cook goitrogenic foods before eating them, to greatly reduce goitrogenic activity
For more details, reading even just the abstract (intro summary) of this paper will help you get healthy cruciferous veg content without having a goitrogenic effect.
(as for soy, consider just skipping that if you suffer from hypothyroidism)
What nutrients to focus on getting?
- Top tier nutrients: iodine, selenium, zinc
- Also important: vitamin B12, vitamin D, magnesium, iron
Enjoy!
Share This Post
-
Dealing with Thirst!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Busting The Myth of “Eight Glasses Of Water A Day”
Everyone knows we must drink 8 glasses of water a day, or else we’re going to get a failing grade at being a healthy human—like not flossing, or not using adequate sunscreen.
But… Do we? And does tea count? How about (we dare but whisper it) coffee? And soda drinks are mostly water, right? But aren’t some drinks dehydrating? Are special electrolyte drinks really better? There are so many things to consider, so many differing advices, and it’s easy to give up, or just choose what to believe in as a leap of faith.
A quick brain-teaser for you first, though:
If coffee and soda don’t count because they’re dehydrating, then what if you were to take:
– A concentrated tiny cup of espresso, and then a glass of water, would the glass of water count?
– Or (we don’t relish the thought) what if you took a spoonful of soda syrup, and then a glass of water, would the glass of water count?
If your answer was “yes, it’s a glass of water”, then why would it not count if it were taken all at once (e.g. as an Americano coffee, or a regular soda)?
If your answer was “yes, but that water might only offset the dehydration caused by the coffee/syrup, so I might only be breaking even”, then you were thinking about this the right way:
How much water you need depends on many factors that can be affected by what else you are consuming and what else you are doing. Science loves averages, so eight glasses a day may be great if you are of average health, and average body size, in a temperate climate, doing moderate exercise, and so on and so on.
If you’re not the most average person of all time? You may need to take into account a lot of factors, ranging from what you ate for dinner to how much you perspired during your morning exercises. As you (probably) don’t live in laboratory conditions, this can become an impossible task—and if you missed (or guessed incorrectly) even one factor, the whole calculation will be thrown off. But is there any other way to know?
What of the infamous pee test? Drink enough to make your urine as clear as possible, and if it’s dark, you’re dehydrated, common wisdom says.
In reality, however, that tells you not what’s in your body, but rather, what got ejected from your body. If your urine is dark, it might mean you had too little water, but it also could just mean you had the right amount of water but too much sodium, for instance. A study of this was done on athletes, and found no correlation between urine color and actual bodily hydration when measured directly via a blood test.
So, if we can’t just have an app tell us “drink this many glasses of water”, and we can’t trust urine color, what can we do?
What we can do is trust that our body comes with (for free!) a wonderful homeostatic system and it will try to correct any imbalances. If you are thirsty, you’re dehydrated. Drink something with plenty of water in, if not plain water.
But what about special electrolyte drinks? If you need salts, you will crave them. Craving a salty snack? Go for it! Or if you prefer not to snack, do a salt lick test (just put a little salt on your finger, and taste it; if it tastes good, wait a minute or two, and then have a little more, and repeat until it doesn’t).
Bonus Tip:
- Make sure you always have a source of hydration (that you enjoy!) to hand. Maybe it’s chilled water, maybe it’s a pot of tea, maybe it’s a sports drink, it doesn’t matter too much. Even coffee is actually fine, by the way (but don’t overdo it).
- Make a personal rule: “I will always make time for hydration”. That means, if you’re thirsty, have something with water in it now. Not when you’ve finished what you’re doing (unless you really can’t stop, because you are a racecar driver mid-race, or a surgeon mid-operation, or something), but now. Do not postpone it until after you’ve done some other thing first; you will forget and it will keep getting postponed. Always make time for water.
Share This Post
Related Posts
-
Eyes for Alzheimer’s Diagnosis: New?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Time!
This is the bit whereby each week, we respond to subscriber questions/requests/etc
Have something you’d like to ask us, or ask us to look into? Hit reply to any of our emails, or use the feedback widget at the bottom, and a Real Human™ will be glad to read it!
Q: As I am a retired nurse, I am always interested in new medical technology and new ways of diagnosing. I have recently heard of using the eyes to diagnose Alzheimer’s. When I did some research I didn’t find too much. I am thinking the information may be too new or I wasn’t on the right sites.
(this is in response to last week’s piece on lutein, eyes, and brain health)
We’d readily bet that the diagnostic criteria has to do with recording low levels of lutein in the eye (discernible by a visual examination of macular pigment optical density), and relying on the correlation between this and incidence of Alzheimer’s, but we’ve not seen it as a hard diagnostic tool as yet either—we’ll do some digging and let you know what we find! In the meantime, we note that the Journal of Alzheimer’s Disease (which may be of interest to you, if you’re not already subscribed) is onto this:
See also:
- Journal of Alzheimer’s Disease (mixture of free and paid content)
- Journal of Alzheimer’s Disease Reports (open access—all content is free)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Black Pepper’s Impressive Anti-Cancer Arsenal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
Piperine, a compound found in Piper nigrum (black pepper, to its friends), has many health benefits. It’s included as a minor ingredient in some other supplements, because it boosts bioavailability. In its form as a kitchen spice, it’s definitely a superfood.
What does it do?
First, three things that generally go together:
These things often go together for the simple reason that oxidative stress, inflammation, and cancer often go together. In each case, it’s a matter of cellular wear-and-tear, and what can mitigate that.
For what it’s worth, there’s generally a fourth pillar: anti-aging. This is again for the same reason. That said, black pepper hasn’t (so far as we could find) been studied specifically for its anti-aging properties, so we can’t cite that here as an evidence-based claim.
Nevertheless, it’s a reasonable inference that something that fights oxidation, inflammation, and cancer, will often also slow aging.
Special note on the anti-cancer properties
We noticed two very interesting things while researching piperine’s anti-cancer properties. It’s not just that it reduces cancer risk and slows tumor growth in extant cancers (as we might expect from the above-discussed properties). Let’s spotlight some studies:
It is selectively cytotoxic (that’s a good thing)
Piperine was found to be selectively cytotoxic to cancerous cells, while not being cytotoxic to non-cancerous cells. To this end, it’s a very promising cancer-sniper:
Piperine as a Potential Anti-cancer Agent: A Review on Preclinical Studies
It can reverse multi-drug resistance in cancer cells
P-glycoprotein, found in our body, is a drug-transporter that is known for “washing out” chemotherapeutic drugs from cancer cells. To date, no drug has been approved to inhibit P-glycoprotein, but piperine has been found to do the job:
Targeting P-glycoprotein: Investigation of piperine analogs for overcoming drug resistance in cancer
What’s this about piperine analogs, though? Basically the researchers found a way to “tweak” piperine to make it even more effective. They called this tweaked version “Pip1”, because calling it by its chemical name,
((2E,4E)-5-(benzo[d][1,3]dioxol-5-yl)-1-(6,7-dimethoxy-3,4-dihydroisoquinolin-2(1 H)-yl)penta-2,4-dien-1-one)
…got a bit unwieldy.
The upshot is: Pip1 is better, but piperine itself is also good.
Other benefits
Piperine does have other benefits too, but the above is what we were most excited to talk about today. Its other benefits include:
- Neuroprotective effects (against Alzheimer’s, Parkinson’s, and more)
- Blood-sugar balancing / antidiabetic effect
- Good for gut microbiome diversity
- Heart health benefits, including cholesterol-balancing
- Boosts bioavailability of other nutrients/drugs
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Are You A Calorie-Burning Machine?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
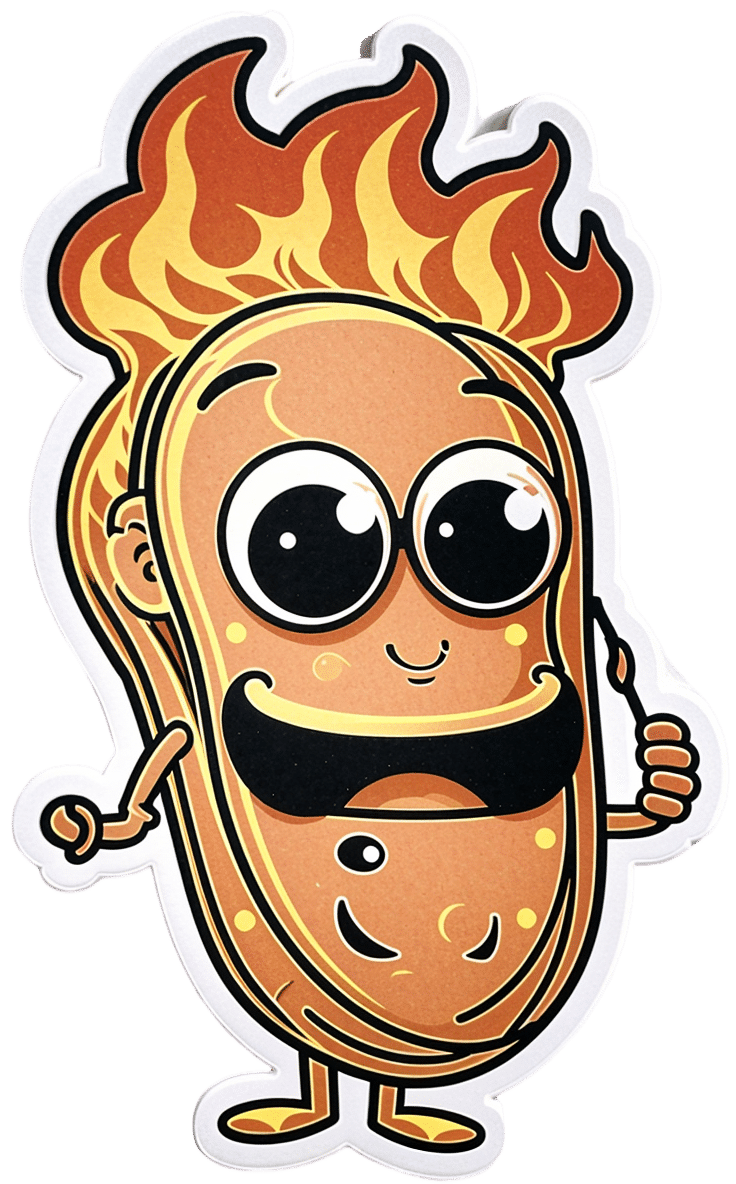
Burn, Calorie, Burn
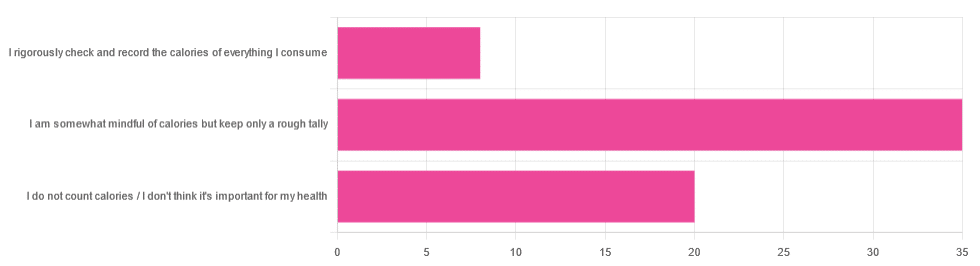
In Tuesday’s newsletter, we asked you whether you count calories, and got the above-depicted, below-described set of answers:
- About 56% said “I am somewhat mindful of calories but keep only a rough tally”
- About 32% said “I do not count calories / I don’t think it’s important for my health”
- About 13% said “I rigorously check and record the calories of everything I consume”
So what does the science say, about the merits of all these positions?
A food’s calorie count is a good measure of how much energy we will, upon consuming the food, have to use or store: True or False?
False, broadly. It can be, at best, a rough guideline. Do you know what a calorie actually is, by the way? Most people don’t.
One thing to know before we get to that: there’s “cal” vs “kcal”. The latter is generally used when it comes to foodstuffs, and it’s what we’ll be meaning whenever we say “calorie” here. 1cal is 1/1000th of a kcal, that’s all.
Now, for what a calorie actually is:
A calorie is the amount of energy needed to raise the temperature of 1 liter of water by 1℃
Question: so, how to we measure how much food is needed to do that?
Answer: by using a bomb calorimeter! Which is the exciting name for the apparatus used to literally burn food and capture the heat produced to indeed raise the temperature of 1 liter of water by 1℃.
If you’re having trouble imagining such equipment, here it is:
Bomb Calorimeter: Definition, Construction, & Operation (with diagram and FAQs)
The unfortunate implication of the above information
A kilogram of sawdust contains about a 1000 kcal, give or take what wood was used and various other conditions.
However, that does not mean you can usefully eat the sawdust. In other words:
Calorie count tells us only how good something is at raising the temperature of water if physically burned.
Now do you see why oils and sugars have such comparably high calorie counts?
And while we may talk about “burning calories” as a metaphor, we do not, in fact, have a little wood stove inside us burning the food we eat.
A calorie is a calorie: True or False?
Definitely False! Building on from the above… We will get very little energy from sawdust; it’s not just that we can’t use it; we can’t store it either; it’ll mostly pass through as fiber.
(however, please do not use sawdust to get your daily dose of fiber either, as it is not safe for human consumption and may give you diseases, depending on what is lurking in it)
But let’s look at oil and sugar, two very high-calorie categories of food, because they’re really easy to physically burn and they give off a good flame.
A bomb calorimeter may treat them quite equally, but to our body, they are metabolically very different indeed.
For a start, most sugars will get absorbed and processed much more quickly than most oils, and that can overwhelm the liver (responsible for glycogen management), and lead to non-alcoholic fatty liver disease, diabetes, and more. Metabolic syndrome in general, and if you keep it up too much and you may find it’s now a lottery between dying of NAFLD, diabetes, or heart disease (it’ll usually be the heart disease that kills).
See also:
- Which Sugars Are Healthier, And Which Are Just The Same?
- 10 Ways To Balance Blood Sugars
- How To Unfatty A Fatty Liver
Meanwhile, we know all about the different kinds of nutritional profiles that oils can have, and some can promote having high energy without putting on fat, while others can strain the heart. Not even “a fat is a fat”, so “a calorie is a calorie” doesn’t get much mileage outside of a bomb calorimeter!
See also:
A calorie-controlled / calorie-restricted diet is an effective weight loss strategy: True or False?
True, usually! Surprise!
- On the one hand: calories are a wildly imprecise way to reckon the value of food, and using them as a guide to health can be dangerously misleading
- On the other hand: the very activity of calorie-counting itself promotes mindful eating, which is very good for the health
There is a strong difference between the mind of somebody who is carefully logging their pre-bedtime piece of chocolate and reflecting on its nutritional value, vs someone who isn’t sure whether this is their second or third glass of wine, nor how much the glass contained.
So if you want to get most of the benefits of a calorie-controlled diet without counting calories, you may try taking a “mindful eating” approach to diet.
However! If you want to do this for weight loss, be aware, that you will have to practice it all the time, not just for one meal here and there.
You can read more on how to do “mindful eating” here:
Dr. Rupy Aujla: The Kitchen Doctor | Mindful Eating & Interoception
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: