Gut Health and Anxiety
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I’d like to read articles on gut health and anxiety❞
We hope you caught yesterday’s edition of 10almonds, which touched on both of those! Other past editions you might like include:
We’ll be sure to include more going forward, too!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Stop Binge-Eating: Flip This Switch!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“The Big Eating Therapist” Sarah Dosanjh has insights from both personal and professional experience:
No “Tough Love” Necessary
Eating certain foods is often socially shamed, and it’s easy to internalize that, and feel guilty. While often guilt is considered a pro-social emotion that helps people to avoid erring in a way that will get us excluded from the tribe (bearing in mind that for most of our evolutionary history, exile would mean near-certain death), it is not good at behavior modification when it comes to addictions or anything similar to addictions.
The reason for this is that if we indulge in a pleasure we feel we “shouldn’t” and expect we’d be shamed for, we then feel bad, and we immediately want something to make us feel better. Guess what that something will be. That’s right: the very same thing we literally just felt ashamed about.
So guilt is not helpful when it comes to (for example) avoiding binge-eating.
Instead, Dosanjh points us to a study whereby dieters ate a donut and drank water, before being given candy for taste testing. The control group proceeded without intervention, while the experimental group had a self-compassion intervention between the donut and the candy. This meant that researchers told the participants not to feel bad about eating the donut, emphasizing self-kindness, mindfulness, and common humanity. The study found that those who received the intervention, ate significantly less candy.
What we can learn from this is: we must be kind to ourselves. Allowing ourselves, consciously and mindfully, “a little treat”, secures its status as being “little”, and “a treat”. Then we smile, thinking “yes, that was a nice little thing to do for myself”, and proceed with our day.
This kind of self-compassion helps avoid the “meta-binge” process, where guilt from one thing leads to immediately reaching for another.
For more on this, plus a link to the study she mentioned, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
Death by Sitting – by Carolyne Thompson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be wondering: is this a lot of words to say “sit down less”?
And the answer is: there’s a lot more in here than that. Of course, yes, “sit down less” is an important take-away, but there’s a lot about the specific problems caused by sitting in chairs, the health risks are that are increased and how, and the early warning signs to watch out for.
After these chapters of woe, most of the book is given over to solutions; about taking standing and walking breaks, tying movement to productivity, why exercise alone is not enough to offset the damage of sitting, relearning ergonomic posture in the context of mitigating the harm, psychological shifts to break the habit of sitting, redefining social norms around sitting and socializing, rewiring one’s body and retraining better movements as well as postures to always immediately move out of if one finds oneself in, and much much more.
The style is light and easy to read, while still including scientific research as appropriate along with practical, actionable advice.
Bottom line: if you’d like to do better for your body than slowly killing it for however many hours a day, then this book has a wealth of advice far beyond the obvious (but important!) “sit less”.
Share This Post
-
Behavioral Activation Against Depression & Anxiety
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Behavioral Activation Against Depression & Anxiety
Psychologists do love making fancy new names for things.
You thought you were merely “eating your breakfast”, but now it’s “Happiness-Oriented Basic Behavioral Intervention Therapy (HOBBIT)” or something.
This one’s quite simple, so we’ll keep it short for today, but it is one more tool for your toolbox:
What is Behavioral Activation?
Behavioral Activation is about improving our mood (something we can’t directly choose) by changing our behavior (something we usually can directly choose).
An oversimplified (and insufficient, as we will explain, but we’ll use this one to get us started) example would be “whistle a happy tune and you will be happy”.
Behavioral Activation is not a silver bullet
Or if it is, then it’s the kind you have to keep shooting, because one shot is not enough. However, this becomes easier than you might think, because Behavioral Activation works by…
Creating a Positive Feedback Loop
A lot of internal problems in depression and anxiety are created by the fact that necessary and otherwise desirable activities are being written off by the brain as:
- Pointless (depression)
- Dangerous (anxiety)
The inaction that results from these aversions creates a negative feedback loop as one’s life gradually declines (as does one’s energy, and interest in life), or as the outside world seems more and more unwelcoming/scary.
Instead, Behavioral Activation plans activities (usually with the help of a therapist, as depressed/anxious people are not the most inclined to plan activities) that will be:
- attainable
- rewarding
The first part is important, because the maximum of what is “attainable” to a depressed/anxious person can often be quite a small thing. So, small goals are ideal at first.
The second part is important, because there needs to be some way of jump-starting a healthier dopamine cycle. It also has to feel rewarding during/after doing it, not next year, so short term plans are ideal at first.
So, what behavior should we do?
That depends on you. Behavioral Activation calls for keeping track of our activities (bullet-journaling is fine, and there are apps* that can help you, too) and corresponding moods.
*This writer uses the pragmatic Daylio for its nice statistical analyses of bullet-journaling data-points, and the very cute Finch for more keyword-oriented insights and suggestions. Whatever works for you, works for you, though! It could even be paper and pen.
Sometimes the very thought of an activity fills us with dread, but the actual execution of it brings us relief. Bullet-journaling can track that sort of thing, and inform decisions about “what we should do” going forwards.
Want a ready-made brainstorm to jump-start your creativity?
Here’s list of activities suggested by TherapistAid (a resource hub for therapists)
Want to know more?
You might like:
- How To Use Behavioral Activation (guide for end users)
- Treatment Guide: Behavioral Activation (guide for clinicians)
Take care!
Share This Post
Related Posts
-
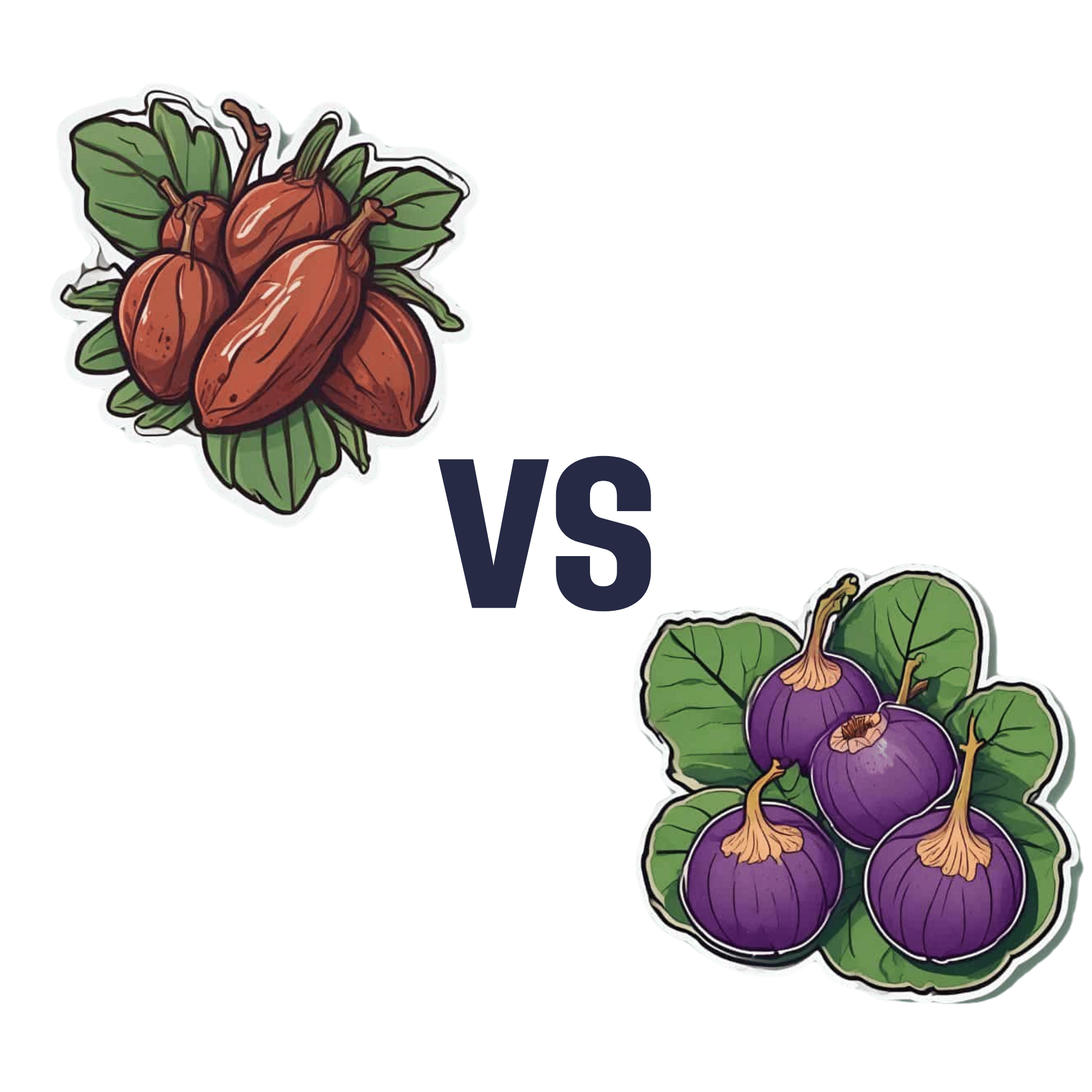
Dates vs Figs – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dates to figs, we picked the dates.
Why?
Dates are higher in sugar, but also have a lower glycemic index than figs, which makes the sugar content much healthier. On the flipside, figs do have around 3x more fiber.
So far, so balanced.
When it comes to micronutrients though, dates take the prize much more clearly.
Dates have slightly more of most vitamins, and a lot more of most minerals.
In particular, dates are several times higher in copper, iron, magnesium, manganese, phosphorus, selenium, and zinc.
As for other phytochemical benefits going on:
- both are good against diabetes for reasons beyond the macros
- both have anti-inflammatory properties
- dates have anticancer properties
- dates have kidney-protecting properties
So in this last case, another win for dates.
Both are still great though, so do enjoy both!
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Creatine: Very Different For Young & Old People
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the Deal with Creatine?
Creatine is best-known for its use as a sports supplement. It has a few other uses too, usually in the case of helping to treat (or recover from) specific medical conditions.
What actually is it?
Creatine is an organic compound formed from amino acids (mostly l-arginine and lysine, can be l-methionine, but that’s not too important for our purposes here).
We can take it as a supplement, we can get it in our diet (unless we’re vegan, because plants don’t make it; vertebrates do), and we can synthesize it in our own bodies.
What does it do?
While creatine supplements mostly take the form of creatine monohydrate, in the body it’s mostly stored in our muscle tissue as phosphocreatine, and it helps cells produce adenosine triphosphate, (ATP).
ATP is how energy is kept ready to use by cells, and is cells’ immediate go-to when they need to do something. For this reason, it’s highly instrumental in cell repair and rebuilding—which is why it’s used so much by athletes, especially bodybuilders or other athletes that have a vested interest in gaining muscle mass and enjoying faster recovery times.
See: Creatine use among young athletes
However! For reasons as yet not fully known, it doesn’t seem to have the same beneficial effect after a certain age:
What about the uses outside of sport?
Almost all studies outside of athletic performance have been on animals, despite it being suggested as potentially helpful for many things, including:
- Alzheimer’s disease
- Parkinson’s disease
- Huntington’s disease
- ischemic stroke
- epilepsy
- brain or spinal cord injuries
- motor neuron disease
- memory and brain function in older adults
However, research that’s been done on humans has been scant, if promising:
- A review of creatine supplementation in age-related diseases: more than a supplement for athletes
- Creatine supplementation and cognitive performance in elderly individuals
In short: creatine may reduce symptoms and slow the progression of some neurological diseases, although more research in humans is needed, and words such as “promising”, “potential”, etc are doing a lot of the heavy lifting in those papers we just cited.
Is it safe?
It seems so: Creatine supplementation and health variables: a retrospective study
Nor does it appear to create the sometimes-rumored kidney problems, cramps, or dehydration:
Where can I get it?
You can get it from pretty much any sports nutrition outlet, or you can order online. For example:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healthy Butternut Macaroni Cheese
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A comfort food classic, healthy and plant-based, without skimping on the comfort.
You will need
- ½ butternut squash, peeled and cut into small pieces (if buying ready-chopped, this should be about 1 lb)
- 1 onion, chopped
- ¼ bulb garlic
- 2 tbsp extra virgin olive oil
- 12 oz (or thereabouts) wholegrain macaroni, or similar pasta shape (even penne works fine—which is good, as it’s often easier to buy wholegrain penne than wholegrain macaroni) (substitute with a gluten-free pasta such as buckwheat pasta, if avoiding gluten)
- 6 oz (or thereabouts) cashews, soaked in hot water for at least 15 minutes (but longer is better)
- ½ cup milk (your preference what kind; we recommend hazelnut for its mellow nutty flavor)
- 3 tbsp nutritional yeast
- Juice of ½ lemon
- 2 tsp black pepper, coarse ground
- ½ tsp MSG, or 1 tsp low-sodium salt
- Optional: smoked paprika, to serve
Note: if you are allergic to nuts, please accept our apologies that there’s no substitution available in this one. Simply put, removing the cashews would mean changing most of the rest of the recipe to compensate, so there’s no easy “or substitute with…” that we can mention. We’ll have to find/develop a good healthy plant-based no-nuts recipe for you at a later date.
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉ / 200℃.
2) Combine the butternut squash, onion, and garlic with the olive oil, in a large roasting tin, tossing thoroughly to ensure an even coat of oil. Roast them for about 25 minutes until soft.
3) Cook the macaroni while you wait (this should take about 10 minutes or so in salted water), drain, and rinse thoroughly in cold water, before setting aside. This cooling increases the pasta’s resistant starch content (that’s good, for your gut and for your blood sugars, and thus also for your heart and brain), and it will maintain this benefit even when we reheat it later.
4) Drain the cashews, and tip them into a high-speed blender with the milk, and process until smooth. Add the roasted vegetables and the remaining ingredients apart from the pasta, and continue to process until again smooth. You can add a little more milk if you need to, but go easy with it.
5) Heat the sauce (that you just made in the food processor) gently in a saucepan, and refresh the pasta by pouring a kettle of boiling water through it in a colander.
6) Optional: combine the pasta and sauce in an ovenproof dish or cast iron pan, and give it a few minutes under the hottest grill (or browning iron, if you have such) your oven can muster. Alternatively, use a culinary blowtorch, if you have one.
7) Serve; and if you didn’t do the optional step above, this means combining the pasta and sauce. You can also dust the top with some extra seasonings if you like. Smoked paprika works well for this.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Butternut Squash vs Pumpkin – Which is Healthier?
- Cashew Nuts vs Coconut – Which is Healthier?
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Sea Salt vs MSG – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: