Grapefruit vs Lemon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing grapefruit to lemon, we picked the lemon.
Why?
Grapefruit has its merits, but in the battle of the citrus fruits, lemons come out on top nutritionally:
In terms of macros, grapefruit has more carbs while lemons have more fiber. So, while both have a low glycemic index, lemon is still the winner by the numbers.
Looking at the vitamins, here we say grapefruit’s strengths: grapefruit has more of vitamins A, B2, B3, and choline, while lemon has more of vitamins B6 and C. So, a 4:2 win for grapefruit here.
In the category of minerals, lemons retake the lead: grapefruit has more zinc, while lemon has more calcium, copper, iron, manganese, and selenium.
One final consideration that’s not shown in the nutritional values, is that grapefruit contains high levels of furanocoumarin, which can inhibit cytochrome P-450 3A4 isoenzyme and P-glycoptrotein transporters in the intestine and liver—slowing down their drug metabolism capabilities, thus effectively increasing the bioavailability of many drugs manifold.
This may sound superficially like a good thing (improving bioavailability of things we want), but in practice it means that in the case of many drugs, if you take them with (or near in time to) grapefruit or grapefruit juice, then congratulations, you just took an overdose. This happens with a lot of meds for blood pressure, cholesterol (including statins), calcium channel-blockers, anti-depressants, benzo-family drugs, beta-blockers, and more. Oh, and Viagra, too. Which latter might sound funny, but remember, Viagra’s mechanism of action is blood pressure modulation, and that is not something you want to mess around with unduly. So, do check with your pharmacist to know if you’re on any meds that would be affected by grapefruit or grapefruit juice!
PS: the same substance is quite available in pummelos and sour oranges (but not meaningfully in sweet oranges); you can see a chart here showing the relative furanocoumarin contents of many citrus fruits, or lack thereof as the case may be, as it is for lemons and most limes)
Adding up the sections gives us a clear win for lemons, but by all means enjoy either or both; just watch out for that furanocoumarin content of grapefruit if you’re on any meds affected by such (again, do check with your pharmacist, as our list was far from exhaustive—and yes, this question is one that a pharmacist will answer more easily and accurately than a doctor will).
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← citrus fruits in general make the list; they inhibit tumor growth and kill cancer cells; regular consumption is also associated with a lower cancer risk 🙂
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
10 Ways To Naturally Boost Dopamine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dopamine is the “reward” hormone, and is responsible for motivation, as well as various oft-forgotten functions (such as spatial skills, motor functions, task processing, planning, and language). Sometimes, our relationship with dopamine isn’t what it could be, so here’s how to fix that:
Let’s get hormone-hacking…
Here are the 10 ways:
- The seesaw effect: reduce overstimulation by taking tolerance breaks from high-dopamine activities that aren’t particularly useful (like social media or phone games), allowing for natural enjoyment of daily activities that you’d normally find enjoyable. Think: if you died and negotiated to be sent back to life on the condition you’d appreciate it properly this time, what things would you then spend your time doing? It’s probably not Kingdom Crush Saga Farm 2, is it?
- Conscious state meditation: practise conscious state meditation, focusing inward to reduce anxiety and release dopamine. Even a few minutes a day can significantly enhance dopamine levels.
- Hack your REM cycles: optimize sleep, especially REM cycles, which produce the most dopamine. Aim to wake up after your final REM cycle to feel energized and happy.
- The runner’s high: engage in regular exercise, which boosts dopamine through physical exertion and can lead to feelings of relaxation and euphoria, often known as the “runner’s high.”
- Mood-enhancing music: listen to music that makes you feel good. Favorite songs can stimulate dopamine production, improving your mood and well-being.
- Bright light therapy: spend time in natural sunlight to stimulate dopamine production and elevate your mood, countering the negative effects of extended indoor time. If natural sunlight is not very available where you are (e.g. this writer who lives next to an ancient bog surrounded by fog and the days are getting short, at time of writing), then artificial daylight lamps are respectable supplement—but just that, a supplement, not a replacement. Despite how it looks/feels, natural sunlight (especially in the morning, to cue the circadian rhythm to do its thing) is beneficial even through cloud cover.
- Relieve stress for good: actively reduce stress, as it inhibits dopamine. Simplify daily routines and eliminate stressors to naturally boost dopamine and feel more relaxed. Of course, you cannot remove all stress from your life, so get good at managing the stress created by the stressors that do remain.
- Tap into your flow state: enter a “flow state” by focusing deeply on an engaging task, which can elevate dopamine levels and boost motivation and happiness.
- The hormesis effect: embrace mild physical challenges, like cold showers. The temporary discomfort will paradoxically increase dopamine (it’s the body’s way of saying “congratulations, you survived the hard thing, here’s a little treat, so that you’ll be motivated to survive the next hard thing, too”)
- Activate your inner artist: engage in creative activities that you find fun. The process of creating boosts dopamine and provides motivation, enhancing mood and enjoyment in life.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Rebalancing Dopamine (Without “Dopamine Fasting”)
Take care!
Share This Post
-
Blue Light At Night? Save More Than Just Your Sleep!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Beating The Insomnia Blues
You previously asked us about recipes for insomnia (or rather, recipes/foods to help with easing insomnia). We delivered!
But we also semi-promised we’d cover a bit more of the general management of insomnia, because while diet’s important, it’s not everything.
Sleep Hygiene
Alright, you probably know this first bit, but we’d be remiss if we didn’t cover it before moving on:
- No caffeine or alcohol before bed
- Ideally: none earlier either, but if you enjoy one or the other or both, we realize an article about sleep hygiene isn’t going to be what changes your mind
- Fresh bedding
- At the very least, fresh pillowcase(s). While washing and drying an entire bedding set constantly may be arduous and wasteful of resources, it never hurts to throw your latest pillowcase(s) in with each load of laundry you happen to do.
- Warm bed, cool room = maximum coziness
- Dark room. Speaking of which…
About That Darkness…
When we say the room should be dark, we really mean it:
- Not dark like “evening mood lighting”, but actually dark.
- Not dark like “in the pale moonlight”, but actually dark.
- Not dark like “apart from the light peeking under the doorway”, but actually dark.
- Not dark like “apart from a few LEDs on electronic devices that are on standby or are charging”, but actually dark.
There are many studies about the impact of blue light on sleep, but here’s one as an example.
If blue light with wavelength between 415 nm and 455 nm (in the visible spectrum) hits the retina, melatonin (the sleep hormone) will be suppressed.
The extent of the suppression is proportional to the amount of blue light. This means that there is a difference between starting at an “artificial daylight” lamp, and having the blue LED of your phone charger showing… but the effect is cumulative.
And it gets worse:
❝This high energy blue light passes through the cornea and lens to the retina causing diseases such as dry eye, cataract, age-related macular degeneration, even stimulating the brain, inhibiting melatonin secretion, and enhancing adrenocortical hormone production, which will destroy the hormonal balance and directly affect sleep quality.❞
Read it in full: Research progress about the effect and prevention of blue light on eyes
See also: Age-related maculopathy and the impact of blue light hazard
So, what this means, if we value our health, is:
- Switch off, or if that’s impractical, cover the lights of electronic devices. This might be as simple as placing your phone face-down rather than face-up, for instance.
- Invest in blackout blinds/curtains (per your preference). Serious ones, like these ← see how they don’t have to be black to be blackout! You don’t have to sacrifice style for function
- If you can’t reasonably do the above, consider a sleep mask. Again, a good one. Not the kind you were given on a flight, or got free with some fluffy handcuffs. We mean a full-blackout sleep mask that’s designed to be comfortable enough to sleep in, like this one.
- If you need to get up to pee or whatever, do like a pirate and keep one eye covered/closed. That way, it’ll remain unaffected by the light. Pirates did it to retain their night vision when switching between being on-deck or below, but you can do it to halve the loss of melatonin.
Lights-Out For Your Brain Too
You can have all the darkness in the world and still not sleep if your mind is racing thinking about:
- your recent day
- your next day
- that conversation you wish had gone differently
- what you really should have done when you were 18
- how you would go about fixing your country’s socio-political and economic woes if you were in charge
- Etc.
We wrote about how to hit pause on all that, in a previous edition of 10almonds.
Check it out: The Off-Button For Your Brain—How to “just say no” to your racing mind (this trick really works)
Sweet dreams!
Share This Post
- No caffeine or alcohol before bed
-
Undoing The Damage Of Life’s Hard Knocks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sometimes, What Doesn’t Kill Us Makes Us Insecure
We’ve written before about Complex PTSD, which is much more common than the more popularly understood kind:
Given that C-PTSD affects so many people (around 1 in 5, but really, do read the article above! It explains it better than we have room to repeat today), it seems like a good idea to share tips for managing it.
(Last time, we took all the space for explaining it, so we just linked to some external resources at the end)
What happened to you?
PTSD has (as a necessity, as part of its diagnostic criteria) a clear event that caused it, which makes the above question easy to answer.
C-PTSD often takes more examination to figure out what tapestry of circumstances (and likely but not necessarily: treatment by other people) caused it.
Often it will feel like “but it can’t be that; that’s not that bad”, or “everyone has things like that” (in which case, you’re probably one of the one in five).
The deeper questions
Start by asking yourself: what are you most afraid of, and why? What are you most ashamed of? What do you fear that other people might say about you?
Often there is a core pattern of insecurity that can be summed up in a simple, harmful, I-message, e.g:
- I am a bad person
- I am unloveable
- I am a fake
- I am easy to hurt
- I cannot keep my loved ones safe
…and so forth.
For a bigger list of common insecurities to see what resonates, check out:
Basic Fears/Insecurities, And Their Corresponding Needs/Desires
Find where they came from
You probably learned bad beliefs, and consequently bad coping strategies, because of bad circumstances, and/or bad advice.
- When a parent exclaimed in anger about how stupid you are
- When a partner exclaimed in frustration that always mess everything up
- When an employer told you you weren’t good enough
…or maybe they told you one thing, and showed you the opposite. Or maybe it was entirely non-verbal circumstances:
- When you gambled on a good idea and lost everything
- When you tried so hard at some important endeavour and failed
- When you thought someone could be trusted, and learned the hard way that you were wrong
These are “life’s difficult bits”, but when we’ve lived through a whole stack of them, it’s less like a single shattering hammer-blow of PTSD, and more like the consistent non-stop tap tap tap that ends up doing just as much damage in the long run.
Resolve them
That may sound a bit like a “and quickly create world peace” level of task, but we have tools:
Ask yourself: what if…
…it had been different? Take some time and indulge in a full-blown fantasy of a life that was better. Explore it. How would those different life lessons, different messages, have impacted who you are, your personality, your behaviour?
This is useful, because the brain is famously bad at telling real memories from false ones. Consciously, you’ll know that one was an exploratory fantasy, but to your brain, it’s still doing the appropriate rewiring. So, little by little, neuroplasticity will do its thing.
Tell yourself a better lie
We borrowed this one from the title of a very good book which we’ve reviewed previously.
This idea is not about self-delusion, but rather that we already express our own experiences as a sort of narrative, and that narrative tends to contain value judgements that are often not useful, e.g. “I am stupid”, “I am useless”, and all the other insecurities we mentioned earlier. Some simple examples might be:
- “I had a terrible childhood” → “I have come so far”
- “I should have known better” → “I am wiser now”
- “I have lost so much” → “I have experienced so much”
So, replacing that self-talk can go a long way to re-writing how secure we feel, and therefore how much trauma-response (ideally: none!) we have to stimuli that are not really as threatening as we sometimes feel they are (a hallmark of PTSD in general).
Here’s a guide to more ways:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
Take care!
Share This Post
Related Posts
-
Could Just Two Hours Sleep Per Day Be Enough?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Polyphasic Sleep… Super-Schedule Or An Idea Best Put To Rest?
What is it?
Let’s start by defining some terms:
- Monophasic sleep—sleeping in one “chunk” per day. For example, a good night’s “normal” sleep.
- Biphasic sleep—sleeping in two “chunks” per day. Typically, a shorter night’s sleep, with a nap usually around the middle of the day / early afternoon.
- Polyphasic sleep—sleeping in two or more “chunks per day”. Some people do this in order to have more hours awake per day, to do things. The idea is that sleeping this way is more efficient, and one can get enough rest in less time. The most popular schedules used are:
- The Überman schedule—six evenly-spaced 20-minute naps, one every four hours, throughout the 24-hour day. The name is a semi-anglicized version of the German word Übermensch, “Superman”.
- The Everyman schedule—a less extreme schedule, that has a three-hours “long sleep” during the night, and three evenly-spaced 20-minute naps during the day, for a total of 4 hours sleep.
There are other schedules, but we’ll focus on the most popular ones here.
Want to learn about the others? Visit: Polyphasic.Net (a website by and for polyphasic sleep enthusiasts)
Some people have pointed to evidence that suggests humans are naturally polyphasic sleepers, and that it is only modern lifestyles that have forced us to be (mostly) monophasic.
There is at least some evidence to suggest that when environmental light/dark conditions are changed (because of extreme seasonal variation at the poles, or, as in this case, because of artificial changes as part of a sleep science experiment), we adjust our sleeping patterns accordingly.
The counterpoint, of course, is that perhaps when at the mercy of long days/nights at the poles, or no air-conditioning to deal with the heat of the day in the tropics, that perhaps we were forced to be polyphasic, and now, with modern technology and greater control, we are free to be monophasic.
Either way, there are plenty of people who take up the practice of polyphasic sleep.
Ok, But… Why?
The main motivation for trying polyphasic sleep is simply to have more hours in the day! It’s exciting, the prospect of having 22 hours per day to be so productive and still have time over for leisure.
A secondary motivation for trying polyphasic sleep is that when the brain is sleep-deprived, it will prioritize REM sleep. Here’s where the Überman schedule becomes perhaps most interesting:
The six evenly-spaced naps of the Überman schedule are each 20 minutes long. This corresponds to the approximate length of a normal REM cycle.
Consequently, when your head hits the pillow, you’ll immediately begin dreaming, and at the end of your dream, the alarm will go off.
Waking up at the end of a dream, when one hasn’t yet entered a non-REM phase of sleep, will make you more likely to remember it. Similarly, going straight into REM sleep will make you more likely to be aware of it, thus, lucid dreaming.
Read: Sleep fragmentation and lucid dreaming (actually a very interesting and informative lucid dreaming study even if you don’t want to take up polyphasic sleep)
Six 20-minute lucid-dreaming sessions per day?! While awake for the other 22 hours?! That’s… 24 hours per day of wakefulness to use as you please! What sorcery is this?
Hence, it has quite an understandable appeal.
Next Question: Does it work?
Can we get by without the other (non-REM) kinds of sleep?
According to Überman cycle enthusiasts: Yes! The body and brain will adapt.
According to sleep scientists: No! The non-REM slow-wave phases of sleep are essential
Read: Adverse impact of polyphasic sleep patterns in humans—Report of the National Sleep Foundation sleep timing and variability consensus panel
(if you want to know just how bad it is… the top-listed “similar article” is entitled “Suicidal Ideation”)
But what about, for example, the Everman schedule? Three hours at night is enough for some non-REM sleep, right?
It is, and so it’s not as quickly deleterious to the health as the Überman schedule. But, unless you are blessed with rare genes that allow you to operate comfortably on 4 hours per day (you’ll know already if that describes you, without having to run any experiment), it’s still bad.
Adults typically need 7–9 hours of sleep per night, and if you don’t get it, you’ll accumulate a sleep debt. And, importantly:
When you accumulate sleep debt, you are borrowing time at a very high rate of interest!
And, at risk of laboring the metaphor, but this is important too:
Not only will you have to pay it back soon (with interest), you will be hounded by the debt collection agents—decreased cognitive ability and decreased physical ability—until you pay up.
In summary:
- Polyphasic sleep is really very tempting
- It will give you more hours per day (for a while)
- It will give the promised lucid dreaming benefits (which is great until you start micronapping between naps, this is effectively a mini psychotic break from reality lasting split seconds each—can be deadly if behind the wheel of a car, for instance!)
- It is unequivocally bad for the health and we do not recommend it
Bottom line:
Some of the claimed benefits are real, but are incredibly short-term, unsustainable, and come at a cost that’s far too high. We get why it’s tempting, but ultimately, it’s self-sabotage.
(Sadly! We really wanted it to work, too…)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A short history of sunscreen, from basting like a chook to preventing skin cancer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australians have used commercial creams, lotions or gels to manage our skin’s sun exposure for nearly a century.
But why we do it, the preparations themselves, and whether they work, has changed over time.
In this short history of sunscreen in Australia, we look at how we’ve slathered, slopped and spritzed our skin for sometimes surprising reasons.
At first, suncreams helped you ‘tan with ease’
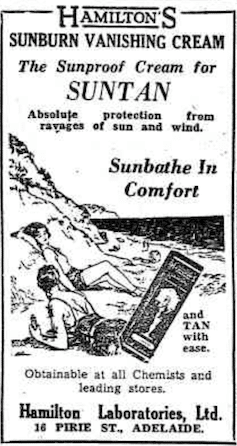
This early sunscreen claimed you could ‘tan with ease’.
Trove/NLASunscreens have been available in Australia since the 30s. Chemist Milton Blake made one of the first.
He used a kerosene heater to cook batches of “sunburn vanishing cream”, scented with French perfume.
His backyard business became H.A. Milton (Hamilton) Laboratories, which still makes sunscreens today.
Hamilton’s first cream claimed you could “
Sunbathe in Comfort and TAN with ease”. According to modern standards, it would have had an SPF (or sun protection factor) of 2.The mirage of ‘safe tanning’
A tan was considered a “modern complexion” and for most of the 20th century, you might put something on your skin to help gain one. That’s when “safe tanning” (without burning) was thought possible.
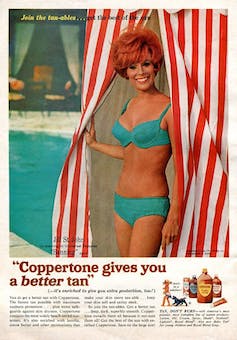
This 1967 Coppertone advertisement urged you to ‘tan, not burn’.
SenseiAlan/Flickr, CC BY-SASunburn was known to be caused by the UVB component of ultraviolet (UV) light. UVA, however, was thought not to be involved in burning; it was just thought to darken the skin pigment melanin. So, medical authorities advised that by using a sunscreen that filtered out UVB, you could “safely tan” without burning.
But that was wrong.
From the 70s, medical research suggested UVA penetrated damagingly deep into the skin, causing ageing effects such as sunspots and wrinkles. And both UVA and UVB could cause skin cancer.
Sunscreens from the 80s sought to be “broad spectrum” – they filtered both UVB and UVA.
Researchers consequently recommended sunscreens for all skin tones, including for preventing sun damage in people with dark skin.
Delaying burning … or encouraging it?
Up to the 80s, sun preparations ranged from something that claimed to delay burning, to preparations that actively encouraged it to get that desirable tan – think, baby oil or coconut oil. Sun-worshippers even raided the kitchen cabinet, slicking olive oil on their skin.
One manufacturer’s “sun lotion” might effectively filter UVB; another’s merely basted you like a roast chicken.
Since labelling laws before the 80s didn’t require manufacturers to list the ingredients, it was often hard for consumers to tell which was which.
At last, SPF arrives to guide consumers
In the 70s, two Queensland researchers, Gordon Groves and Don Robertson, developed tests for sunscreens – sometimes experimenting on students or colleagues. They printed their ranking in the newspaper, which the public could use to choose a product.
An Australian sunscreen manufacturer then asked the federal health department to regulate the industry. The company wanted standard definitions to market their products, backed up by consistent lab testing methods.
In 1986, after years of consultation with manufacturers, researchers and consumers, Australian Standard AS2604 gave a specified a testing method, based on the Queensland researchers’ work. We also had a way of expressing how well sunscreens worked – the sun protection factor or SPF.
This is the ratio of how long it takes a fair-skinned person to burn using the product compared with how long it takes to burn without it. So a cream that protects the skin sufficiently so it takes 40 minutes to burn instead of 20 minutes has an SPF of 2.
Manufacturers liked SPF because businesses that invested in clever chemistry could distinguish themselves in marketing. Consumers liked SPF because it was easy to understand – the higher the number, the better the protection.
Australians, encouraged from 1981 by the Slip! Slop! Slap! nationwide skin cancer campaign, could now “slop” on a sunscreen knowing the degree of protection it offered.
How about skin cancer?
It wasn’t until 1999 that research proved that using sunscreen prevents skin cancer. Again, we have Queensland to thank, specifically the residents of Nambour. They took part in a trial for nearly five years, carried out by a research team led by Adele Green of the Queensland Institute of Medical Research. Using sunscreen daily over that time reduced rates of squamous cell carcinoma (a common form of skin cancer) by about 60%.
Follow-up studies in 2011 and 2013 showed regular sunscreen use almost halved the rate of melanoma and slowed skin ageing. But there was no impact on rates of basal cell carcinoma, another common skin cancer.
By then, researchers had shown sunscreen stopped sunburn, and stopping sunburn would prevent at least some types of skin cancer.
What’s in sunscreen today?
An effective sunscreen uses one or more active ingredients in a cream, lotion or gel. The active ingredient either works:
-
“chemically” by absorbing UV and converting it to heat. Examples include PABA (para-aminobenzoic acid) and benzyl salicylate, or
-
“physically” by blocking the UV, such as zinc oxide or titanium dioxide.
Physical blockers at first had limited cosmetic appeal because they were opaque pastes. (Think cricketers with zinc smeared on their noses.)
With microfine particle technology from the 90s, sunscreen manufacturers could then use a combination of chemical absorbers and physical blockers to achieve high degrees of sun protection in a cosmetically acceptable formulation.
Where now?
Australians have embraced sunscreen, but they still don’t apply enough or reapply often enough.
Although some people are concerned sunscreen will block the skin’s ability to make vitamin D this is unlikely. That’s because even SPF50 sunscreen doesn’t filter out all UVB.
There’s also concern about the active ingredients in sunscreen getting into the environment and whether their absorption by our bodies is a problem.
Sunscreens have evolved from something that at best offered mild protection to effective, easy-to-use products that stave off the harmful effects of UV. They’ve evolved from something only people with fair skin used to a product for anyone.
Remember, slopping on sunscreen is just one part of sun protection. Don’t forget to also slip (protective clothing), slap (hat), seek (shade) and slide (sunglasses).
Laura Dawes, Research Fellow in Medico-Legal History, Australian National University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
-
Palliative care as a true art form
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How do you ease the pain from an ailment amidst lost words? How can you serve the afflicted when lines start to blur? When the foundation of communication begins to crumble, what will be the pillar health-care professionals can lean on to support patients afflicted with dementia during their final days?
The practice of medicine is both highly analytical and evidence based in nature. However, it is considered a “practice” because at the highest level, it resembles a musician navigating an instrument. It resembles art. Between lab values, imaging techniques and treatment options, the nuances for individualized patient care so often become threatened.
Dementia, a non-malignant terminal illness, involves the progressive cognitive and social decline in those afflicted. Though there is no cure, dementia is commonly met in the setting of end-of-life care. During this final stage of life, the importance of comfort via symptomatic management and communication usually is a priority in patient care. But what about the care of a patient suffering from dementia? While communication serves as the vehicle to deliver care at a high level, medical professionals are suddenly met with a roadblock. And there … behind the pieces of shattered communication and a dampened map of ethical guidelines, health-care providers are at a standstill.
It’s 4:37 a.m. You receive a text message from the overnight nurse at a care facility regarding a current seizure. After lorazepam is ordered and administered, Mr. H, a quick-witted 76-year-old, stabilizes. Phenobarbital 15mg SC qhs was also added to prevent future similar events. You exhale a sigh of relief.
Mr. H. has been admitted to the floor 36 hours earlier after having a seizure while playing poker with colleagues. Since he became your patient, he’s shared many stories from professional and family life with you, along with as many jokes as he could fit in between. However, over the course of the next seven days, Mr. H. would develop aspiration pneumonia, progressing to ventilator dependency and, ultimately, multi-organ failure with rapid cognitive decline.
What strategies and tools would you use to maximize the well-being of your patient during his decline? How would you bridge the gap of understanding between the patient’s family and health-care team to provide the standard of care that all patients are owed?
To give Mr. H. the type of care he would have wanted, upon his hospital admission, he should have been questioned about his understanding of illness along with the goals of care of the medical team. The patient should have been informed that it is imperative to adhere to the medical regimen implemented by his team along with the risks of not doing so. In the event disease-related complications arose, advanced directives should have been documented to avoid any unnecessary measures.
It is important to note, that with each change in status of the patient’s health status, the goal of treatment must be reassessed. The patient or surrogate decision-maker’s understanding of these goals is paramount in maintaining the patient’s autonomy. It is often said that effective communication is the bedrock of a healthy relationship. This is true regardless of type of relationship.
This is why I and Megan Vierhout wrote Integrated End of Life Care in Dementia: A Comprehensive Guide, a book targeted at providing a much-needed road map to navigate the many challenges involved in end-of-life care for individuals with dementia. Ultimately, our aim is to provide a compass for both health-care professionals and the families of those affected by the progressive effects of dementia. We provide practical advice on optimizing communication with individuals with dementia while taking their cognitive limitations, preferences and needs into account.
I invite you to explore the unpredictable terrain of end-of-life care for patients with dementia. Together, we can pave a smoother, sturdier path toward the practice of medicine as a true art form.
This article is republished from healthydebate under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: