Why Going Gluten-Free Could Be A Bad Idea
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is A Gluten-Free Diet Right For You?
This is Rachel Begun, MS, RD. She’s a nutritionist who, since her own diagnosis with Celiac disease, has shifted her career into a position of educating the public (and correcting misconceptions) about gluten sensitivity, wheat allergy, and Celiac disease. In short, the whole “gluten-free” field.
First, a quick recap
We’ve written on this topic ourselves before; here’s what we had to say:
On “Everyone should go gluten-free”
Some people who have gone gluten-free are very evangelical about the lifestyle change, and will advise everyone that it will make them lose weight, have clearer skin, more energy, and sing well, too. Ok, maybe not the last one, but you get the idea—a dietary change gets seen as a cure-all.
And for some people, it can indeed make a huge difference!
Begun urges us to have a dose of level-headedness in our approach, though.
Specifically, she advises:
- Don’t ignore symptoms, and/but…
- Don’t self-diagnose
- Don’t just quit gluten
One problem with self-diagnosis is that we can easily be wrong:
But why is that a problem? Surely there’s not a health risk in skipping the gluten just to be on the safe side? As it turns out, there actually is:
If we self-diagnose incorrectly, Begun points out, we can miss the actual cause of the symptoms, and by cheerfully proclaiming “I’m allergic to gluten” or such, a case of endometriosis, or Hashimoto’s, or something else entirely, might go undiagnosed and thus untreated.
“Oh, I feel terrible today, there must have been some cross-contamination in my food” when in fact, it’s an undiagnosed lupus flare-up, that kind of thing.
Similarly, just quitting gluten “to be on the safe side” can mask a different problem, if wheat consumption (for example) contributed to, but did not cause, some ailment.
In other words: it could reduce your undesired symptoms, but in so doing, leave a more serious problem unknown.
Instead…
If you suspect you might have a gluten sensitivity, a wheat allergy, or even Celiac disease, get yourself tested, and take professional advice on proceeding from there.
How? Your physician should be able to order the tests for you.
You can also check out resources available here:
Celiac Disease Foundation | How do I get tested?
Or for at-home gluten intolerance tests, here are some options weighed against each other:
MNT | 5 gluten intolerance tests and considerations
Want to learn more?
Begun has a blog:
Rachel Begun | More than just recipes
(it is, in fact, just recipes—but they are very simple ones!)
You also might enjoy this interview, in which she talks about gluten sensitivity, celiac disease, and bio-individuality:
Want to watch it, but not right now? Bookmark it for later
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
7 Days Of Celery Juice: What’s The Verdict?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Laura “Try” tries many popular trends, and reports on the benefits (or problems, or both). In this case, it’s 7 days of celery juice… Not as a fast, though, i.e. she doesn’t just have celery juice for 7 days, but rather, it’s how she kicks off each morning, with half a liter (16oz) on an empty stomach.
What she found
First, she bought a masticating juicer and organic celery. So, those are expenses to consider, especially the one-off expense of the juicer, and the ongoing expense of organic celery—estimated $90/month).
In terms of taste, she was surprised it wasn’t as bitter as expected, but from the second day onwards, she did use the juicer’s filter to remove the frothy sludge, and she also switched to juicing only the stalks, not the leaves—which are more bitter.
10almonds note: the leaves are more bitter because that’s where the polyphenols are more densely concentrated. The leaves are better for you than the stalks. Enjoy the leaves. Really: if you chop them finely you can use them as herbs in your cooking, and if you’re making a salad, just chop them into that too.
The reason she picked the quantity of half a liter is because this is what she found recommended to coat the stomach lining—on the promise of increased stomach acid production, reduced bacteria overgrowth, as well as antiviral, antifungal, and anti-inflammatory properties. As she’s just one woman without a personal lab, she couldn’t test and thus verify any of these though—but she did still have benefits to report:
She did experience clearer skin, more energy, and better sleep after a few days.
Ultimately, she decided to continue to do it just at the weekends, due to its positive effects, despite the cost and time consumption.
For more personal insights, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Enjoy Bitter Foods For Your Heart & Brain
Take care!
Share This Post
-
This Chair Rocks: A Manifesto Against Ageism – by Ashton Applewhite
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to think of ageism as being 80% “nobody will hire me because I am three years away from standard retirement age”, but it’s a lot more pervasive than that. And some of it, perhaps the most insidious, is the ageism that we can sometimes internalize without thinking it through.
10almonds readers love to avoid/reverse aging (and this reviewer is no different!), but it’s good once in a while to consider our priorities and motivations, for example:
- There is merit in being able to live without disability or discomfort
- There is harm in feeling a need to pass for younger than we are
And yet, even things such as disabilities are, Applewhite fairly argues, not to be feared. Absolutely avoided if reasonably possible of course, yes, but if they happen they happen and it’s good that we be able to make our peace with that, because most people have at least some kind of disability before the end, and can still strive to make the most of the precious gift that is life. The goal can and should be to play the hand we’re dealt and to live as well as we can—whatever that latter means for us personally.
Many people’s life satisfaction goes up in later years, and Applewhite hypothesizes that while some of that can be put down to circumstances (often no longer overwhelmed with work etc, often more financially stable), a lot is a matter of having come to terms with “losing” youth and no longer having that fear. Thus, a new, freer age of life begins.
The book does cover many other areas too, more than we can list here (but for example: ranging from pro/con brain differences to sex and intimacy), and the idea that long life is a team sport, and that we should not fall into the all-American trap of putting independence on a pedestal. Reports of how aging works with close-knit communities in the supercentenarian Blue Zones can be considered to quash this quite nicely, for instance.
The style is casual and entertaining, and yet peppered with scholarly citations, which stack up to 30 pages of references at the back.
Bottom line: getting older is a privilege that not everyone gets to have, so who are we to squander it? This book shares a vital sense of perspective, and is a call-to-arms for us all to do better, together.
Click here to check out This Chair Rocks, and indeed rock it!
Share This Post
-
The Five Pillars Of Longevity
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Five Pillars Of Longevity
This is Dr. Mark Hyman. He’s a medical doctor, and he’s the board president of clinical affairs of the Institute for Functional Medicine. He’s also the founder and medical director of the UltraWellness Center!
What he’d like you to know about is what he calls the “Five Pillars of Longevity”.
Now, here at 10almonds, we often talk about certain things that science finds to be good for almost any health condition, and have made a habit of referencing what we call “The Usual Five Things™” (not really a trademark, by the way—just a figure of speech), which are:
- Have a good diet
- Get good exercise
- Get good sleep
- Reduce (or eliminate) alcohol consumption
- Don’t smoke
…and when we’re talking about a specific health consideration, we usually provide sources as to why each of them are particularly relevant, and pointers as to the what/how associated with them (ie what diet is good, how to get good sleep, etc).
Dr. Hyman’s “Five Pillars of Longevity” are based on observations from the world’s “Blue Zones”, the popular name for areas with an unusually high concentration of supercentenarians—Sardinia and Okinawa being famous examples, with a particular village in each being especially exemplary.
These Five Pillars of Longevity partially overlap with ours for three out of five, and they are:
- Good nutrition
- Optimized workouts
- Reduce stress
- Get quality sleep
- Find (and live) your purpose
We won’t argue against those! But what does he have to say, for each of them?
Good nutrition
Dr. Hyman advocates for a diet he calls “pegan”, which he considers to combine the paleo and vegan diets. Here at 10almonds, we generally advocate for the Mediterranean Diet because of the mountains of evidence for it, but his approach may be similar in some ways, since it looks to consume a majority plant diet, with some unprocessed meats/fish, limited dairy, and no grains.
By the science, honestly, we stand by the Mediterranean (which includes whole grains), but if for example your body may have issues of some kind with grains, his approach may be a worthy consideration.
Optimized workouts
For Dr. Hyman, this means getting in three kinds of exercise regularly:
- Aerobic/cardio, to look after your heart health
- Resistance training (e.g. weights or bodyweight strength-training) to look after your skeletal and muscular health
- Yoga or similar suppleness training, to look after your joint health
Can’t argue with that, and it can be all too easy to fall into the trap of thinking “I’m healthy because I do x” while forgetting y and/or z! Thus, a three-pronged approach definitely has its merits.
Reduce stress
Acute stress (say, a cold shower) is can confer some health benefits, but chronic stress is ruinous to our health and it ages us. So, reducing this is critical. Dr. Hyman advocates for the practice of mindfulness and meditation, as well as journaling.
Get quality sleep
Quality here, not just quantity. As well as the usual “sleep hygiene” advices, he has some more unorthodox methods, such as the use of binaural beats to increase theta-wave activity in the brain (and thus induce more restful sleep), and the practice of turning off Wi-Fi, on the grounds that Wi-Fi signals interfere with our sleep.
We were curious about these recommendations, so we checked out what the science had to say! Here’s what we found:
- Minimal Effects of Binaural Auditory Beats for Subclinical Insomnia: A Randomized Double-Blind Controlled Study
- Spending the night next to a router – Results from the first human experimental study investigating the impact of Wi-Fi exposure on sleep
In short: probably not too much to worry about in those regards. On the other hand, worrying less, unlike those two things, is a well-established way improve sleep!
(Surprised we disagreed with our featured expert on a piece of advice? Please know: you can always rely on us to stand by what the science says; we pride ourselves on being as reliable as possible!)
Find (and live!) your purpose
This one’s an ikigai thing, to borrow a word from Japanese, or finding one’s raison d’être, as we say in English using French, because English is like that. It’s about having purpose.
Dr. Hyman’s advice here is consistent with what many write on the subject, and it’d be an interesting to have more science on, but meanwhile, it definitely seems consistent with commonalities in the Blue Zone longevity hotspots, where people foster community, have a sense of belonging, know what they are doing for others and keep doing it because they want to, and trying to make the world—or even just their little part of it—better for those who will follow.
Being bitter, resentful, and self-absorbed is not, it seems a path to longevity. But a life of purpose, or even just random acts of kindness, may well be.
Share This Post
Related Posts
-
Yes, you still need to use sunscreen, despite what you’ve heard on TikTok
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Summer is nearly here. But rather than getting out the sunscreen, some TikTokers are urging followers to chuck it out and go sunscreen-free.
They claim it’s healthier to forgo sunscreen to get the full benefits of sunshine.
Here’s the science really says.
Karolina Grabowska/Pexels How does sunscreen work?
Because of Australia’s extreme UV environment, most people with pale to olive skin or other risk factors for skin cancer need to protect themselves. Applying sunscreen is a key method of protecting areas not easily covered by clothes.
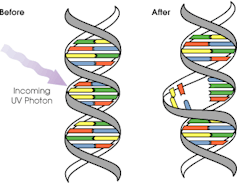
Sunscreen works by absorbing or scattering UV rays before they can enter your skin and damage DNA or supportive structures such as collagen.
When UV particles hit DNA, the excess energy can damage our DNA. This damage can be repaired, but if the cell divides before the mistake is fixed, it causes a mutation that can lead to skin cancers.
The energy from a particle of UV (a photon) causes DNA strands to break apart and reconnect incorrectly. This causes a bump in the DNA strand that makes it difficult to copy accurately and can introduce mutations. NASA/David Herring The most common skin cancers are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). Melanoma is less common, but is the most likely to spread around the body; this process is called metastasis.
Two in three Australians will have at least one skin cancer in their lifetime, and they make up 80% of all cancers in Australia.
Around 99% of skin cancers in Australia are caused by excessive exposure to UV radiation.
Excessive exposure to UV radiation also affects the appearance of your skin. UVA rays are able to penetrate deep into the skin, where they break down supportive structures such as elastin and collagen.
This causes signs of premature ageing, such as deep wrinkling, brown or white blotches, and broken capillaries.
Sunscreen can help prevent skin cancers
Used consistently, sunscreen reduces your risk of skin cancer and slows skin ageing.
In a Queensland study, participants either used sunscreen daily for almost five years, or continued their usual use.
At the end of five years, the daily-use group had reduced their risk of squamous cell carcinoma by 40% compared to the other group.
Ten years later, the daily use group had reduced their risk of invasive melanoma by 73%
Does sunscreen block the health-promoting properties of sunlight?
The answer is a bit more complicated, and involves personalised risk versus benefit trade-offs.
First, the good news: there are many health benefits of spending time in the sun that don’t rely on exposure to UV radiation and aren’t affected by sunscreen use.
Sunscreen only filters UV rays, not all light. Ron Lach/Pexels Sunscreen only filters UV rays, not visible light or infrared light (which we feel as heat). And importantly, some of the benefits of sunlight are obtained via the eyes.
Visible light improves mood and regulates circadian rhythm (which influences your sleep-wake cycle), and probably reduces myopia (short-sightedness) in children.
Infrared light is being investigated as a treatment for several skin, neurological, psychiatric and autoimmune disorders.
So what is the benefit of exposing skin to UV radiation?
Exposing the skin to the sun produces vitamin D, which is critical for healthy bones and muscles.
Vitamin D deficiency is surprisingly common among Australians, peaking in Victoria at 49% in winter and being lowest in Queensland at 6% in summer.
Luckily, people who are careful about sun protection can avoid vitamin D deficiency by taking a supplement.
Exposing the skin to UV radiation might have benefits independent of vitamin D production, but these are not proven. It might reduce the risk of autoimmune diseases such as multiple sclerosis or cause release of a chemical that could reduce blood pressure. However, there is not enough detail about these benefits to know whether sunscreen would be a problem.
What does this mean for you?
There are some benefits of exposing the skin to UV radiation that might be blunted by sunscreen. Whether it’s worth foregoing those benefits to avoid skin cancer depends on how susceptible you are to skin cancer.
If you have pale skin or other factors that increase you risk of skin cancer, you should aim to apply sunscreen daily on all days when the UV index is forecast to reach 3.
If you have darker skin that rarely or never burns, you can go without daily sunscreen – although you will still need protection during extended times outdoors.
For now, the balance of evidence suggests it’s better for people who are susceptible to skin cancer to continue with sun protection practices, with vitamin D supplementation if needed.
Katie Lee, PhD Candidate, Dermatology Research Centre, The University of Queensland and Rachel Neale, Principal research fellow, QIMR Berghofer Medical Research Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
PS, We Love You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
PS, we love you. With good reason!
There are nearly 20,000 studies on PS listed on PubMed alone, and its established benefits include:
- significantly improving memory
- potential reversal (!) of neurodegeneration
- reduction of stress activation
- improvement in exercise capacity
- it even helps avoid rejection of medical implants
We’ll explore some of these studies and give an overview of how PS does what it does. Just like the (otherwise unrelated) l-theanine we talked about a couple of weeks ago, it does do a lot of things.
PS = Cow Brain?!
Let’s first address a concern. You may have heard something along the lines of “hey, isn’t PS made from cow brain, and isn’t that Very Bad™ for humans, mad cow disease and all?”. The short answer is:
Firstly: ingesting cow brain tissue is indeed generally considered Very Bad™ for humans, on account of the potential for transmission of Bovine Spongiform Encephalopathy (BSE) resulting in its human equivalent, Creutzfeldt–Jakob Disease (CJD), whose unpleasantries are beyond the scope of this newsletter.
Secondly (and more pleasantly): whilst PS can be derived from bovine brain tissue, most PS supplements these days derive from soy—or sometimes sunflower lecithin. Check labels if unsure.
Using PS to Improve Other Treatments
In the human body, the question of tolerance brings us a paradox (not the tolerance paradox, important as that may also be): we must build and maintain a strong immune system capable of quickly adapting to new things, and then when we need medicines (or even supplements), we need our body to not build tolerance of them, for them to continue having an effect.
So, we’re going to look at a very hot-off-the-press study (Feb 2023), that found PS to “mediate oral tolerance”, which means that it helps things (medications, supplements etc.) that we take orally and want to keep working, keep working.
In the scientists’ own words (we love scientists’ own words because they haven’t been distorted by the popular press)…
❝This immunotherapy has been shown to prevent/reduce immune response against life-saving protein-based therapies, food allergens, autoantigens, and the antigenic viral capsid peptide commonly used in gene therapy, suggesting a broad spectrum of potential clinical applications. Given the good safety profile of PS together with the ease of administration, oral tolerance achieved with PS-based nanoparticles has a very promising therapeutic impact.❞
Nguyen et al, Feb 2023
In other words, to parse those two very long sentences into two shorter bullet points:
- It allows a lot of important treatments to continue working—treatments that the body would otherwise counteract
- It is very safe—and won’t harm the normal function of your immune system at large
This is also very consistent with one of the benefits we mentioned up top—PS helps avoid rejection of implants, something that can be a huge difference to health-related quality of life (HRQoL), never mind sometimes life itself!
What is PS Anyways, and How Does It Work?
Phosphatidylserine is a phospholipid, a kind of lipid, found in cell membranes. More importantly:
It’s a signalling agent, mainly for apoptosis, which in lay terms means: it tells cells when it’s time to die.
Cellular death sounds like a bad thing, but prompt and efficient cellular apoptosis (death) and resultant prompt and efficient autophagy (recycling) reduce the risk of your body making mistakes when creating new cells from old cells.
Think about photocopying:
- Situation A: You have a document, and you want to copy it. If you copy it before it gets messed up, your copy will look almost, if not exactly, like the original. It’ll be super easy to read.
- Situation B: You have a document, and you want to copy it, but you delay doing so for so long that the original is all scuffed and creased and has a coffee stain on it. These unwanted changes will get copied onto the new document, and any copy made of that copy will keep the problems too. It gets worse and worse each time.
So, using this over-simplifier analogy, the speed of ‘copying’ is a major factor in cellular aging. The sooner cells are copied, before something gets damaged, the better the copy will be.
So you really, really want to have enough PS (our bodies make it too, by the way) to signal promptly to a cell when its time is up.
You do not want cells soldiering on until they’re the biological equivalent of that crumpled up, coffee-stained sheet of paper.
Little wonder, then, that PS’ most commonly-sought benefit when it comes to supplementation is to help avoid age-related neurodegeneration (most notably, memory loss)!
Keeping the cells young means keeping the brain young!
PS’s role as a signalling agent doesn’t end there—it also has a lot to say to a wide variety of the body’s immunological cells, helping them know what needs to happen to what. Some things should be immediately eaten and recycled; other things need more extreme measures applied to them first, and yet other things need to be ignored, and so forth.
You can read more about that in Elsevier’s publication if you’re curious 🙂
Wow, what a ride today’s newsletter has been! We started at paracetamoxyfrusebendroneomycin, and got down to the nitty gritty with a bunch of hopefully digestible science!
We love feedback, so please let us know if we’re striking the balance right, and/or if you’d like to see more or less of something—there’s a feedback widget at the bottom of this email!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Women Living Deliciously – by Florence Given
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Wouldst thou like to live deliciously?” as the line goes, and this book answers that, and how.
While roundly aimed at women, as per the title, this book will be of benefit to anyone who finds that society has wanted to keep you small and contained, and that perhaps you were meant for better.
The book is divided into three sections:
- Excavating
- Planting
- Blooming
…which broadly describes the process the author takes us through, of:
- Digging up what is wrong
- Putting better things in place
- Enjoying life
This is important, because otherwise a lot of people will understandably exhort us to step 3 (enjoying life), without really thinking about steps 1 and 2.
Her wording of it is important too, it wasn’t just being flowery for floweriness’ sake—rather, it highlights the nature of the process: while “enjoy life” seems like a thing-in-itself (as Kant might say), in reality, there’s another necessary thing (or series of things) behind it. In contrast, the gardening metaphor renders it clear: how will your flowers bloom if you do not plant them? And what good will planting them do if the soil is not right for them?
So, she gives us a “ground upwards” therapeutic approach.
The style throughout is casual but sincere and heartfelt, and while this is a book of personal change rather than social change, it does reference feminism throughout so if that’s not for you, then neither is this book.
Bottom line: this is a lot more than just a pep talk or a book of platitudes; it’s a lot of concrete, applicable stuff to markedly live life better.
Click here to check out Women Living Deliciously, and live deliciously!
PS: we notice a one-star review on Amazon expressed disappointment upon discovering that this is not a recipe book. So please be aware, the only recipe in this book is the recipe for a fulfilling and vibrant life 😎
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: