Genital herpes is on the rise. Here’s what to know about this common infection
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The World Health Organization (WHO) recently released new estimates suggesting around 846 million people aged between 15 and 49 live with a genital herpes infection.
That’s equivalent to one in every five people from that age group.
At least one person each second (42 million people annually) contracts a new genital herpes infection.
So what is genital herpes, and are cases on the rise? Here’s what to know about this common infection.

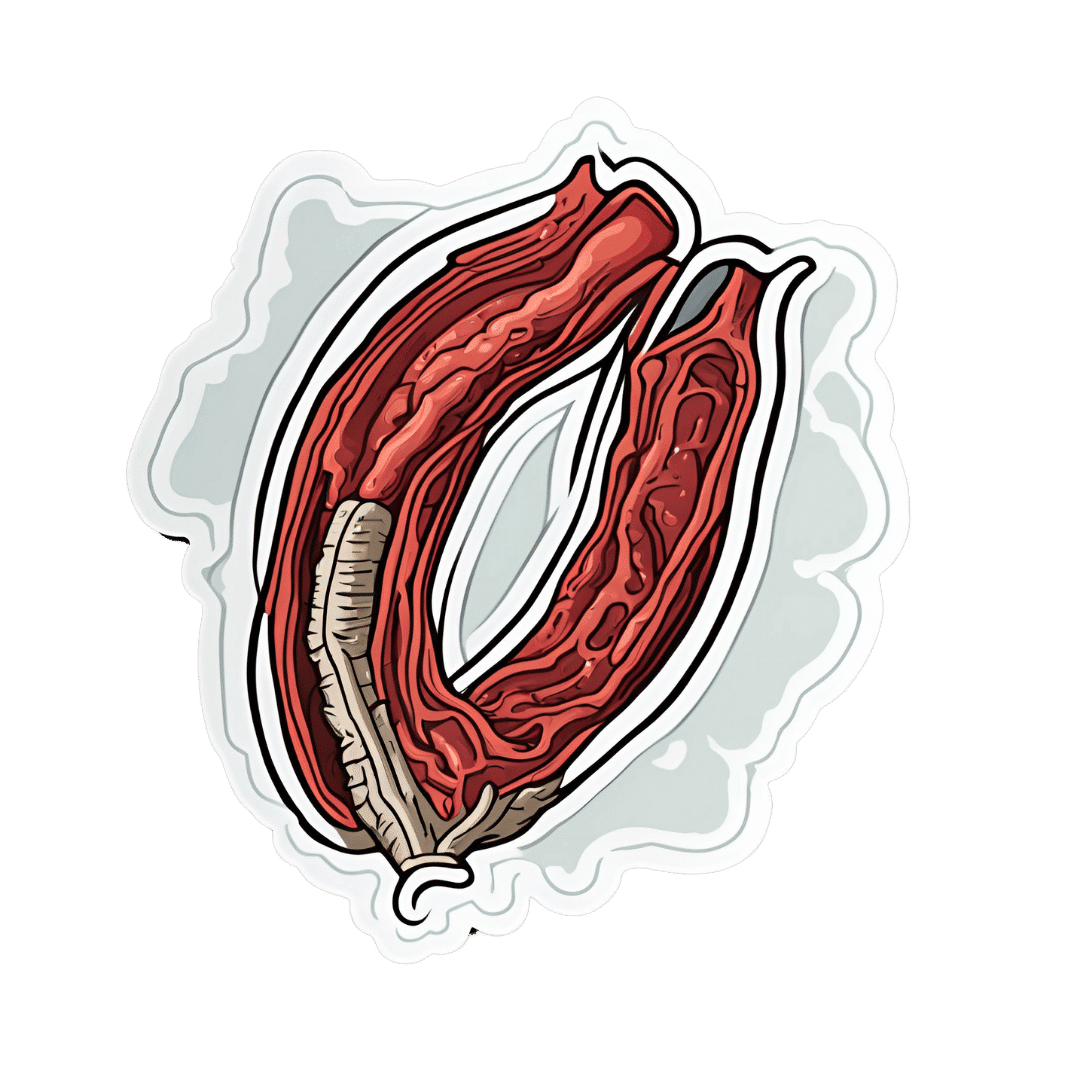
First, what causes genital herpes?
Genital herpes is a sexually transmitted infection (STI) caused by the herpes simplex virus, which also causes cold sores.
There are two types of herpes simplex virus, HSV-1 and HSV-2 (and it’s possible to be infected by both at the same time).
HSV-1 most commonly spreads through oral contact such as kissing or sharing infected objects such as lip balm, cups or utensils, and presents as cold sores (or oral herpes) around the mouth. But it can also be sexually transmitted to cause a genital herpes infection.
An estimated 3.8 billion people under the age of 50 (64%) globally have HSV-1.
HSV-2 is less prevalent, but almost always causes a genital herpes infection. Some 520 million people aged 15–49 (13%) worldwide are believed to have HSV-2.
The initial episode of genital herpes can be quite painful, with blisters, ulcers and peeling skin around the genitals over 7–10 days.
Not all people have severe (or any) initial symptoms. This means a person might not know they have been infected with a herpes virus.
Herpes is a lifelong infection, which means once you contract the virus, you have it forever. After an initial episode, subsequent episodes can occur, but are usually less painful or even symptom free.
Both oral and genital herpes are particularly easy to spread when you have active lesions (cold sores or genital ulcers). But even with no symptoms, herpes can still be spread to a partner.
And although relatively rare, oral herpes can be transmitted to the genital area, and genital herpes can be transmitted to the mouth through oral sex.
If an expectant mother exhibits a genital herpes infection close to childbirth, there are risks to the baby. A herpes infection can be very serious in a baby, and the younger the infant, the more vulnerable they are. This is also one reason why you should avoid kissing a baby on the mouth.
Changing trends
WHO’s recent figures brought together data from around the world to estimate the prevalence of genital herpes in 2020, compared with previous estimates in 2012 and 2016.
This data shows no significant difference in the prevalence of genital herpes caused by HSV-2 since 2016, but does highlight increases in genital herpes infections caused by HSV-1.
The estimated number of genital HSV-1 infections globally was nearly twice as high in 2020 compared with 2016 (376 million compared with 192 million).
A 2022 study looking at Australia, New Zealand and Canada found more than 60% of genital herpes infections are still caused by HSV-2. But this is declining by about 2% each year while new genital infections that result from HSV-1 are rising.

There’s no simple fix, but safe sex is important
Genital herpes causes a substantial disease burden and economic cost to health-care services.
With such a large proportion of the world’s population infected with HSV-1, evidence this virus is increasingly causing genital herpes is concerning.
There’s no cure for genital herpes, but some medications, such as antivirals, can help reduce the amount of virus present in the system. While this won’t kill it completely, it helps to prevent symptomatic genital herpes recurrences, improve quality of life, and minimise the risk of transmission.
To prevent the spread of genital herpes and other STIs, practise safe sex, particularly if you’re not sure of your partner’s sexual health. You need to use a barrier method such as condoms to protect against STIs (a contraceptive such as the pill won’t work). This includes during oral sex.
As herpes is now so common, testing is not usually included as part of a regular sexual health check-up, except for in specific circumstances such as during pregnancy or severe episodes.
So it’s wise not to let your guard down, even if your partner insists they have received the all-clear from a recent check-up.
If there are herpes lesions present around the genitals, avoid sex entirely. Even condoms are not fully effective at these times, as exposed areas can still transmit the infection.

Immune health
If you are infected with HSV-1 or HSV-2 it’s more likely symptoms will appear when you’re stressed, tired or overwhelmed. During these times, our immune system may not be as functional, and dormant viruses such as herpes can start to develop quickly in our bodies.
To reduce the risk of recurrent herpes infections, try to eat healthily, get at least seven hours of sleep each night if possible, and look out for when your body may be telling you to take a step back and relax. This self-care can go a long way towards keeping latent viruses at bay.
While the prevalence has increased significantly in recent years, we have not lost the war on genital herpes just yet. Safe sexual practices, education and awareness can help reduce its spread, and the stigma around it.
If you have personal concerns, you should discuss them with a medical professional.
Christian Moro, Associate Professor of Science & Medicine, Bond University and Charlotte Phelps, Senior Teaching Fellow in Medicine, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
CBD Oil’s Many Benefits
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
CBD Oil: What Does The Science Say?
First, a quick legal (and practical) note:
CBD and THC are both derived from the hemp or cannabis plant, but only the latter has euphoriant psychoactive effects, i.e., will get you high. We’re writing here about CBD derived from hemp and not containing THC (thus, will not get you high).
Laws and regulations differ far too much from place to place for us to try to advise here, so please check your own local laws and regulations. And also, while you’re at it, with your doctor and/or pharmacist.
As ever, this newsletter is for purposes of education and enjoyment, and does not constitute any kind of legal (or medical) advice.
With that in mind, onwards to today’s research review…
CBD for Pain Relief
CBD has been popularly touted as a pain relief panacea, and there are a lot of pop-science articles out there “debunking” this, but…
The science seems to back it up. We couldn’t find studies refuting the claim (of CBD as a viable pain relief option). We did, however, find research showing it was good against:
Note that that latter (itself a research review, not a single study, hence covering a lot of bases) describes it matter-of-factly, with no caveats or weasel-words, as:
“CBD, a non-euphoriant, anti-inflammatory analgesic with CB1 receptor antagonist and endocannabinoid modulating effects”
As a quick note: all of the above is about the topical use of CBD oil, not any kind of ingestion
CBD for Anxiety/Depression
There’s a well-cited study with what honestly we think was a bit of a small sample size, but compelling results within that:
A study published in the Brazilian Journal of Psychiatry tested the anxiety levels of 57 men in a simulated public speaking test.
Compared to placebo…
- Those who received 300mg of CBD experienced significantly reduced anxiety during the test.
- Those who received either 150mg or 600mg of CBD experienced more anxiety during the test than the 300mg group
- This means there’s a sweet spot to the dosage
There was also a clinical study that found CBD to have anti-depressant effects.
The methodology was a lot more robust, but the subjects were mice. We can’t have everything in one study, apparently! There is probably a paucity of human volunteers to have their brain slices looked at after tests, though.
Anyway, what makes this study interesting is that it measured quite an assortment of biological markers in the brain, and found that the CBD had a similar physiological effect to the antidepressant imipramine.
CBD for Treating Opioid Addiction
There are a lot of studies for this, both animal and human, but we’d like to put the spotlight on a human study (with the participation of heroin users) that found:
❝Within one week, CBD significantly reduced cravings, anxiety, resting heart rate, and salivary cortisol levels. No serious adverse effects were found.❞
This is groundbreaking because the very thing about heroin is that it’s so addictive and the body rapidly needs more and more of it. You might think “duh”, but most people don’t realize this part:
Heroin is attractive because it offers (and delivers) an immediate guaranteed “downer”, instant relaxation… with none of the bad side effects of, for example, alcohol. No nausea, no hangover, nothing.
The problem is that the body gets tolerant to heroin very quickly, meaning your doses need to get bigger and more frequent to have the same effect.
Before you know it, what seemed like an affordable “self-medication for a stressful life” is very much out of control! Many doctors have personally found this out the hard way.
So, it’s ruinous:
- first to your financial health, as the costs rapidly spiral
- then to your physical health, as you either suffer from withdrawal or eventually overdose
Consequently, heroin is an incredibly easy drug to get hooked onto, and incredibly difficult to get back off.
So CBD offering relief is really a game-changer.
And more…
CBD has been well-studied and found to be effective for a lot of things, more than we could hope to cover in a single edition here.
Some further reading that may interest you includes:
- CBD against Diabetes in mice / in vitro / in humans
- CBD against neurological diseases (in general, in humans)
- CBD against arthritis in mice / in humans
- CBD specifically against the pain of rheumatoid arthritis / of osteoarthritis
Let us know if there’s any of these (or other) conditions you’d like us to look more into the CBD-related research for, because there’s a lot! You can always hit reply to any of our emails, or use the feedback widget at the bottom
Read (and shop, if you want and it’s permitted where you are):
10 Best CBD Oils of 2023, According to the Forbes Health Advisory Board
Share This Post
-
An Elegant Defense – by Matt Richtel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a way, Richtel got the best and worst of the publication date lottery. This book, which he’d obviously been working on for however long, was published in March 2020. Yes, that March 2020. So, it obviously got a huge boost in sales that launced it to bestseller status, and/but it doesn’t actually discuss COVID at all.
What it does discuss, is—as one might expect—the immune system. Or really, the immune systems, plural, several systems working alongside each other. How we got to have such, how our immune functions work, where all the various immune cells come from and what part they play. What pathogens can do to fight and/or confuse (or even co-opt) our immune response, and what modern medicine can do to counteract the pathogens’ anti-countermeasure countermeasures. And how it can still go wrong.
The “Four Lives” promised in the subtitle are stories, and Richtel explains the immune system through specific people’s specific battles. In particular, a friend of his who had quite a remarkable battle against cancer, which was of course terrible for him, but illustrative for us.
The style of the book is very readably journalistic. The author is a Pulitzer-winning NYT journalist, and not normally a science writer. Here at 10almonds, “we like big bibliographies and we cannot lie”, and we didn’t get to enjoy that in this case. The book contained no bibliography (nor appropriate inline citations, nor equivalent footnotes). Maybe a future addition will include this.
Bottom line: there’s a lot of “science for the lay reader” here. While the lack of references is a big oversight, the book does give a very good overview of what both sides (immune response and pathogenic invasion) bring to the battle of your body.
Click here to check out Elegant Defense, and demystify immunology!
Share This Post
-
The Humor Habit – by Paul Osincup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ask not for whom the bell tolls… It could be tolling for anyone. Don’t worry about it.It’s probably fine.
More seriously (heh), laughter is good for healthy lifespan, also called healthspan. It eases stress and anxiety, gives our brains neurochemicals they need to function well, and is very pro-social too, which in turn has knock-on positive effects for our own mental health as well as those around us.
This book is a guide to cultivating that humor, finding the funny side in difficult times, and bringing a light-hearted silliness to moments where it helps.
The title suggests it’s about habit-building (and it is!) but it’s also about knowing where to look in your daily life for humorous potential and how to find it, and how to bring that into being in the moment.
The style is that of an instruction manual with a healthy dose of pop-science; first and foremost this is a practical guide, not a several-hundred page exhortation on “find things funny!”, but rather a “hey, psst, here are many sneaky insider tricks for finding the funny“.
Bottom line: this book is not only a very enjoyable read, but also very much the gift that keeps on giving, so treat yourself!
Click here to check out The Humor Habit, and strength your funny-bones!
Share This Post
Related Posts
-
Yoga Safety: Simple Guidelines
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I was wondering whether there were very simple, clear bullet points or instructions on things to be wary of in Yoga.❞
That’s quite a large topic, and not one that lends itself well to being conveyed in bullet points, but first we’ll share the article you sent us when sending this question:
Tips for Avoiding Yoga Injuries
…and next we’ll recommend the YouTube channel @livinleggings, whose videos we feature here from time to time. She (Liv) has a lot of good videos on problems/mistakes/injuries to avoid.
Here’s a great one to get you started:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lower Cholesterol Naturally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Lower Cholesterol, Without Statins
We’ll start this off by saying that lowering cholesterol might not, in fact, be critical or even especially helpful for everyone, especially in the case of women. We covered this more in our article about statins:
…which was largely informed by the wealth of data in this book:
The Truth About Statins – by Dr. Barbara H. Roberts
…which in turn, may in fact put a lot of people off statins. We’re not here to tell you don’t use them—they may indeed be useful or even critical for some people, as Dr. Roberts herself also makes makes clear. But rather, we always recommend learning as much as possible about what’s going on, to be able to make the most informed choices when it comes to what often might be literally life-and-death decisions.
On which note, if anyone would like a quick refresher on cholesterol, what it actually is (in its various forms) and what it does, why we need it, the problems it can cause anyway, then here you go:
Now, with all that in mind, we’re going to assume that you, dear reader, would like to know:
- how to lower your LDL cholesterol, and/or
- how to maintain a safe LDL cholesterol level
Because, while the jury’s out on the dangers of high LDL levels for women in particular, it’s clear that for pretty much everyone, maintaining them within well-established safe zones won’t hurt.
Here’s how:
Relax
Or rather, manage your stress. This doesn’t just reduce your acute risk of a heart attack, it also improves your blood metrics along the way, and yes, that includes not just blood pressure and blood sugars, but even triglycerides! Here’s the science for that, complete with numbers:
What are the effects of psychological stress and physical work on blood lipid profiles?
With that in mind, here’s…
How To Manage Chronic Stress (Even While Chronically Stressed)
Not chemically “relaxed”, though
While relaxing is important, drinking alcohol and smoking are unequivocally bad for pretty much everything, and this includes cholesterol levels:
Can We Drink To Good Health? ← this also covers popular beliefs about red wine and heart health, and the answer is no, we cannot
As for smoking, it is good to quit as soon as possible, unless your doctor specifically advises you otherwise (there are occasional situations where something else needs to be dealt with first, but not as many some might like to believe):
Addiction Myths That Are Hard To Quit
If you’re wondering about cannabis (CBD and/or THC), then we’d love to tell you about the effect these things have on heart health in general and cholesterol levels in particular, but the science is far too young (mostly because of the historic, and in some places contemporary, illegality cramping the research), and we could only find small, dubious, mutually contradictory studies so far. So the honest answer is: science doesn’t know this one, yet.
Exercise… But don’t worry, you can still stay relaxed
When it comes to heart health, the most important thing is keeping moving, so getting in those famous 150 minutes per week of moderate exercise is critical, and getting more is ideal.
240 minutes per week is a neat 40 minutes per day, by the way and is very attainable (this writer lives a 20-minute walk away from where she does her daily grocery shopping, thus making for a daily 40-minute round trip, not counting the actual shopping).
See: The Doctor Who Wants Us To Exercise Less, And Move More
If walking is for some reason not practical for you, here’s a whole list of fun options that don’t feel like exercise but are:
Manage your hormones
This one is mostly for menopausal women, though some people with atypical hormonal situations may find it applicable too.
Estrogen protects the heart… Until it doesn’t:
See also: World Menopause Day: Menopause & Cardiovascular Disease Risk
Here’s a great introduction to sorting it out, if necessary:
Dr. Jen Gunter: What You Should Have Been Told About Menopause Beforehand
Eat a heart-healthy diet
Shocking nobody, but it has to be said, for the sake of being methodical. So, what does that look like?
What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure
(it’s fiber in the #1 spot, but there’s a list of most important things there, that’s worth checking out and comparing it to what you habitually eat)
You can also check out the DASH (Dietary Approaches to Stop Hypertension) edition of the Mediterranean diet, here:
Four Ways To Upgrade The Mediterranean Diet
As for saturated fat (and especially trans-fats), the basic answer is to keep them to minimal, but there is room for nuance with saturated fats at least:
Can Saturated Fats Be Healthy?
And lastly, do make sure to get enough omega 3 fatty-acids:
What Omega-3s Really Do For Us
And enjoy plant sterols and stanols! This would need a whole list of their own, so here you go:
Take These To Lower Cholesterol! (Statin Alternatives)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Stretches To Relieve The Pain From Sitting & Poor Posture
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sitting is not good for the health, yes often it’s a necessity of modern life, especially if driving. To make things worse, it can often be difficult to remember to maintain good posture the rest of the time, if it’s not a habit. So, while reducing sitting and improving posture are both very good things to do, here are 5 stretches to mitigate the damage meanwhile:
Daily doses:
These are best done at a rate of 2–3 sets daily:
Cat-Cow Stretch:
- Benefits: eases spinal tension, boosts flexibility, improves posture.
- How to: start on all fours, alternate between arching and rounding your back while syncing with your breath (10-15 times).
Butterfly Stretch:
- Benefits: loosens tight hips, improves lower back flexibility, and enhances mobility for activities like squats.
- How to: sit with soles of feet together, let knees fall toward the floor, lean forward slightly, and hold for 30 seconds to 1 minute.
Supine Twist:
- Benefits: unlocks the spine, relieves post-workout tension, and relaxes the shoulders and hips.
- How to: lie on your back, bend knees, twist to one side while keeping shoulders grounded, and hold for 30 seconds to 1 minute per side.
Calf Stretch:
- Benefits: improves ankle mobility, loosens tight calves, and prevents injuries like Achilles tendinitis.
- How to: stand facing a wall, extend one leg back with the heel on the ground, lean into the stretch, or use a step for deeper stretches. Hold for 30 seconds to 1 minute per leg.
Child’s Pose:
- Benefits: decompresses the spine, relaxes hips, and relieves tension in back and thighs.
- How to: start on hands and knees, sit back onto your heels, stretch arms forward, and rest forehead on the mat. Hold for 30 seconds to 1 minute.
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
10 Tips To Reduce Morning Pain & Stiffness With Arthritis
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: