A Fresh Take On Hypothyroidism
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Three Rs To Boost Thyroid-Related Energy Levels
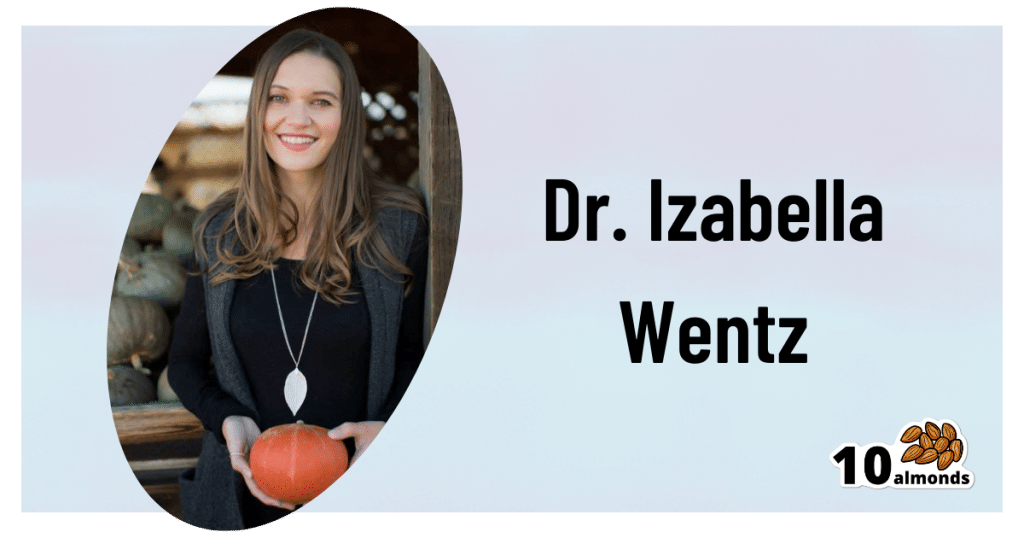
This is Dr. Izabella Wentz. She’s a doctor of pharmacology, and after her own diagnosis with Hashimoto’s thyroiditis, she has taken it up as her personal goal to educate others on managing hypothyroidism.
Dr. Wentz is also trained in functional medicine through The Institute for Functional Medicine, Kalish Functional Medicine, and the American Academy of Anti-Aging Medicine. She is a Fellow of the American Society of Consultant Pharmacists, and holds certifications in Medication Therapy Management as well as Advanced Diabetes Care through the American Pharmacists Association. In 2013, she received the Excellence in Innovation Award from the Illinois Pharmacists Association.
Dr. Wentz’s mission
Dr. Wentz was disenchanted by the general medical response to hypothyroidism in three main ways. She tells us:
- Thyroid patients are not diagnosed appropriately.
- For this, she criticises over-reliance on TSH tests that aren’t a reliable marker of thyroid function, especially if you have Hashimoto’s.
- Patients should be better optimized on their medications.
- For this, she criticizes many prescribed drugs that are actually pro-drugs*, that don’t get converted adequately if you have an underactive thyroid.
- Lifestyle interventions are often ignored by mainstream medicine.
- Medicines are great; they truly are. But medicating without adjusting lifestyle can be like painting over the cracks in a crumbling building.
*a “pro-drug” is what it’s called when the drug we take is not the actual drug the body needs, but is a precursor that will get converted to that actual drug we need, inside our body—usually by the liver, but not always. An example in this case is T4, which by definition is a pro-drug and won’t always get correctly converted to the T3 that a thyroid patient needs.
Well that does indeed sound worthy of criticism. But what does she advise instead?
First, she recommends a different diagnostic tool
Instead of (or at least, in addition to) TSH tests, she advises to ask for TPO tests (thyroid peroxidase), and a test for Tg antibodies (thyroglobulin). She says these are elevated for many years before a change in TSH is seen.
Next, identify the root cause and triggers
These can differ from person to person, but in countries that add iodine to salt, that’s often a big factor. And while gluten may or may not be a factor, there’s a strong correlation between celiac disease and Hashimoto’s disease, so it is worth checking too. Same goes for lactose.
By “checking”, here we mean testing eliminating it and seeing whether it makes a difference to energy levels—this can be slow, though, so give it time! It is best to do this under the guidance of a specialist if you can, of course.
Next, get to work on repairing your insides.
Remember we said “this can be slow”? It’s because your insides won’t necessarily bounce back immediately from whatever they’ve been suffering from for what’s likely many years. But, better late than never, and the time will pass anyway, so might as well get going on it.
For this, she recommends a gut-healthy diet with specific dietary interventions for hypothyroidism. Rather than repeat ourselves unduly here, we’ll link to a couple of previous articles of ours, as her recommendations match these:
She also recommends regular blood testing to see if you need supplementary TSH, TPO antibodies, and T3 and T4 hormones—as well as vitamin B12.
Short version
After diagnosis, she recommends the three Rs:
- Remove the causes and triggers of your hypothyroidism, so far as possible
- Repair the damage caused to your body, especially your gut
- Replace the thyroid hormones and related things in which your body has become deficient
Learn more
If you’d like to learn more about this, she offers a resource page, with resources ranging from on-screen information, to books you can get, to links to hook you up with blood tests if you need them, as well as recommended supplements to consider.
She also has a blog, which has an interesting relevant article added weekly.
Enjoy, and take care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Anti-Inflammatory Diet 101 (What to Eat to Fight Inflammation)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chronic inflammation is a cause and/or exacerbating factor in very many diseases. Arthritis, diabetes, and heart disease are probably top of the list, but there are lots more where they came from. And, it’s good to avoid those things. So, how to eat to avoid inflammation?
Let food be thy medicine
The key things to keep in mind, the “guiding principles” are to prioritize whole, minimally-processed foods, and enjoy foods with plenty of antioxidants. Getting a healthy balance of omega fatty acids is also important, which for most people means getting more omega-3 and less omega-6.
Shopping list (foods to prioritize) includes:
- fruits and vegetables in a variety of colors (e.g. berries, leafy greens, beats)
- whole grains, going for the most fiber-rich options (e.g. quinoa, brown rice, oats)
- healthy fats (e.g. avocados, nuts, seeds)
- fatty fish (e.g. salmon, mackerel, sardines) ← don’t worry about this if you’re vegetarian/vegan though, as the previous category can already cover it
- herbs and spices (e.g. turmeric, garlic, ginger)
Noping list (foods to avoid) includes:
- refined carbohydrates
- highly processed and/or fried foods
- red meats and/or processed meats (yes, that does mean that organic grass-fed farmers’ pinky-promise-certified holistically-raised beef is also off the menu)
- dairy products, especially if unfermented
For more information on each of these, plus advice on transitioning away from an inflammatory diet, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How to Prevent (or Reduce) Inflammation
Take care!
Share This Post
-
Meditation for Fidgety Skeptics – by Dan Harris
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you already meditate regularly, this book isn’t aimed at you (though you may learn a thing or two anyway—this reviewer, who has practiced meditation for the past 30 years, learned a thing!).
However, if you’re—as the title suggests—someone who hasn’t so far been inclined towards meditation, you could get the most out of this one. We’ll say more on this (obviously), but first, there’s one other group that may benefit from this book:
If you have already practiced meditation, and/or already understand and want its benefits, but never really made it stick as a habit.
Now, onto what you’ll get:
- A fair scientific overview of meditation as an increasingly evidence-based way to reduce stress and increase both happiness and productivity
- A good grounding in what meditation is and isn’t
- A how-to guide for building up a consistent meditation habit that won’t get kiboshed when you have a particularly hectic day—or a cold.
- An assortment of very common (and some less common) meditative practices to try
- Some great auxiliary tools to build cognitive restructuring into your meditation
We don’t usually cite other people’s reviews, but we love that one Amazon reviewer wrote:
❝I am 3 weeks into daily meditation practice, and I already notice that I am no longer constantly wishing for undercarriage rocket launchers while driving. I will always think your driving sucks, but I no longer wish you a violent death because of it. Yes, I live in Boston❞
Bottom line: if you’re not already meditating daily, this is definitely a book for you. And if you are, you may learn a thing or two anyway!
Click here to get your copy of Meditation For Fidgety Skeptics from Amazon today!
Share This Post
-
What happens when I stop taking a drug like Ozempic or Mounjaro?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hundreds of thousands of people worldwide are taking drugs like Ozempic to lose weight. But what do we actually know about them? This month, The Conversation’s experts explore their rise, impact and potential consequences.
Drugs like Ozempic are very effective at helping most people who take them lose weight. Semaglutide (sold as Wegovy and Ozempic) and tirzepatide (sold as Zepbound and Mounjaro) are the most well known in the class of drugs that mimic hormones to reduce feelings of hunger.
But does weight come back when you stop using it?
The short answer is yes. Stopping tirzepatide and semaglutide will result in weight regain in most people.
So are these medications simply another (expensive) form of yo-yo dieting? Let’s look at what the evidence shows so far.
It’s a long-term treatment, not a short course
If you have a bacterial infection, antibiotics will help your body fight off the germs causing your illness. You take the full course of medication, and the infection is gone.
For obesity, taking tirzepatide or semaglutide can help your body get rid of fat. However it doesn’t fix the reasons you gained weight in the first place because obesity is a chronic, complex condition. When you stop the medications, the weight returns.
Perhaps a more useful comparison is with high blood pressure, also known as hypertension. Treatment for hypertension is lifelong. It’s the same with obesity. Medications work, but only while you are taking them. (Though obesity is more complicated than hypertension, as many different factors both cause and perpetuate it.)
Obesity drugs only work while you’re taking them. KK Stock/Shutterstock Therefore, several concurrent approaches are needed; taking medication can be an important part of effective management but on its own, it’s often insufficient. And in an unwanted knock-on effect, stopping medication can undermine other strategies to lose weight, like eating less.
Why do people stop?
Research trials show anywhere from 6% to 13.5% of participants stop taking these drugs, primarily because of side effects.
But these studies don’t account for those forced to stop because of cost or widespread supply issues. We don’t know how many people have needed to stop this medication over the past few years for these reasons.
Understanding what stopping does to the body is therefore important.
So what happens when you stop?
When you stop using tirzepatide or semaglutide, it takes several days (or even a couple of weeks) to move out of your system. As it does, a number of things happen:
- you start feeling hungry again, because both your brain and your gut no longer have the medication working to make you feel full
When you stop taking it, you feel hungry again. Stock-Asso/Shutterstock - blood sugars increase, because the medication is no longer acting on the pancreas to help control this. If you have diabetes as well as obesity you may need to take other medications to keep these in an acceptable range. Whether you have diabetes or not, you may need to eat foods with a low glycemic index to stabilise your blood sugars
- over the longer term, most people experience a return to their previous blood pressure and cholesterol levels, as the weight comes back
- weight regain will mostly be in the form of fat, because it will be gained faster than skeletal muscle.
While you were on the medication, you will have lost proportionally less skeletal muscle than fat, muscle loss is inevitable when you lose weight, no matter whether you use medications or not. The problem is, when you stop the medication, your body preferentially puts on fat.
Is stopping and starting the medications a problem?
People whose weight fluctuates with tirzepatide or semaglutide may experience some of the downsides of yo-yo dieting.
When you keep going on and off diets, it’s like a rollercoaster ride for your body. Each time you regain weight, your body has to deal with spikes in blood pressure, heart rate, and how your body handles sugars and fats. This can stress your heart and overall cardiovascular system, as it has to respond to greater fluctuations than usual.
Interestingly, the risk to the body from weight fluctuations is greater for people who are not obese. This should be a caution to those who are not obese but still using tirzepatide or semaglutide to try to lose unwanted weight.
How can you avoid gaining weight when you stop?
Fear of regaining weight when stopping these medications is valid, and needs to be addressed directly. As obesity has many causes and perpetuating factors, many evidence-based approaches are needed to reduce weight regain. This might include:
- getting quality sleep
- exercising in a way that builds and maintains muscle. While on the medication, you will likely have lost muscle as well as fat, although this is not inevitable, especially if you exercise regularly while taking it
Prioritise building and maintaining muscle. EvMedvedeva/Shutterstock - addressing emotional and cultural aspects of life that contribute to over-eating and/or eating unhealthy foods, and how you view your body. Stigma and shame around body shape and size is not cured by taking this medication. Even if you have a healthy relationship with food, we live in a culture that is fat-phobic and discriminates against people in larger bodies
- eating in a healthy way, hopefully continuing with habits that were formed while on the medication. Eating meals that have high nutrition and fibre, for example, and lower overall portion sizes.
Many people will stop taking tirzepatide or semaglutide at some point, given it is expensive and in short supply. When you do, it is important to understand what will happen and what you can do to help avoid the consequences. Regular reviews with your GP are also important.
Read the other articles in The Conversation’s Ozempic series here.
Natasha Yates, General Practitioner, PhD Candidate, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Neuroaffirming care values the strengths and differences of autistic people, those with ADHD or other profiles. Here’s how
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve come a long way in terms of understanding that everyone thinks, interacts and experiences the world differently. In the past, autistic people, people with attention deficit hyperactive disorder (ADHD) and other profiles were categorised by what they struggled with or couldn’t do.
The concept of neurodiversity, developed by autistic activists in the 1990s, is an emerging area. It promotes the idea that different brains (“neurotypes”) are part of the natural variation of being human – just like “biodiversity” – and they are vital for our survival.
This idea is now being applied to research and to care. At the heart of the National Autism Strategy, currently in development, is neurodiversity-affirming (neuroaffirming) care and practice. But what does this look like?
Unsplash Reframing differences
Neurodiversity challenges the traditional medical model of disability, which views neurological differences solely through a lens of deficits and disorders to be treated or cured.
Instead, it reframes it as a different, and equally valuable, way of experiencing and navigating the world. It emphasises the need for brains that are different from what society considers “neurotypical”, based on averages and expectations. The term “neurodivergent” is applied to Autistic people, those with ADHD, dyslexia and other profiles.
Neuroaffirming care can take many forms depending on each person’s needs and context. It involves accepting and valuing different ways of thinking, learning and experiencing the world. Rather than trying to “fix” or change neurodivergent people to fit into a narrow idea of what’s considered “normal” or “better”, neuroaffirming care takes a person-centered, strengths-based approach. It aims to empower and support unique needs and strengths.
Neuroaffirming care can look different in a school or clinical setting. Shutterstock/Inna Reznik Adaptation and strengths
Drawing on the social model of disability, neuroaffirming care acknowledges there is often disability associated with being different, especially in a world not designed for neurodivergent people. This shift focuses away from the person having to adapt towards improving the person-environment fit.
This can include providing accommodations and adapting environments to make them more accessible. More importantly, it promotes “thriving” through greater participation in society and meaningful activities.
At school, at work, in clinic
In educational settings, this might involve using universal design for learning that benefits all learners.
For example, using systematic synthetic phonics to teach reading and spelling for students with dyslexia can benefit all students. It also could mean incorporating augmentative and alternative communication, such as speech-generating devices, into the classroom.
Teachers might allow extra time for tasks, or allow stimming (repetitive movements or noises) for self-regulation and breaks when needed.
In therapy settings, neuroaffirming care may mean a therapist grows their understanding of autistic culture and learns about how positive social identity can impact self-esteem and wellbeing.
They may make efforts to bridge the gap in communication between different neurotypes, known as the double empathy problem. For example, the therapist may avoid relying on body language or facial expressions (often different in autistic people) to interpret how a client is feeling, instead of listening carefully to what the client says.
Affirming therapy approaches with children involve “tuning into” their preferred way of communicating, playing and engaging. This can bring meaningful connection rather than compliance to “neurotypical” ways of playing and relating.
In workplaces, it can involve flexible working arrangements (hours, patterns and locations), allowing different modes of communication (such as written rather than phone calls) and low-sensory workspaces (for example, low-lighting, low-noise office spaces).
In public spaces, it can look like providing a “sensory space”, such as at large concerts, where neurodivergent people can take a break and self-regulate if needed. And staff can be trained to recognise, better understand and assist with hidden disabilities.
Combining lived experience and good practice
Care is neuroaffirmative when it centres “lived experience” in its design and delivery, and positions people with disability as experts.
As a result of being “different”, people in the neurodivergent community experience high rates of bullying and abuse. So neuroaffirming care should be combined with a trauma-informed approach, which acknowledges the need to understand a person’s life experiences to provide effective care.
Culturally responsive care acknowledges limited access to support for culturally and racially marginalised Autistic people and higher rates of LGBTQIA+ identification in the neurodivergent community.
In the workplace, we can acknowledge how difference can fuel ideas. Unsplash/Jason Goodman Authentic selves
The draft National Autism Strategy promotes awareness that our population is neurodiverse. It hopes to foster a more inclusive and understanding society.
It emphasises the societal and public health responsibilities for supporting neurodivergent people via public education, training, policy and legislation. By providing spaces and places where neurodivergent people can be their authentic, unmasked selves, we are laying the foundations for feeling seen, valued, safe and, ultimately, happy and thriving.
The author would like to acknowledge the assistance of psychologist Victoria Gottliebsen in drafting this article. Victoria is a member of the Oversight Council for the National Autism Strategy.
Josephine Barbaro, Associate Professor, Principal Research Fellow, Psychologist, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The End of Food Allergy – by Dr. Kari Nadeau & Sloan Barnett
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We don’t usually mention author credentials beyond their occupation/title. However, in this case it bears acknowledging at least the first line of the author bio:
❝Kari Nadeau, MD, PhD, is the director of the Sean N. Parker Center for Allergy and Asthma Research at Stanford University and is one of the world’s leading experts on food allergy❞
We mention this, because there’s a lot of quack medicine out there [in general, but especially] when it comes to things such as food allergies. So let’s be clear up front that Dr. Nadeau is actually a world-class professional at the top of her field.
This book is, by the way, about true allergies—not intolerances or sensitivities. It does touch on those latter two, but it’s not the main meat of the book.
In particular, most of the research cited is around peanut allergies, though the usual other common allergens are all discussed too.
The authors’ writing style is that of a science educator (Dr. Nadeau’s co-author, Sloan Barnett, is lawyer and health journalist). We get a clear explanation of the science from real-world to clinic and back again, and are left with a strong understanding, not just a conclusion.
The titular “End of Food Allergy” is a bold implicit claim; does the book deliver? Yes, actually.
The book lays out guidelines for safely avoiding food allergies developing in infants, and yes, really, how to reverse them in adults. But…
Big caveat:
The solution for reversing severe food allergies (e.g. “someone nearby touched a peanut three hours ago and now I’m in anaphylactic shock”), drug-assisted oral immunotherapy, takes 6–24 months of weekly several-hour-long clinic visits, relies on having a nearby clinic offering the service, and absolutely 100% cannot be done at home (on pain of probable death).
Bottom line: it’s by no means a magic bullet, but yes, it does deliver.
Click here to check out The End of Food Allergy to learn more!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Machine-Dispensed Coffee & Heart Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have written before about the health benefits (and risks) of coffee; for most people, the benefits far outweigh the risks, but individual cases may vary:
The Bitter Truth About Coffee (or is it?) ← this is a mythbusting edition
Speaking of bitterness; coffee has abundant polyphenols, which means…
- Coffee is the world’s biggest source of antioxidants
- 65% reduced risk of Alzheimer’s for coffee-drinkers
- 67% reduced risk of type 2 diabetes for coffee-drinkers
- 43% reduced risk of liver cancer for coffee-drinkers
- 53% reduced suicide risk for coffee-drinkers
See also: Why Bitter Is Better: Enjoy Bitter Foods For Your Heart & Brain ← while it says foods in the title, this does cover coffee too.
For mythbusting on caffeine specifically, enjoy: Caffeine: Cognitive Enhancer Or Brain-Wrecker?
There are also gut health benefits from drinking coffee, and what’s good for our gut is invariably good for our heart and brain:
Coffee & Your Gut ← gut bacteria do not, by the way, have a preference about how you make your coffee or whether it is caffeinated or not
The latest science on coffee and heart health
Specifically, on coffee and cholesterol levels, so for a quick primer on cholesterol, check out: Demystifying Cholesterol
High total cholesterol, and especially high LDL (“bad” cholesterol) is generally associated with cardiovascular disease, for the reasons outlined in the link above.
Recently, researchers at Uppsala University in Sweden examined the levels of cafestol and kahweol, which are both diterpenes, substances known to increase cholesterol levels, in coffee made by various methods, including those dispensed from coffee machines in workplaces.
Two samples were taken from each machine every 2–3 weeks, and the most common kinds of machines produced the highest concentrations of diterpenes. These machines are the ones that push hot water through a small amount of ground coffee, through a wide-gauge filter, dispensing coffee into a cup in about 30 seconds.
Actual espresso machines, which work on the same principle but usually with a finer filter, higher pressure, and slower dispensing of the drink, had widely varying results, quite possibly because there is (in most machines) a human element in how tightly the ground coffee is packed into the metal filter basket.
Simple filter coffee, whether made in a coffee percolator machine or made using the pour-over method, had the lowest concentrations of diterpenes.
You can read about this study here:
However!
We were curious as to how, exactly, cafestol and kahweol increase cholesterol levels.
It turns out that research in this area has been scant, because most mice aren’t affected by it in the way that most humans are, which has limited mouse model studies.
Scant does not mean non-existent, though, and the answer came by virtue of transgenic mice (specifically, apolipoprotein (apo) E*3-Leiden transgenic mice, which do have the same reaction to cafestol as humans), the paper title sums it up nicely:
You may be wondering: what does suppression of bile acid synthesis have to do with cholesterol levels?
To oversimplify it a bit: cafestol messes with cholesterol metabolism by interfering with the enzymes involved in cholesterol metabolism (specifically, regulatory enzymes found in bile acid).
As to what it actually does in that regard: it reduces LDLR (LDL receptor) mRNA levels by 37% (that figure’s an average of the specific enzymes, sterol 27-hydroxylase and oxysterol 7α-hydroxylase, which were reduced by 32% and 48%, respectively).
Why this matters in practical terms: cafestol does not add any cholesterol to our systems, it inhibits our ability to clear LDL cholesterol, thus promoting raised LDL cholesterol levels.
In other words: if you have little or no dietary cholesterol (no dietary cholesterol, for example, if you are vegan), then your body will only have the cholesterol that it made for itself because it needed it, and as such, the body won’t need to do the same kind of clean-up job that it would if you had that coffee with a double cheeseburger with extra bacon.
As such, if you have little or no dietary cholesterol, cafestol is unlikely to have anything like the same effect on cholesterol levels.
Disclaimer: this latter is technically a hypothesis, but based on sound reasoning:
It’s the same logic that says “if you do not drink alcohol, then eating a durian fruit, which inhibits aldehyde dehydrogenase, which the body uses to metabolize alcohol, will not cause alcohol-related problems for you”.
Want to know more?
We wrote previously on coffee and cafestol, along with some suggestions:
Health-Hack Your Coffee To Make Your Coffee Heart-Healthier!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: