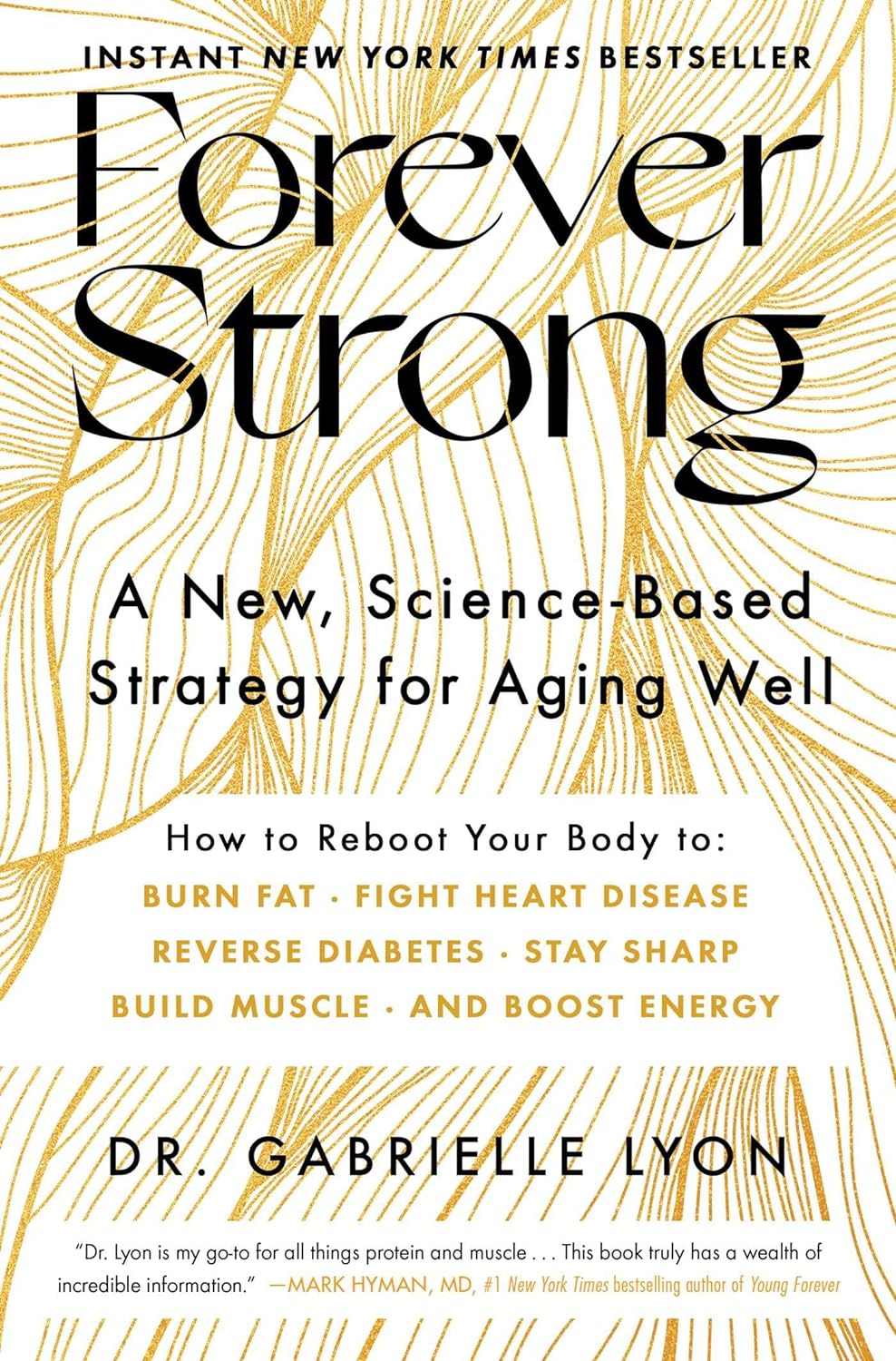
Forever Strong – by Dr. Gabrielle Lyon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Obesity kills a lot of people (as does medical neglect and malpractice when it comes to obese patients, but that is another matter), but often the biggest problem is not “too much fat” but rather “too little muscle”. This gets disguised a bit, because these factors often appear in the same people, but it’s a distinction that’s worthy of note.
Dr. Lyon lays out a lot of good hard science in this work, generally in the field of protein metabolism, but also with a keen eye on all manner of blood metrics (triglycerides, LDL/HDL, fasting blood sugars, assorted other biomarkers of metabolic health).
The style of this book is two books in one. It’s a very accessible pop-science book in its primary tone, with an extra layer of precise science and lots of references, for those who wish to dive into that.
In the category of criticism, the diet plan section of the book is rather meat-centric, but the goal of this is protein content, not meat per se, so substitutions can easily be made. That’s just one small section of the book, though, and it’s little enough a downside that even Dr. Mark Hyman (a popular proponent of plant-based nutrition) highly recommends the book.
Bottom line: if you’d like to be less merely fighting decline and more actually becoming healthier as you age, then this book will help you do just that.
Click here to check out Forever Strong, and level up your wellness as you age!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chew On This… But Don’t Swallow − by Dr. Blanche Grube & Anita Vasquez-Tibau
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Blanche Grube is a dentist with over 40 years of experience, and Anita Vasquez-Tibau is a well-respected research scientist with many peer-reviewed publications to her name, and both have lectured extensively.
So, what do they want us to know?
It’s mostly about the iatrogenic (i.e., caused by treatment) harm done by many common conventional dental practices (including dental mercury amalgams, metal crowns, root canals, implants, and even braces), and how we can avoid such, and enjoy better treatment instead.
After an introductory overview of the basics (and also where her own work came from in the first place, namely, her own root canals that were established as largely responsible for her leukemia), the largest part of the book is practical advice, laid out practically. What things come with what risks, what things get advertised differently than they really are, and which way to go in the case of unenviable situations where one must choose the “least bad” option out of a bunch of bad options.
Lastly, she discusses a range of solutions that can help side-step most problems, provided one implements them early. The good news is, they are “do these small things every day” recommendations, not “get this prophylactic surgical treatment” options. And yes, they are beyond the obvious of good dental hygiene, though she does cover that too.
The style is in part narrative, in part explanatory, and/but very readable throughout.
Bottom line: if you love having teeth and/but don’t love going to the dentist, this book will help you take good care of yourself, and also mean you can safely and informedly advocate for yourself if you do find yourself in the dentist’s office.
Click here to check out Chew On This… But Don’t Swallow, and protect your teeth!
Share This Post
-
The Minerals That Neutralize Viruses (While Being Harmless To Humans)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Researchers in Estonia and Sweden (it was a joint project, with five researchers from each country) have found a way to use titanium dioxide nanoparticles to neutralize viruses, including COVID & flu.
Titanium dioxide, yes, the common additive to foods, cosmetics, and more (in most cases, added as a non-bleaching whitening agent—simply, titanium dioxide is body-safe, white in color, and very reflective, making it a brilliant, shiny white). Also used in sunscreens, for its excellent safety profile and again, its full-spectrum reflectiveness.
See also: Who Screens The Sunscreens?
How it works
Some viruses, including coronaviruses and influenza viruses, have an outer layer that’s a lipid membrane. The researchers found (by testing against multiple viruses, and by using a control of silicotungstate polyoxymethalate nanoparticles), that the ability of titanium dioxide to bind to phospholipids (and ability that the silicotungstate polyoxymethalate doesn’t have) means that the nanoparticles bind to the virus’s outer case, thus preventing it from effectively entering human cells (which it needs to do in order to infect the host, as this is how viruses replicate themselves).
What this means, in practical terms
While more research will be needed to know whether this can be used in the medicinal sense, it already means that a nanoparticle spray can be used to create virus-neutralizing layers on surfaces and in air filters. This alone could greatly reduce transmission in enclosed spaces such as public transport (ranging from taxis to airplanes), as well as other places where people get packed into a small space.
If you have an air purifier at home, keep an eye out for when improved filters arrive on the market!
See also: What’s Lurking In Your Household Air?
Wait, you said “minerals”; are there more?
It seems so, but we can’t truly say for sure until they’ve been tested. However, the researchers see no reason why other small metal oxides that bind strongly to phospholipids shouldn’t work exactly the same way—which would include iron oxide (yes, as in rust) and aluminum oxide (the coating that automatically forms immediately when aluminum is exposed to oxygen (aluminum is so reactive to oxygen, that it’s almost impossible to get aluminum without an oxidized surface, unless you use something else to coat it, or cut it in an oxygen-free atmosphere and keep it there).
You can read the paper itself here:
Molecular mechanisms behind the anti corona virus activity of small metal oxide nanoparticles
And on a related note (different scientists, different science, similar principle, though, using mineral nanotechnology to kill microbes):
❝Researchers report that laboratory tests of their nanoflower-coated dressings demonstrate antibiotic, anti-inflammatory and biocompatible properties. They say these results show these tannic acid and copper(II) phosphate sprouted nanoflower bandages are promising candidates for treating infections and inflammatory conditions.❞
Read in full: This delicate nanoflower is downright deadly to bacteria
Want to learn more?
Check out:
Move over, COVID and Flu! We Have “Hybrid Viruses” To Contend With Now
Take care!
Share This Post
-
Sun-dried Tomatoes vs Black Olives – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sun-dried tomatoes to black olives, we picked the sun-dried tomatoes.
Why?
These common snack-salad items may seem similar in consistency, but their macros are very different: the tomatoes, being dried, have proportionally a lot more protein, carbs, and fiber. The olives, meanwhile, have more fat (and/but yes, a very healthy blend of fats). Note that these comments are true for the things themselves; be aware that sun-dried tomatoes are often sold in vegetable oil, which would obviously change the macros considerably and be much less healthy. So, for the sake of statistics, we’re assuming you got sun-dried tomatoes that aren’t soaked in oil. All in all, we’re calling this category a win for the tomatoes, but those fats from the olives are very good too.
In terms of vitamins, the sun-dried tomatoes being dried again means that the loss of water weight means the vitamin content is proportionally much higher; the tomatoes are higher in vitamins A, B1, B2, B3, B5, B6, B9, C, and K, while olives are higher only in vitamin E (but in their defence, olives have 165x more vitamin E than sun-dried tomatoes). Still, a win for sun-dried tomatoes here.
When it comes to minerals, it’s a similar story for the same reason; the loss of water weight in the sun-dried tomatoes makes them much more nutritionally dense; they are higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while the olives are higher only in sodium. Note, we’re looking at black olives today; green olives would be even higher in sodium than black ones, as they are “cured” for longer.
Lastly, in terms of polyphenols, they both have a lot of great things to bring, but sun-dried tomatoes are pretty much the richest natural source of lycopene, which itself a very powerful polyphenol even my general polyphenol standards, so we’d call this one a win for the sun-dried tomatoes too.
Want to learn more?
You might like to read:
Lycopene’s Benefits For The Gut, Heart, Brain, & More
Take care!
Share This Post
Related Posts
-
Keeping Your Kidneys Healthy (Especially After 60)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Keeping your kidneys happy: it’s more than just hydration!
Your kidneys are very busy organs. They filter waste products, balance hydration, pH, salt, and potassium. They also make some of our hormones, and are responsible for regulating red blood cell production too. They also handle vitamin D in a way our bodies would not work without, making them essential for calcium absorption and the health of our bones, and even muscular function.
So, how to keep them in good working order?
Yes, hydrate
This is obvious and may go without saying, but we try to not leave important things without saying. So yes, get plenty of water, spread out over the day (you can only usefully absorb so much at once!). If you feel thirsty, you’re probably already dehydrated, so have a little (hydrating!) drink.
Don’t smoke
It’s bad for everything, including your kidneys.
Look after your blood
Not just “try to keep it inside your body”, but also:
- Keep your blood sugar levels healthy (hyperglycemia can cause kidney damage)
- Keep your blood pressure healthy (hypertension can cause kidney damage)
Basically, your kidneys’ primary job of filtering blood will go much more smoothly if that blood is less problematic on the way in.
Watch your over-the-counter pill intake
A lot of PRN OTC NSAIDs (PRN = pro re nata, i.e. you take them as and when symptoms arise) (NSAIDs = Non-Steroidal Anti-Inflammatory Drugs, such as ibuprofen for example) can cause kidney damage if taken regularly.
Many people take ibuprofen (for example) constantly for chronic pain, especially the kind cause by chronic inflammation, including many autoimmune diseases.
It is recommended to not take them for more than 10 days, nor more than 8 per day. Taking more than that, or taking them for longer, could damage your kidneys temporarily or permanently.
Read more: National Kidney Foundation: Advice About Pain Medicines
See also: Which Drugs Are Harmful To Your Kidneys?
Get a regular kidney function checkup if you’re in a high risk group
Who’s in a high risk group?
- If you’re over 60
- If you have diabetes
- If you have cardiovascular disease
- If you have high blood pressure
- If you believe, or know, you have existing kidney damage
The tests are very noninvasive, and will be a urine and/or blood test.
For more information, see:
Kidney Testing: Everything You Need to Know
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Taurine’s Benefits For Heart Health And More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Taurine: Research Review
First, what is taurine, beyond being an ingredient in many energy drinks?
It’s an amino acid that many animals, including humans, can synthesize in our bodies. Some other animals—including obligate carnivores such as cats (but not dogs, who are omnivorous by nature) cannot synthesize taurine and must get it from food.
So, as humans are very versatile omnivorous frugivores by nature, we have choices:
- Synthesize it—no need for any conscious action; it’ll just happen
- Eat it—by eating meat, which contains taurine
- Supplement it—by taking supplements, including energy drinks, which generally (but not always) use a bioidentical lab-made taurine. Basically, lab-made taurine is chemically identical to the kind found in meat, it’s just cheaper and doesn’t involve animals as a middleman.
What does it do?
Taurine does a bunch of essential things, including:
- Maintaining hydration/electrolyte balance in cells
- Regulating calcium/magnesium balance in cells
- Forming bile salts, which are needed for digestion
- Supporting the integrity of the central nervous system
- Regulating the immune system and antioxidative processes
Thus, a shortage of taurine can lead to such issues as kidney problems, eye tissue damage (since the eyes are a particularly delicate part of the CNS), and cardiomyopathy.
If you want to read more, here’s an academic literature review:
Taurine: A “very essential” amino acid
On the topic of eye health, a 2014 study found that taurine is the most plentiful amino acid in the eye, and helps protect against retinal degeneration, in which they say:
❝We here review the evidence for a role of taurine in retinal ganglion cell survival and studies suggesting that this compound may be involved in the pathophysiology of glaucoma or diabetic retinopathy. Along with other antioxidant molecules, taurine should therefore be seriously reconsidered as a potential treatment for such retinal diseases❞
Read more: Taurine: the comeback of a neutraceutical in the prevention of retinal degenerations
Taurine for muscles… In more than sports!
We’d be remiss not to mention that taurine is enjoyed by athletes to enhance athletic performance; indeed, it’s one of its main selling-points:
See: Taurine in sports and exercise
But! It’s also useful for simply maintaining skeleto-muscular health in general, and especially in the context of age-related decline and chronic disease:
Taurine: the appeal of a safe amino acid for skeletal muscle disorders
On the topic of safety… How safe is it?
There’s an interesting answer to that question. Within safe dose ranges (we’ll get to that), taurine is not only relatively safe, but also, studies that looked to explore its risks found new benefits in the process. Specifically of interest to us were that it appears to promote better long-term memory, especially as we get older (as taurine levels in the brain decline with age):
Taurine, Caffeine, and Energy Drinks: Reviewing the Risks to the Adolescent Brain
^Notwithstanding the title, we assure you, the research got there; they said:
❝Interestingly, the levels of taurine in the brain decreased significantly with age, which led to numerous studies investigating the potential neuroprotective effects of supplemental taurine in several different experimental models❞
What experimental models were those? These ones:
- Taurine protects cerebellar neurons of the external granular layer
- Effects of taurine on alterations of neurobehavior and neurodevelopment key proteins expression
- Neuroprotective role of taurine in developing offspring affected by maternal alcohol consumption
…which were all animal studies, however.
The same systematic review also noted that not only was more research needed on humans, but also, existing studies have had a strong bias to male physiology (in both human and assorted other animal studies), so more diverse study is needed too.
What are the safe dose ranges?
Before we get to toxicity, let’s look at some therapeutic doses. In particular, some studies that found that 500mg 3x daily, i.e. 1.5g total daily, had benefits for heart health:
- Taurine and atherosclerosis
- The Anti-Inflammatory Effect of Taurine on Cardiovascular Disease
- Taurine supplementation has anti-atherogenic and anti-inflammatory effects before and after incremental exercise in heart failure
- Taurine Supplementation Lowers Blood Pressure and Improves Vascular Function in Prehypertension
- Taurine improves the vascular tone through the inhibition of TRPC3 function in the vasculature
Bottom line on safety: 3g/day has been found to be safe:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
America Worries About Health Costs — And Voters Want to Hear From Biden and Republicans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
President Joe Biden is counting on outrage over abortion restrictions to help drive turnout for his reelection. Former President Donald Trump is promising to take another swing at repealing Obamacare.
But around America’s kitchen tables, those are hardly the only health topics voters want to hear about in the 2024 campaigns. A new KFF tracking poll shows that health care tops the list of basic expenses Americans worry about — more than gas, food, and rent. Nearly 3 in 4 adults — and majorities of both parties — say they’re concerned about paying for unexpected medical bills and other health costs.
“Absolutely health care is something on my mind,” Rob Werner, 64, of Concord, New Hampshire, said in an interview at a local coffee shop in January. He’s a Biden supporter and said he wants to make sure the Affordable Care Act, also known as Obamacare, is retained and that there’s more of an effort to control health care costs.
The presidential election is likely to turn on the simple question of whether Americans want Trump back in the White House. (Nikki Haley, the former South Carolina governor and U.S. ambassador to the United Nations, remained in the race for the Republican nomination ahead of Super Tuesday, though she had lost the first four primary contests.) And neither major party is basing their campaigns on health care promises.
But in the KFF poll, 80% of adults said they think it’s “very important” to hear presidential candidates talk about what they’d do to address health care costs — a subject congressional and state-level candidates can also expect to address.
“People are most concerned about out-of-pocket expenses for health care, and rightly so,” said Andrea Ducas, vice president of health policy at the Center for American Progress, a Washington, D.C.-based progressive think tank.
Here’s a look at the major health care issues that could help determine who wins in November.
Abortion
Less than two years after the Supreme Court overturned the constitutional right to an abortion, it is shaping up to be the biggest health issue in this election.
That was also the case in the 2022 midterm elections, when many voters rallied behind candidates who supported abortion rights and bolstered Democrats to an unexpectedly strong showing. Since the Supreme Court’s decision, voters in six states — including Kansas, Kentucky, and Ohio, where Republicans control the legislatures — have approved state constitutional amendments protecting abortion access.
Polls show that abortion is a key issue to some voters, said Robert Blendon, a public opinion researcher and professor emeritus at the Harvard T.H. Chan School of Public Health. He said up to 30% across the board see it as a “personal” issue, rather than policy — and most of those support abortion rights.
“That’s a lot of voters, if they show up and vote,” Blendon said.
Proposals to further protect — or restrict — abortion access could drive voter turnout. Advocates are working to put abortion-related measures on the ballot in such states as Arizona, Florida, Missouri, and South Dakota this November. A push in Washington toward a nationwide abortion policy could also draw more voters to the polls, Blendon said.
A surprise ruling by the Alabama Supreme Court in February that frozen embryos are children could also shake up the election. It’s an issue that divides even the anti-abortion community, with some who believe that a fertilized egg is a unique new person deserving of full legal rights and protections, and others believing that discarding unused embryos as part of the in vitro fertilization process is a morally acceptable way for couples to have children.
Pricey Prescriptions
Drug costs regularly rank high among voters’ concerns.
In the latest tracking poll, more than half — 55% — said they were very worried about being able to afford prescription drugs.
Biden has tried to address the price of drugs, though his efforts haven’t registered with many voters. While its name doesn’t suggest landmark health policy, the Inflation Reduction Act, or IRA, which the president signed in August 2022, included a provision allowing Medicare to negotiate prices for some of the most expensive drugs. It also capped total out-of-pocket spending for prescription drugs for all Medicare patients, while capping the price of insulin for those with diabetes at $35 a month — a limit some drugmakers have extended to patients with other kinds of insurance.
Drugmakers are fighting the Medicare price negotiation provision in court. Republicans have promised to repeal the IRA, arguing that forcing drugmakers to negotiate lower prices on drugs for Medicare beneficiaries would amount to price controls and stifle innovation. The party has offered no specific alternative, with the GOP-led House focused primarily on targeting pharmacy benefit managers, the arbitrators who control most Americans’ insurance coverage for medicines.
Costs of Coverage
Health care costs continue to rise for many Americans. The cost of employer-sponsored health plans have hit new highs in the past few months, raising costs for employers and workers alike. Experts have attributed the increase to high demand and expensive prices for certain drugs and treatments, notably weight loss drugs, as well as to medical inflation.
Meanwhile, the ACA is popular. The KFF poll found that more adults want to see the program expanded than scaled back. And a record 21.3 million people signed up for coverage in 2024, about 5 million of them new customers.
Enrollment in Republican-dominated states has grown fastest, with year-over-year increases of 80% in West Virginia, nearly 76% in Louisiana, and 62% in Ohio, according to the Centers for Medicare & Medicaid Services.
Public support for Obamacare and record enrollment in its coverage have made it politically perilous for Republicans to pursue the law’s repeal, especially without a robust alternative. That hasn’t stopped Trump from raising that prospect on the campaign trail, though it’s hard to find any other Republican candidate willing to step out on the same limb.
“The more he talks about it, the more other candidates have to start answering for it,” said Jarrett Lewis, a partner at Public Opinion Strategies, a GOP polling firm.
“Will a conversation about repeal-and-replace resonate with suburban women in Maricopa County?” he said, referring to the populous county in Arizona known for being a political bellwether. “I would steer clear of that if I was a candidate.”
Biden and his campaign have pounced on Trump’s talk of repeal. The president has said he wants to make permanent the enhanced premium subsidies he signed into law during the pandemic that are credited with helping to increase enrollment.
Republican advisers generally recommend that their candidates promote “a market-based system that has the consumer much more engaged,” said Lewis, citing short-term insurance plans as an example. “In the minds of Republicans, there is a pool of people that this would benefit. It may not be beneficial for everyone, but attractive to some.”
Biden and his allies have criticized short-term insurance plans — which Trump made more widely available — as “junk insurance” that doesn’t cover care for serious conditions or illnesses.
Entitlements Are Off-Limits
Both Medicaid and Medicare, the government health insurance programs that cover tens of millions of low-income, disabled, and older people, remain broadly popular with voters, said the Democratic pollster Celinda Lake. That makes it unlikely either party would pursue a platform that includes outright cuts to entitlements. But accusing an opponent of wanting to slash Medicare is a common, and often effective, campaign move.
Although Trump has said he wouldn’t cut Medicare spending, Democrats will likely seek to associate him with other Republicans who support constraining the program’s costs. Polls show that most voters oppose reducing any Medicare benefits, including by raising Medicare’s eligibility age from 65. However, raising taxes on people making more than $400,000 a year to shore up Medicare’s finances is one idea that won strong backing in a recent poll by The Associated Press and NORC Center for Public Affairs Research.
Brian Blase, a former Trump health adviser and the president of Paragon Health Institute, said Republicans, if they win more control of the federal government, should seek to lower spending on Medicare Advantage — through which commercial insurers provide benefits — to build on the program’s efficiencies and ensure it costs taxpayers less than the traditional program.
So far, though, Republicans, including Trump, have expressed little interest in such a plan. Some of them are clear-eyed about the perils of running on changing Medicare, which cost $829 billion in 2021 and is projected to consume nearly 18% of the federal budget by 2032.
“It’s difficult to have a frank conversation with voters about the future of the Medicare program,” said Lewis, the GOP pollster. “More often than not, it backfires. That conversation will have to happen right after a major election.”
Addiction Crisis
Many Americans have been touched by the growing opioid epidemic, which killed more than 112,000 people in the United States in 2023 — more than gun deaths and road fatalities combined. Rural residents and white adults are among the hardest hit.
Federal health officials have cited drug overdose deaths as a primary cause of the recent drop in U.S. life expectancy.
Republicans cast addiction as largely a criminal matter, associating it closely with the migration crisis at the U.S. southern border that they blame on Biden. Democrats have sought more funding for treatment and prevention of substance use disorders.
“This affects the family, the neighborhood,” said Blendon, the public opinion researcher.
Billions of dollars have begun to flow to states and local governments from legal settlements with opioid manufacturers and retailers, raising questions about how to best spend that money. But it isn’t clear that the crisis, outside the context of immigration, will emerge as a campaign issue.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: