Elderberries vs Gooseberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing elderberries to gooseberries, we picked the elderberries.
Why?
These are both berries more likely found in your garden or local wood than in the supermarket, but if you have convenient access to them, they’re great options for eating!
In terms of macros, elderberry has nearly 2x the carbs and/but also nearly 2x the fiber, which in glycemic index terms, mostly cancels out (although: elderberry has the slightly lower glycemic index of the two)
In the category of vitamins, both are great but elderberries are winning with more of vitamins A, B1, B2, B3, B6, and C, while gooseberries have more vitamin B5.
When it comes to minerals, elderberries again lead with more calcium, iron, phosphorus, and potassium, while gooseberries have more magnesium.
There is an extra category today, which is “extra medicinal properties”, and elderberries have extra immune-boosting qualities, whereas gooseberries—while being as polyphenol-laden as one usually expects berries to be—do not confer the same kind of benefit in this regard.
You can check out the information about elderberry’s extra properties in the links section below; meanwhile, if you’re choosing between these berries, that’s the clear winner in every category today!
Want to learn more?
You might like to read:
- Herbs for Evidence-Based Health & Healing ← including elderberry
- Does It Come In A Pill? ← it does (but it doesn’t have to)
- Beyond Supplements: The Real Immune-Boosters! ← this article focusses on not-supplements, but does also have a supplement section
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Habits of a Happy Brain – by Dr. Loretta Graziano Breuning
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are lots of books on “happy chemicals” and “how to retrain your brain”, so what makes this one different?
Firstly, it focuses on four “happy chemicals”, not just one:
- Serotonin
- Dopamine
- Oxytocin
- Endorphins
It also looks at the role of cortisol, and how it caps off each of those just a little bit, to keep us just a little malcontent.
Behavioral psychology tends to focus most on dopamine, while prescription pharmaceuticals for happiness (i.e., most antidepressants) tend to focus on serotonin. Here, Dr. Breuning helps us understand the complex interplay of all of the aforementioned chemicals.
She also clears up many misconceptions, since a lot of people misattribute the functions of each of these.
Common examples include “I’m doing this for the serotonin!” when the activity is dopaminergic not serotoninergic, or considering dopamine “the love molecule” when oxytocin, or even something else like phenylethylamine would be more appropriate.
The above may seem like academic quibbles and not something of practical use, but if we want to biohack our brains, we need to do better than the equivalent of a chef who doesn’t know the difference between salt and sugar.
Where things are of less practical use, she tends to skip over or at least streamline them. For example, she doesn’t really discuss the role of post-dopamine prolactin in men—but the discussion of post-happiness cortisol covers the same ground anyway, for practical purposes.
Dr. Breuning also looks at where our evolved neurochemical responses go wrong, and lays out guidelines for such challenges as overcoming addiction, or embracing delayed gratification.
Bottom line: this book is a great user-manual for the brain. If you’d like to be happier and more effective with fewer bad habits, this is the book for you.
Click here to check out Habits of a Happy Brain, and get biohacking yours!
Share This Post
-
Get Fitter As You Go
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Jaime Seeman: Hard To Kill?
This is Dr. Jaime Seeman. She’s a board-certified obstetrician-gynecologist with a background in nutrition, exercise, and health science. She’s also a Fellow in Integrative Medicine, and a board-certified nutrition specialist.
However, her biggest focus is preventative medicine.
What does she want us to know?
The Five Pillars of being “Hard to Kill”!
As an athlete when she was younger, she got away with poor nutrition habits with good exercise, but pregnancy (thrice) brought her poor thyroid function, other hormonal imbalances, and pre-diabetes.
So, she set about getting better—not something the general medical establishment focuses on a lot! Doctors are pressured to manage symptoms, but are under no expectation to actually help people get better.
So, what are her five pillars?
Nutrition
Dr. Seeman unsurprisingly recommends a whole-foods diet with lots of plants, but unlike many plant-enjoyers, she is also an enjoyer of the ketogenic diet.
While keto-enthusiasts say “carbs are bad” and vegans say “meat is bad”, the reality is: both of those things can be bad, and in both cases, avoiding the most harmful varieties is a very good first step:
Movement
This is in two parts:
- get your 150 minutes of moderate exercise per week
- keep your body mobile!
See also:
Sleep
This one’s quite straightforward, and Dr. Seeman uncontroversially recommends getting 7–9 hours per night; yes, even you:
Mindset
This is key to Dr. Seeman’s approach, and it is about not settling for average, because the average is undernourished, overmedicated, sedentary, and suffering.
She encourages us all to keep working for better health, wherever we’re at. To not “go gentle into that good night”, to get stronger whatever our age, to showcase increasingly robust vitality as we go.
To believe we can, and then to do it.
Environment
That previous item usually won’t last beyond a 10-day health-kick without the correct environment.
As for how to make sure we have that? Check out:
Want more?
She does offer coaching:
Hard To Kill Academy: Master The Mindset To Maximize Your Years
Take care!
Share This Post
-
The Brain Alarm Signs That Warn Of Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to predicting age-related cognitive impairment:
First there are genetic factors to take into account (such as the APOE4 gene for Alzheimer’s), as well as things such as age and sex.
When it comes to sex, by the way, what matters here is hormones, which is why [it seems; this as technically as yet unproven with full rigor, but the hypothesis is sound and there is a body of evidence gradually being accumulated to support it] postmenopausal women with untreated menopause get Alzheimer’s at a higher rate and deteriorate more quickly:
Alzheimer’s Sex Differences May Not Be What They Appear
Next, there are obviously modifiable lifestyle factors to take into account, things that will reduce your risk such as getting good sleep, good diet, good exercise, and abstaining from alcohol and smoking, as well as oft-forgotten things such as keeping cognitively active and, equally importantly, socially active:
How To Reduce Your Alzheimer’s Risk
(the article outlines what matters the most in each of the above areas, by the way, so that you can get the most bang-for-buck in terms of lifestyle adjustments)
Lastly (in the category of risk factors), there are things to watch out for in the blood such as hypertension and high cholesterol.
Nipping it in the blood
In new research (so new it is still ongoing, but being at year 2 of a 4-year prospective study, they have published a paper with their results so far), researchers have:
- started with the premise “dementia is preceded by mild cognitive impairment”
- then, asked the question “what are the biometric signs of mild cognitive impairment?”
Using such tools as functional near-infrared spectroscopy (fNIRS) while the participants performed cognitive tasks, they were able to record changes in plasma levels of extracellular vesicles, assessing them with small-particle flow cytometry.
Translating from sciencese: they gave the participants mental tasks, and while they completed them, the researchers scanned their brains and monitored blood flow and the brain’s ability to compensate for any lack of it.
What they found:
- in young adults, blood flow increased, facilitating neurovascular coupling (this is good)
- in older adults, blood flow did not increase as much, but they engaged other areas of the brain to compensate, by what’s called functional connectivity (this is next best)
- in those with mild cognitive impairment, blood flow was reduced, and they did not have the ability to compensate by functional connectivity (this is not good)
They also performed a liquid biopsy, which sounds alarming but it just means they took some blood, and tested this for density of cerebrovascular endothelial extracellular vesicles (CEEVs), which—in more prosaic words—are bits from the cells lining the blood vessels in the brain.
People with mild cognitive impairment had more of these brain bits in their blood than those without.
You can read the paper itself here:
What this means
The science here is obviously still young (being as it is still in progress), but this will likely contribute greatly to early warning signs of dementia, by catching mild cognitive impairment in its early stages, by means of a simple blood test, instead of years of wondering before getting a dementia diagnosis.
And of course, forewarned is forearmed, so if this is something that could be done as a matter of routine upon hitting the age of, say, 65 and then periodically thereafter, it would catch a lot of cases while there’s still more time to turn things around.
As for how to turn things around, well, we imagine you have now read our “How To Reduce Your Alzheimer’s Risk” article linked up top (if not, we recommend checking it out), and there is also…
Do Try This At Home: The 12-Week Brain Fitness Program To Measurably Boost Your Brain
Take care!
When it comes to predicting age-related cognitive impairment:
First there are genetic factors to take into account (such as the APOE4 gene for Alzheimer’s), as well as things such as age and sex.
When it comes to sex, by the way, what matters here is hormones, which is why [it seems; this as technically as yet unproven with full rigor, but the hypothesis is sound and there is a body of evidence gradually being accumulated to support it] postmenopausal women with untreated menopause get Alzheimer’s at a higher rate and deteriorate more quickly:
Alzheimer’s Sex Differences May Not Be What They Appear
Next, there are obviously modifiable lifestyle factors to take into account, things that will reduce your risk such as getting good sleep, good diet, good exercise, and abstaining from alcohol and smoking, as well as oft-forgotten things such as keeping cognitively active and, equally importantly, socially active:
How To Reduce Your Alzheimer’s Risk
(the article outlines what matters the most in each of the above areas, by the way, so that you can get the most bang-for-buck in terms of lifestyle adjustments)
Lastly (in the category of risk factors), there are things to watch out for in the blood such as hypertension and high cholesterol.
Nipping it in the blood
In new research (so new it is still ongoing, but being at year 2 of a 4-year prospective study, they have published a paper with their results so far), researchers have:
- started with the premise “dementia is preceded by mild cognitive impairment”
- then, asked the question “what are the biometric signs of mild cognitive impairment?”
Using such tools as functional near-infrared spectroscopy (fNIRS) while the participants performed cognitive tasks, they were able to record changes in plasma levels of extracellular vesicles, assessing them with small-particle flow cytometry.
Translating from sciencese: they gave the participants mental tasks, and while they completed them, the researchers scanned their brains and monitored blood flow and the brain’s ability to compensate for any lack of it.
What they found:
- in young adults, blood flow increased, facilitating neurovascular coupling (this is good)
- in older adults, blood flow did not increase as much, but they engaged other areas of the brain to compensate, by what’s called functional connectivity (this is next best)
- in those with mild cognitive impairment, blood flow was reduced, and they did not have the ability to compensate by functional connectivity (this is not good)
They also performed a liquid biopsy, which sounds alarming but it just means they took some blood, and tested this for density of cerebrovascular endothelial extracellular vesicles (CEEVs), which—in more prosaic words—are bits from the cells lining the blood vessels in the brain.
People with mild cognitive impairment had more of these brain bits in their blood than those without.
You can read the paper itself here:
What this means
The science here is obviously still young (being as it is still in progress), but this will likely contribute greatly to early warning signs of dementia, by catching mild cognitive impairment in its early stages, by means of a simple blood test, instead of years of wondering before getting a dementia diagnosis.
And of course, forewarned is forearmed, so if this is something that could be done as a matter of routine upon hitting the age of, say, 65 and then periodically thereafter, it would catch a lot of cases while there’s still more time to turn things around.
As for how to turn things around, well, we imagine you have now read our “How To Reduce Your Alzheimer’s Risk” article linked up top (if not, we recommend checking it out), and there is also…
Do Try This At Home: The 12-Week Brain Fitness Program To Measurably Boost Your Brain
Take care!
Share This Post
Related Posts
-
Older people’s risk of abuse is rising. Can an ad campaign protect them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Elder abuse is an emerging public health and safety issue for communities of high-income countries.
The most recent data from Australia’s National Elder Abuse Prevalence Study, which surveyed 7,000 older people living in the community, found one in six self-reported being a victim of some form of abuse. But this did not include older people living in residential aged care or those with cognitive impairment, such as dementia – so is likely an underestimate.
This week the Australian government announced a multi-million dollar advertising campaign it hopes will address this serious and abhorrent abuse.
But is investing in community awareness of elder abuse the best use of scarce resources?
Nuttapong punna/Shutterstock What is elder abuse?
The World Health Organization (WHO) defines elder abuse as
[…] a single, or repeated act, or lack of appropriate action, occurring within any relationship where there is an expectation of trust which causes harm or distress to an older person.
Australia usually defines older people as those over 65. The exact age varies between countries depending on the overall health status of a nation and its vulnerable population groups. The WHO definitions of an older adult for sub-Saharan Africa, for example, is over 50. And there are communities with poorer health status and shorter lifespans within country borders, including our First Nations people.
Elder abuse can take on many different forms including physical, sexual, psychological, emotional, or financial abuse and neglect.
Living longer and wealthier
The number of older people in our society is greater than it has ever been. Around 17% Australians are aged 65 and over. By 2071, older Australians will make up between 25% and 27% of the total population.
People are living longer, accumulating substantial wealth and are vulnerable to abuse due to cognitive, physical or functional limitations.
Longer lifespans increase the time of possible exposure to abuse. Australian men aged 65 can expect to live another 20.2 years, while women aged 65 are likely to live another 22.8 years. (Life expectancy for First Nations men and women remains significantly shorter.)
Australian men are now 143 times more likely to reach the age of 100 than they were in 1901. Women are 82 times more likely.
Older people hold a large proportion of our nation’s wealth, making them vulnerable to financial abuse. Recent research by the Australian Council of Social Service and UNSW Sydney reveals older households (with people over 65) are 25% wealthier than the average middle-aged household and almost four times as wealthy as the average under-35 household.
Finally, older people have higher levels of impairment in their thinking, reasoning and physical function. Cognitive impairment, especially dementia, increases from one in 67 Australians under 60 to almost one in two people aged over 90.
Over half of Australians aged 65 years and over have disability. A particularly vulnerable group are the 258,374 older Australians who receive government-funded home care.
Who perpetrates elder abuse?
Sadly, most of the perpetrators of elder abuse are known to their victims. They are usually a member of the family, such as a life partner, child or grandchild.
Elder abuse causes significant illness and even early death. Financial abuse (across all ages) costs the community billions of dollars. Specific data for financial elder abuse is limited but indicates massive costs to individual survivors and the community.
Despite this, the level of awareness of elder abuse is likely to be much lower than for family violence or child abuse. This is partly due to the comparatively recent concept of elder abuse, with global awareness campaigns only developed over the past two decades.
Is an advertising campaign the answer?
The federal government has allocated A$4.8 million to an advertising campaign on television, online and in health-care clinics to reach the broader community. For context, last year the government spent $131.4 million on all media campaigns, including $32.6 million on the COVID vaccination program, $2 million on Japanese encephalitis and $3.2 million on hearing health awareness.
The campaign will likely benefit a small number of people who may be victims and have the capacity to report their perpetrators to authorities. It will generate some heartbreaking anecdotes. But it is unlikely to achieve broad community or systemic change.
There is little research evidence to show media campaigns alter the behaviour of perpetrators of elder abuse. And suggesting the campaign raises awareness of the issue for older people who are survivors of abuse sounds more like blaming victims than empowering them.
We don’t know how the government will judge the success of the campaign, so taxpayers won’t know whether a reasonable return on this investment was achieved. There may also be opportunity costs associated with the initiative – that is, lost opportunities for other actions and strategies. It could be more effective and efficient to target high-risk subgroups or to allocate funding to policy, practice reform or research that has direct tangible benefits for survivors. https://www.youtube.com/embed/DeK2kaqplTI?wmode=transparent&start=0 The Australian Human Rights Commission’s campaign from last year.
But the campaign can’t hurt, right?
Actually, the dangers that could come with an advertising campaign are two-fold.
First it may well oversimplify a highly complex issue. Identifying and managing elder abuse requires an understanding of the person’s vulnerabilities, their decision-making capacity and ability to consent, the will and preferences of victim and the role of perpetrator in the older person’s life. Abuse happens in the context of family and social networks. And reporting abuse can have consequences for the victim’s quality of life and care.
Consider the complexities of a case where an older person declines to have her grandson reported to police for stealing her money and medication because of her fear of becoming socially isolated. She might even feel responsible for the behaviour having raised the grandson and not want him to have a criminal record.
Secondly, a public campaign can create the illusion government and our institutions have the matter “in hand”. This might slow the opportunity for real change.
Ideally, the campaign will strengthen the argument for better policies, reporting procedures, policing, prosecution and judgements that are aligned. But these ends will also need investment in more research to build better communities that take good care of older people.
Joseph Ibrahim, Professor, Aged Care Medical Research Australian Centre for Evidence Based Aged Care, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Half of Australians in aged care have depression. Psychological therapy could help
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
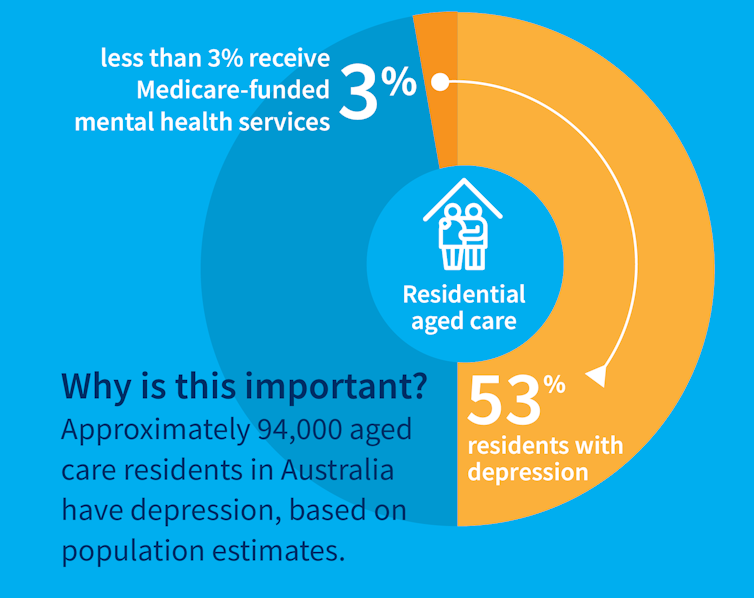
While many people maintain positive emotional wellbeing as they age, around half of older Australians living in residential aged care have significant levels of depression. Symptoms such as low mood, lack of interest or pleasure in life and difficulty sleeping are common.
Rates of depression in aged care appear to be increasing, and without adequate treatment, symptoms can be enduring and significantly impair older adults’ quality of life.
But only a minority of aged care residents with depression receive services specific to the condition. Less than 3% of Australian aged care residents access Medicare-subsidised mental health services, such as consultations with a psychologist or psychiatrist, each year.
Cochrane AustraliaInstead, residents are typically prescribed a medication by their GP to manage their mental health, which they often take for several months or years. A recent study found six in ten Australian aged care residents take antidepressants.
While antidepressant medications may help many people, we lack robust evidence on whether they work for aged care residents with depression. Researchers have described “serious limitations of the current standard of care” in reference to the widespread use of antidepressants to treat frail older people with depression.
Given this, we wanted to find out whether psychological therapies can help manage depression in this group. These treatments address factors contributing to people’s distress and provide them with skills to manage their symptoms and improve their day-to-day lives. But to date researchers, care providers and policy makers haven’t had clear information about their effectiveness for treating depression among older people in residential aged care.
The good news is the evidence we published today suggests psychological therapies may be an effective approach for people living in aged care.
We reviewed the evidence
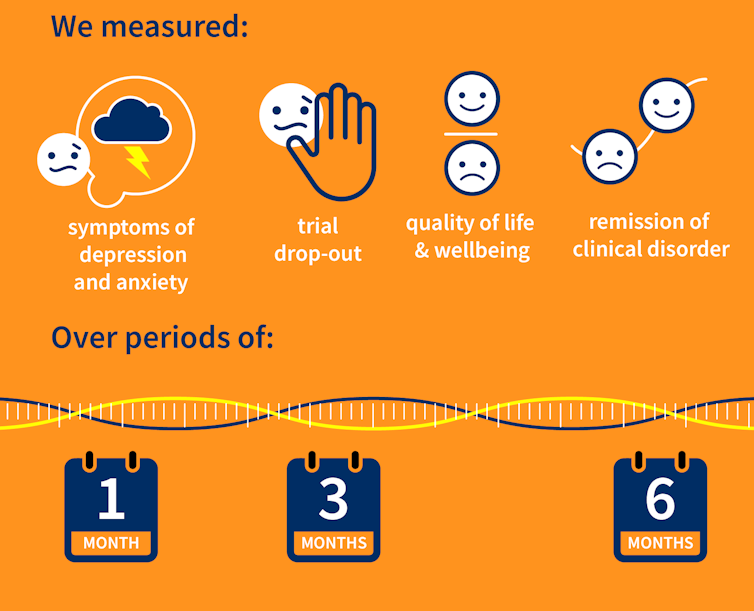
Our research team searched for randomised controlled trials published over the past 40 years that were designed to test the effectiveness of psychological therapies for depression among aged care residents 65 and over. We identified 19 trials from seven countries, including Australia, involving a total of 873 aged care residents with significant symptoms of depression.
The studies tested several different kinds of psychological therapies, which we classified as cognitive behavioural therapy (CBT), behaviour therapy or reminiscence therapy.
CBT involves teaching practical skills to help people re-frame negative thoughts and beliefs, while behaviour therapy aims to modify behaviour patterns by encouraging people with depression to engage in pleasurable and rewarding activities. Reminiscence therapy supports older people to reflect on positive or shared memories, and helps them find meaning in their life history.
The therapies were delivered by a range of professionals, including psychologists, social workers, occupational therapists and trainee therapists.
Cochrane AustraliaIn these studies, psychological therapies were compared to a control group where the older people did not receive psychological therapy. In most studies, this was “usual care” – the care typically provided to aged care residents, which may include access to antidepressants, scheduled activities and help with day-to-day tasks.
In some studies psychological therapy was compared to a situation where the older people received extra social contact, such as visits from a volunteer or joining in a discussion group.
What we found
Our results showed psychological therapies may be effective in reducing symptoms of depression for older people in residential aged care, compared with usual care, with effects lasting up to six months. While we didn’t see the same effect beyond six months, only two of the studies in our review followed people for this length of time, so the data was limited.
Our findings suggest these therapies may also improve quality of life and psychological wellbeing.
Psychological therapies mostly included between two and ten sessions, so the interventions were relatively brief. This is positive in terms of the potential feasibility of delivering psychological therapies at scale. The three different therapy types all appeared to be effective, compared to usual care.
However, we found psychological therapy may not be more effective than extra social contact in reducing symptoms of depression. Older people commonly feel bored, lonely and socially isolated in aged care. The activities on offer are often inadequate to meet their needs for stimulation and interest. So identifying ways to increase meaningful engagement day-to-day could improve the mental health and wellbeing of older people in aged care.
Some limitations
Many of the studies we found were of relatively poor quality, because of small sample sizes and potential risk of bias, for example. So we need more high-quality research to increase our confidence in the findings.
Many of the studies we reviewed were also old, and important gaps remain. For example, we are yet to understand the effectiveness of psychological therapies for people from diverse cultural or linguistic backgrounds.
Separately, we need better research to evaluate the effectiveness of antidepressants among aged care residents.
What needs to happen now?
Depression should not be considered a “normal” experience at this (or any other) stage of life, and those experiencing symptoms should have equal access to a range of effective treatments. The royal commission into aged care highlighted that Australians living in aged care don’t receive enough mental health support and called for this issue to be addressed.
While there have been some efforts to provide psychological services in residential aged care, the unmet need remains very high, and much more must be done.
The focus now needs to shift to how to implement psychological therapies in aged care, by increasing the competencies of the aged care workforce, training the next generation of psychologists to work in this setting, and funding these programs in a cost-effective way.
Tanya Davison, Adjunct professor, Health & Ageing Research Group, Swinburne University of Technology and Sunil Bhar, Professor of Clinical Psychology, Swinburne University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Relieve GERD and Acid Reflux with Stretches and Exercises
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Looking for relief from GERD or acid reflux? Today we’re featuring an amazing video by Dr. Jo, packed with stretches and exercises designed to ease those symptoms.
Here’s a quick rundown, in case you don’t have time to watch the whole video.
If you’re not familiar with GERD, you can find our simple explanation of GERD here. Or, if you’re on the other end of the spectrum and want to do a deeper dive on the topic, we reviewed a great book on the topic).
1. Mobilize Your SEM Muscle
The sternocleidomastoid (SEM) muscle, if tight, can aggravate acid reflux. Dr. Jo shows how to gently mobilize this muscle by turning your head while holding the SEM in place. It’s simple but effective.
2. Portrait Pose Stretch
Stretch out that SEM with the Portrait Pose. Place your hand on your collarbone, turn your head away, side bend, and look up. Hold for 30 seconds. You’ll feel the tension melting away.
3. Seated Cat-Cow Motion
Open up your stomach area with this easy exercise. Sit down, roll your body forward, arch your back (Cow), then curl your spine and tuck your chin (Cat). Alternate for 30 seconds and feel the difference.
4. Quadruped Cat-Cow with Breathing
Similar to the seated cat-cow, the quadruped cat-cow focuses on flexing the lower spine whilst on all fours. Bonus tip: focus on deep belly breathing during the exercise. This helps improve digestion and ease reflux symptoms.
5. Exaggerated Pelvic Tilt
Lie on your back and tilt your pelvis back and forth. This loosens up the abdominal area and helps everything flow better.
6. Trunk Rotation
Lie down, bend your knees, and rotate them to one side. Hold for 30 seconds, then switch sides. It’s a great way to relax and stretch your abdominal muscles.
We know this is a quick overview (sorry if it seems rushed!), but if you have a few more minutes on your hand you can watch the whole video below.
Feel better soon! And if you have any favorite tips or videos to share, email us at 10almonds.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: