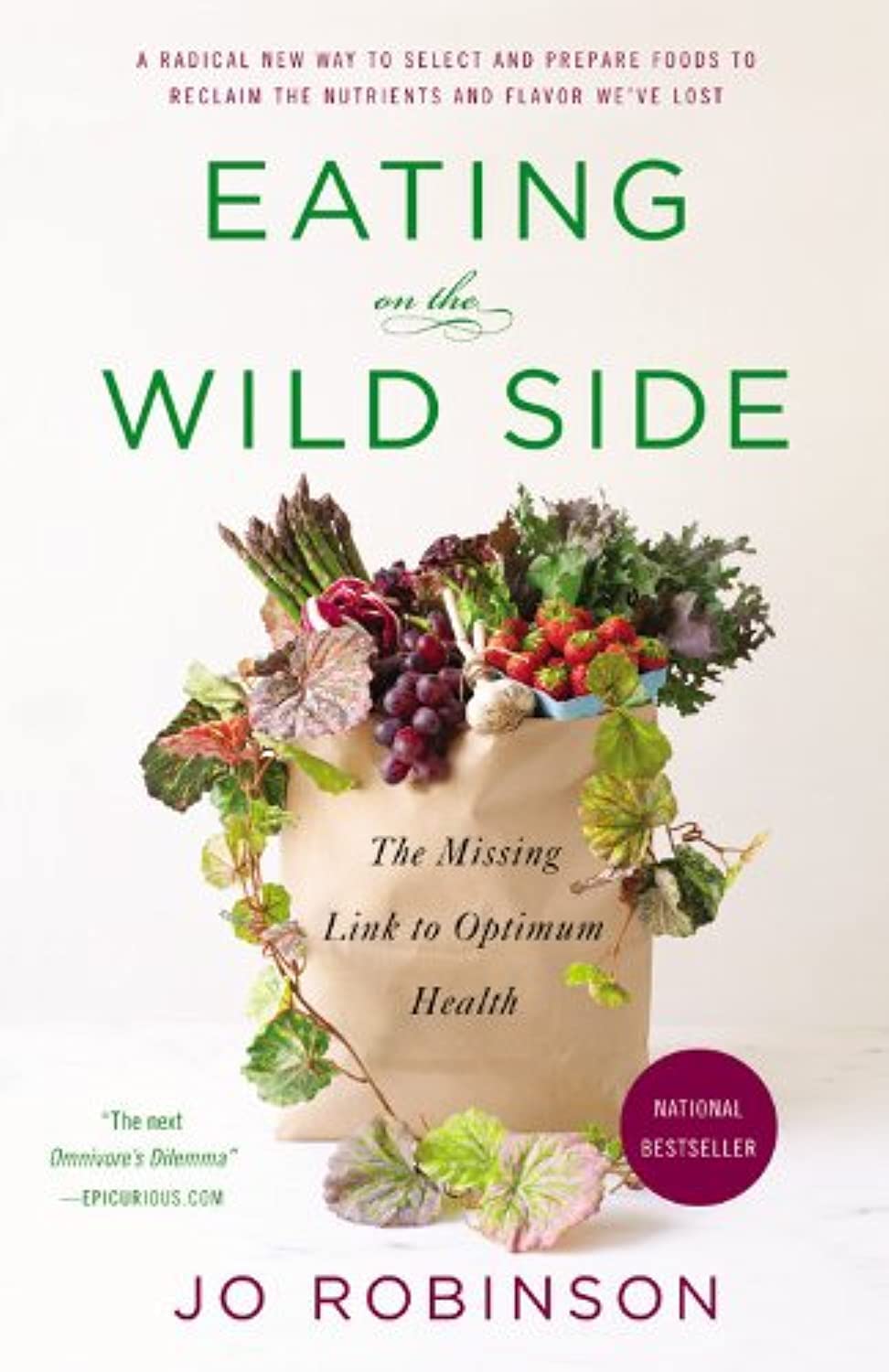
Eating on the Wild Side: – by Jo Robinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author is an investigative journalist, and it shows here, as she leaves no stone unturned in her quest for the truth in the face of many food myths.
She covers a lot of “popular wisdom” things that are varyingly true or false, or sometimes even both—in the case of food lore that’s a good rule of thumb, but has notable exceptions (e.g. “more colorful and/or darker-colored fruits/vegetables contain more nutrients”, which is a very good rule of thumb until one meets a cauliflower, for example).
She also covers food preparation myths, and how, to give one example, in spite of the popularity of “less cooked is better”, in some cases certain cooking methods will indeed destroy nutrients; in others, certain cooking methods will improve nutritional availability. Either by destroying an adjacent antinutrient (e.g. phytates), or by breaking something down into a more manageable form that our body can absorb. Knowing which is which, is important.
The book is organized by kinds of food, and does exclusively cover plants, but there’s more than enough material for any omnivore to enjoy.
The style is… Journalistic, it would be fair to say. Which is not surprising, given the author. But it means that it is written in a fairly narrative way, to draw the reader in and make it an enjoyable read while still being informative in all parts (there is no padding). In terms of science, the in-the-prose science is as minimal as possible to still convey what needs to be conveyed, while 25 pages of bibliography stack up at the end to show that indeed, this journalist cites sources.
Bottom line: this is a really enjoyable book, packed with a wealth of knowledge, and is perfect to uplift your cooking by knowing your ingredients a little more intimately!
Click here to check out Eating On The Wild Side, and, enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Avoid Carer Burnout (Without Dropping Care)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Avoid Carer Burnout
Sometimes in life we find ourselves in a caregiving role.
Maybe we chose it. For example, by becoming a professional carer, or even just by being a parent.
Oftentimes we didn’t. Sometimes because our own parents now need care from us, or because a partner becomes disabled.
Philosophical note: an argument could be made for that latter also having been a pre-emptive choice; we probably at some point said words to the effect of “in sickness and in health”, hopefully with free will, and hopefully meant it. And of course, sometimes we enter into a relationship with someone who is already disabled.
But, we are not a philosophy publication, and will henceforth keep to the practicalities.
First: are you the right person?
Sometimes, a caregiving role might fall upon you unasked-for, and it’s worth considering whether you are really up for it. Are you in a position to be that caregiver? Do you want to be that caregiver?
It may be that you do, and would actively fight off anyone or anything that tried to stop you. If so, great, now you only need to make sure that you are actually in a position to provide the care in question.
It may be that you do want to, but your circumstances don’t allow you to do as good a job of it as you’d like, or it means you have to drop other responsibilities, or you need extra help. We’ll cover these things later.
It may be that you don’t want to, but you feel obliged, or “have to”. If that’s the case, it will be better for everyone if you acknowledge that, and find someone else to do it. Nobody wants to feel a burden, and nobody wants someone providing care to be resentful of that. The result of such is two people being miserable; that’s not good for anyone. Better to give the job to someone who actually wants to (a professional, if necessary).
So, be honest (first with yourself, then with whoever may be necessary) about your own preferences and situation, and take steps to ensure you’re only in a caregiving role that you have the means and the will to provide.
Second: are you out of your depth?
Some people have had a life that’s prepared them for being a carer. Maybe they worked in the caring profession, maybe they have always been the family caregiver for one reason or another.
Yet, even if that describes you… Sometimes someone’s care needs may be beyond your abilities. After all, not all care needs are equal, and someone’s condition can (and more often than not, will) deteriorate.
So, learn. Learn about the person’s condition(s), medications, medical equipment, etc. If you can, take courses and such. The more you invest in your own development in this regard, the more easily you will handle the care, and the less it will take out of you.
And, don’t be afraid to ask for help. Maybe the person knows their condition better than you, and certainly there’s a good chance they know their care needs best. And certainly, there are always professionals that can be contacted to ask for advice.
Sometimes, a team effort may be required, and there’s no shame in that either. Whether it means enlisting help from family/friends or professionals, sometimes “many hands make light work”.
Check out: Caregiver Action Network: Organizations Near Me
A very good resource-hub for help, advice, & community
Third: put your own oxygen mask on first
Like the advice to put on one’s own oxygen mask first before helping others (in the event of a cabin depressurization in an airplane), the rationale is the same here. You can’t help others if you are running on empty yourself.
As a carer, sometimes you may have to put someone else’s needs above yours, both in general and in the moment. But, you do have needs too, and cannot neglect them (for long).
One sleepless night looking after someone else is… a small sacrifice for a loved one, perhaps. But several in a row starts to become unsustainable.
Sometimes it will be necessary to do the best you can, and accept that you cannot do everything all the time.
There’s a saying amongst engineers that applies here too: “if you don’t schedule time for maintenance, your equipment will schedule it for you”.
In other words: if you don’t give your body rest, your body will break down and oblige you to rest. Please be aware this goes for mental effort too; your brain is just another organ.
So, plan ahead, schedule breaks, find someone to take over, set up your cared-for-person with the resources to care for themself as well as possible (do this anyway, of course—independence is generally good so far as it’s possible), and make the time/effort to get you what you need for you. Sleep, distraction, a change of scenery, whatever it may be.
Lastly: what if it’s you?
If you’re reading this and you’re the person who has the higher care needs, then firstly:all strength to you. You have the hardest job here; let’s not forget that.
About that independence: well-intentioned people may forget that, so don’t be afraid to remind them when “I would prefer to do that myself”. Maintaining independence is generally good for the health, even if sometimes it is more work for all concerned than someone else doing it for you. The goal, after all, is your wellbeing, so this shouldn’t be cast aside lightly.
On the flipside: you don’t have to be strong all the time; nobody should.
Being disabled can also be quite isolating (this is probably not a revelation to you), so if you can find community with other people with the same or similar condition(s), even if it’s just online, that can go a very, very long way to making things easier. Both practically, in terms of sharing tips, and psychologically, in terms of just not feeling alone.
See also: How To Beat Loneliness & Isolation
Share This Post
-
How To Leverage Placebo Effect For Yourself
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Placebo Effect: Making Things Work Since… Well, A Very Long Time Ago
The placebo effect is a well-known, well-evidenced factor that is very relevant when it comes to the testing and implementation of medical treatments:
NIH | National Center for Biotechnology Information | Placebo Effect
Some things that make placebo effect stronger include:
- Larger pills instead of small ones: because there’s got to be more going on in there, right?
- Thematically-colored pills: e.g. red for stimulant effects, blue for relaxing effects
- Things that seem expensive: e.g. a well-made large heavy machine, over a cheap-looking flimsy plastic device. Similarly, medication from a small glass jar with a childproof lock, rather than popped out from a cheap blister-pack.
- Things that seem rational: if there’s an explanation for how it works that you understand and find rational, or at least you believe you understand and find rational ← this works in advertising, too; if there’s a “because”, it lands better almost regardless of what follows the word “because”
- Things delivered confidently by a professional: this is similar to the “argument from authority” fallacy (whereby a proposed authority will be more likely trusted, even if this is not their area of expertise at all, e.g. celebrity endorsements), but in the case of placebo trials, this often looks like a well-dressed middle-aged or older man with an expensive haircut calling for a young confident-looking aide in a lab coat to administer the medicine, and is received better than a slightly frazzled academic saying “and, uh, this one’s yours” while handing you a pill.
- Things with ritual attached: this can be related to the above (the more pomp and circumstance is given to the administration of the treatment, the better), but it can also be as simple as an instruction on an at-home-trial medication saying “take 20 minutes before bed”. Because, if it weren’t important, they wouldn’t bother to specify that, right? So it must be important!
And now for a quick personality test
Did you see the above as a list of dastardly tricks to watch out for, or did you see the above as a list of things that can make your actual medication more effective?
It’s arguably both, of course, but the latter more optimistic view is a lot more useful than the former more pessimistic one.
Since placebo effect works at least somewhat even when you know about it, there is nothing to stop you from leveraging it for your own benefit when taking medication or doing health-related things.
Next time you take your meds or supplements or similar, pause for a moment for each one to remember what it is and what it will be doing for you. This is a lot like the principles (which are physiological as well as psychological) of mindful eating, by the way:
How To Get More Nutrition From The Same Food
Placebo makes some surprising things evidence-based
We’ve addressed placebo effect sometimes as part of an assessment of a given alternative therapy, often in our “Mythbusting Friday” edition of 10almonds.
- In some cases, placebo is adjuvant to the therapy, i.e. it is one of multiple mechanisms of action (example: chiropractic or acupuncture)
- In some cases, placebo is the only known mechanism of action (example: homeopathy)
- In some cases, even placebo can’t help (example: ear candling)
One other fascinating and far-reaching (in a potentially good way) thing that placebo makes evidence-based is: prayer
…which is particularly interesting for something that is fundamentally faith-based, i.e. the opposite of evidence-based.
Now, we’re a health science publication, not a theological publication, so we’ll consider actual divine intervention to be beyond the scope of mechanisms of action we can examine, but there’s been a lot of research done into the extent to which prayer is beneficial as a therapy, what things it may be beneficial for, and what factors affect whether it helps:
Prayer and healing: A medical and scientific perspective on randomized controlled trials
👆 full paper here, and it is very worthwhile reading if you have time, whether or not you are religious personally
Placebo works best when there’s a clear possibility for psychosomatic effect
We’ve mentioned before, and we’ll mention again:
- psychosomatic effect does not mean: “imagining it”
- psychosomatic effect means: “your brain regulates almost everything else in your body, directly or indirectly, including your autonomic functions, and especially notably when it comes to illness, your immune responses”
So, a placebo might well heal your rash or even shrink a tumor, but it probably won’t regrow a missing limb, for instance.
And, this is important: it’s not about how credible/miraculous the outcome will be!
Rather, it is because we have existing pre-programmed internal bodily processes for healing rashes and shrinking tumors, that just need to be activated—whereas we don’t have existing pre-programmed internal bodily processes for regrowing a missing limb, so that’s not something our brain can just tell our body to do.
So for this reason, in terms of what placebo can and can’t do:
- Get rid of cancer? Yes, sometimes—because the body has a process for doing that; enjoy your remission
- Fix a broken nail? No—because the body has no process for doing that; you’ll just have to cut it and wait for it to grow again
With that in mind, what will you use the not-so-mystical powers of placebo for? What ever you go for… Enjoy, and take care!
Share This Post
-
100,000 People, 30 Years, One Clear Winner vs Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Generally speaking, the scientific community most highly lauds the Mediterranean diet as being best for general health:
The Mediterranean Diet: What Is It Good For? ← what isn’t it good for?!
However, even this can be tweaked with specific health considerations in mind, for example:
Four Ways To Upgrade The Mediterranean Diet ← these tweaks offer adjusted versions of the Mediterranean diet, optimized for anti-inflammation, gut health, heart health, or brain health
And today we present to you some very good research into…
The best diet for aging well
Let’s be clear on terms first: by “aging well”, this means reaching age 70 without chronic diseases and maintaining good cognitive, physical, and mental health.
105,015 participants (of whom, 66% women, average age 53 at the start of the study) were followed for up to 30 years. Not in the stalkery way, but in the longitudinal study way. We say “up to”, because as with any sizeable longitudinal study, some died before the end of the study.
9,771 of them were deemed, at the end of the study, to have achieved “healthy aging”.
So, how did those participants achieve that, in terms of diet?
The dietary patterns that had the strongest positive impact were:
- AHEI (Alternative Healthy Eating Index): best for mental and physical function, overall healthy aging.
- PHDI (Planetary Health Diet Index): best for cognitive health and survival to age 70.
- DASH (Dietary Approaches to Stop Hypertension): strongest general impact.
- MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay): best for brain health.
- rEDIH (Reversed Empirical Dietary Index for Hyperinsulinemia): most effective for chronic disease prevention.
In contrast:
- EIDP (Empirically Inflammatory Dietary Pattern): shocking nobody, performed least well in all areas
You are probably wondering what those dietary patterns actually consist of, so click here to see a chart of what’s included or excluded in each dietary pattern.
As you can see, the AHEI diet that was “best for mental and physical function, overall healthy aging” is essentially the Mediterranean diet with three small tweaks:
- no seafood, but long-chain omega-3 fatty acids include to compensate
- no sugar-sweetened beverages or fruit juices
- “no” sodium (in other words, minimal sodium, since almost everything contains trace amounts)
The PHDI diet, which was “best for cognitive health and survival to age 70” is essentially a whole-foods plant-based diet. Which in turn is very consistent with the Mediterranean, except that it excludes animal products, of which the Mediterranean diet uses small amounts.
You can read the paper in its entirety here:
Optimal dietary patterns for healthy aging
Want to know more?
A panel of 69 doctors and nutritionists examined the evidence for 38 diets (including Mediterranean, MIND, DASH, Vegan, Keto, Slimfast, WeightWatchers, Nutrisystem, and more) and scored them in 21 categories (e.g. best for general health, best for weight loss, best for heart, best against diabetes, etc):
Which Diet? Top Diets Ranked By Experts
Enjoy!
Share This Post
Related Posts
-
Cognitive Enhancement Without Drugs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cognitive Enhancement Without Drugs
This is Elizabeth Ricker. She’s a Harvard-and-MIT-trained neuroscientist and researcher, who now runs the “Citizen Science” DIY-neurohacking organization, NeuroEducate.
Sounds fun! What’s it about?
The philosophy that spurs on her research and practice can be summed up as follows:
❝I’m not going to leave my brain up to my doctor or [anyone else]… My brain is my own responsibility, and I’m going to do the best that I can to optimize it❞
Her goal is not just to optimize her own brain though; she wants to make the science accessible to everyone.
What’s this about Citizen Science?
“Citizen Science” is the idea that while there’s definitely an important role in society for career academics, science itself should be accessible to all. And, not just the conclusions, but the process too.
This can take the form of huge experiments, often facilitated these days by apps where we opt-in to allow our health metrics (for example) to be collated with many thousands of others, for science. It can also involve such things as we talked about recently, getting our own raw genetic data and “running the numbers” at home to get far more comprehensive and direct information than the genetic testing company would ever provide us.
For Ricker, her focus is on the neuroscience side of biohacking, thus, neurohacking.
I’m ready to hack my brain! Do I need a drill?
Happily not! Although… Bone drills for the skull are very convenient instruments that make it quite hard to go wrong even with minimal training. The drill bit has a little step/ledge partway down, which means you can only drill through the thickness of the skull itself, before the bone meeting the wider part of the bit stops you from accidentally drilling into the brain. Still, please don’t do this at home.
What you can do at home is a different kind of self-experimentation…
If you want to consider which things are genuinely resulting in cognitive enhancement and which things are not, you need to approach the matter like a scientist. That means going about it in an organized fashion, and recording results.
There are several ways cognitive enhancement can be measured, including:
- Learning and memory
- Executive function
- Emotional regulation
- Creative intelligence
Let’s look at each of them, and what can be done. We don’t have a lot of room here; we’re a newsletter not a book, but we’ll cover one of Ricker’s approaches for each:
Learning and memory
This one’s easy. We’re going to leverage neuroplasticity (neurons that fire together, wire together!) by simple practice, and introduce an extra element to go alongside your recall. Perhaps a scent, or a certain item of clothing. Tell yourself that clinical studies have shown that this will boost your recall. It’s true, but that’s not what’s important; what’s important is that you believe it, and bring the placebo effect to bear on your endeavors.
You can test your memory with word lists, generated randomly by AI, such as this one:
You’ll soon find your memory improving—but don’t take our word for it!
Executive function
Executive function is the aspect of your brain that tells the other parts how to work, when to work, and when to stop working. If you’ve ever spent 30 minutes thinking “I need to get up” but you were stuck in scrolling social media, that was executive dysfunction.
This can be trained using the Stroop Color and Word Test, which shows you words, specifically the names of colors, which will themselves be colored, but not necessarily in the color the word pertains to. So for example, you might be shown the word “red”, colored green. Your task is to declare either the color of the word only, ignoring the word itself, or the meaning of the word only, ignoring its appearance. It can be quite challenging, but you’ll get better quite quickly:
The Stroop Test: Online Version
Emotional Regulation
This is the ability to not blow up angrily at the person with whom you need to be diplomatic, or to refrain from laughing when you thought of something funny in a sombre situation.
It’s an important part of cognitive function, and success or failure can have quite far-reaching consequences in life. And, it can be trained too.
There’s no online widget for this one, but: when and if you’re in a position to safely* do so, think about something that normally triggers a strong unwanted emotional reaction. It doesn’t have to be something life-shattering, but just something that you feel in some way bad about. Hold this in your mind, sit with it, and practice mindfulness. The idea is to be able to hold the unpleasant idea in your mind, without becoming reactive to it, or escaping to more pleasant distractions. Build this up.
*if you perchance have PTSD, C-PTSD, or an emotional regulation disorder, you might want to talk this one through with a qualified professional first.
Creative Intelligence
Another important cognitive skill, and again, one that can be cultivated and grown.
The trick here is volume. A good, repeatable test is to think of a common object (e.g. a rock, a towel, a banana) and, within a time constraint (such as 15 minutes) list how many uses you can think of for that item.
Writer’s storytime: once upon a time, I was sorting through an inventory of medical equipment with a colleague, and suggested throwing out our old arterial clamps, as we had newer, better ones—in abundance. My colleague didn’t want to part with them, so I challenged him “Give me one use for these, something we could in some possible world use them for that the new clamps don’t do better, and we’ll keep them”. He said “Thumbscrews”, and I threw my hands up in defeat, saying “Fine!”, as he had technically fulfilled my condition.
What’s the hack to improve this one? Just more volume. Creativity, as it turns out, isn’t something we can expend—like a muscle, it grows the more we use it. And because the above test is repeatable (with different objects), you can track your progress.
And if you feel like using your grown creative muscle to write/paint/compose/etc your magnum opus, great! Or if you just want to apply it to the problem-solving of everyday life, also great!
In summary…
Our brain is a wonderful organ with many functions. Society expects us to lose these as we get older, but the simple, scientific truth is that we can not only maintain our cognitive function, but also enhance and grow it as we go.
Want to know more from today’s featured expert?
You might enjoy her book, “Smarter Tomorrow”, which we reviewed back in March
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Wondering how to spot the signs of postpartum depression?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Postpartum depression, or PPD, is a debilitating, potentially life-threatening mental health condition that impacts about one in eight people who give birth in the U.S. While it’s normal to feel worried or stressed after becoming a parent, PPD can cause feelings of extreme sadness or anxiety that may lead to suicidal thoughts.
Read on to learn what PPD is, what causes it, how it’s treated, and more.
What is the difference between the baby blues and postpartum depression?
Postpartum blues, or the “baby blues,” impact up to 80 percent of new parents. The baby blues may cause bouts of crying, mood swings, anxiety, sadness, reduced concentration, irritability, changes in appetite, and trouble sleeping, but symptoms are fleeting.
“Baby blues are a transient period—hours to a few days—of emotionality that does not impair one’s functioning or cause severe symptoms like suicidality,” says Dr. Jennifer L. Payne, a professor of psychiatry and neurobehavioral sciences at the University of Virginia. “[Postpartum depression] can cause severe symptoms, including suicidality.”
In addition to causing more debilitating symptoms, PPD can last for months.
Some new parents also experience postpartum psychosis, which can cause hallucinations and delusions. However, unlike PPD, postpartum psychosis is rare.
What are the symptoms of postpartum depression?
PPD symptoms may include:
- Feeling depressed, irritable, angry, or hopeless
- Severe mood swings
- Difficulty bonding with your baby
- Withdrawing from family and friends
- Changes in appetite or sleeping patterns
- Extreme fatigue
- Difficulty concentrating
- Anxiety and panic attacks
- Thoughts of harming yourself or your baby
- Thoughts of death or suicide
If you are experiencing symptoms of PPD, Payne recommends seeking help from a primary care provider or obstetrician right away.
“It’s really important—not just for you, but for your baby,” Payne explains. “Babies exposed to significant PPD have slower language development, lower IQs, and more behavioral problems.”
Your health care provider will ask you a series of screening questions to determine if you are experiencing PPD.
What causes postpartum depression?
Research suggests that the drop in hormones that occurs after birth, genetics, and sleep deprivation may contribute to PPD.
You may be at higher risk of developing PPD if you have a history of mental health conditions like depression or bipolar disorder, have relatives who’ve experienced PPD, or experienced stressful events during or after pregnancy.
How is postpartum depression treated?
“PPD is usually treated with antidepressant medications—typically SSRIs and now with the new FDA-approved medication, zuranolone,” says Payne. Therapy has also been shown to help people manage PPD.
Your health care provider can help determine the best treatment options for you and can outline the risks and benefits of taking certain medications while breastfeeding.
For referrals to care, information about local support groups, and other mental health resources for new parents, call the National Maternal Mental Health Hotline or Postpartum Support International. If you are experiencing a mental health emergency, call or text the 988 Suicide & Crisis Lifeline.
Can non-birthing parents have postpartum depression?
New parents who did not give birth, including cisgender men, may experience anxiety, depression, irritability, fatigue, and changes in appetite or sleeping patterns after a partner gives birth.
“Everyone knows that mothers’ hormones change a lot during and after pregnancy,” psychologist Scott Bea said in a 2019 Cleveland Clinic article. “But there’s evidence that fathers also experience real changes in their hormone levels after a baby is born.”
Adoptive parents may also show similar symptoms.
If you or anyone you know is considering suicide or self-harm or is anxious, depressed, upset, or needs to talk, call the Suicide & Crisis Lifeline at 988 or text the Crisis Text Line at 741-741. For international resources, here is a good place to begin.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Codependency Isn’t What Most People Think It Is
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Codependency isn’t what most people think it is
In popular parlance, people are often described as “codependent” when they rely on each other to function normally. That’s interdependent mutualism, and while it too can become a problem if a person is deprived of their “other half” and has no idea how to do laundry and does not remember to take their meds, it’s not codependency.
Codependency finds its origins in the treatment and management of alcoholism, and has been expanded to encompass other forms of relationships with dependence on substances and/or self-destructive behaviors—which can be many things, including the non-physical, for example a pattern of irresponsible impulse-spending, or sabotaging one’s own relationship(s).
We’ll use the simplest example, though:
- Person A is (for example) an alcoholic. They have a dependency.
- Person B, married to A, is not an alcoholic. However, their spouse’s dependency affects them greatly, and they do what they can to manage that, and experience tension between wanting to “save” their spouse, and wanting their spouse to be ok, which latter, superficially, often means them having their alcohol.
Person B is thus said to be “codependent”.
The problem with codependency
The problems of codependency are mainly twofold:
- The dependent partner’s dependency is enabled and thus perpetuated by the codependent partner—they might actually have to address their dependency, if it weren’t for their partner keeping them from too great a harm (be it financially, socially, psychologically, medically, whatever)
- The codependent partner is not having a good time of it either. They have the stress of two lives with the resources (e.g. time) of one. They are stressing about something they cannot control, understandably worrying about their loved one, and, worse: every action they might take to “save” their loved one by reducing the substance use, is an action that makes their partner unhappy, and causes conflict too.
Note: codependency is often a thing in romantic relationships, but it can appear in other relationships too, e.g. parent-child, or even between friends.
See also: Development and validation of a revised measure of codependency
How to deal with this
If you find yourself in a codependent position, or are advising someone who is, there are some key things that can help:
- Be a nurturer, not a rescuer. It is natural to want to “rescue” someone we care about, but there are some things we cannot do for them. Instead, we must look for ways to build their strength so that they can take the steps that only they can take to fix the problem.
- Establish boundaries. Practise saying “no”, and also be clear over what things you can and cannot control—and let go of the latter. Communicate this, though. An “I’m not the boss of you” angle can prompt a lot of people to take more personal responsibility.
- Schedule time for yourself. You might take some ideas from our previous tangentially-related article:
How To Avoid Carer Burnout (Without Dropping Care)
Want to read more?
That’s all we have space for today, but here’s a very useful page with a lot of great resources (including questionnaires and checklist and things, in case you’re thinking “is it, or…?”)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: