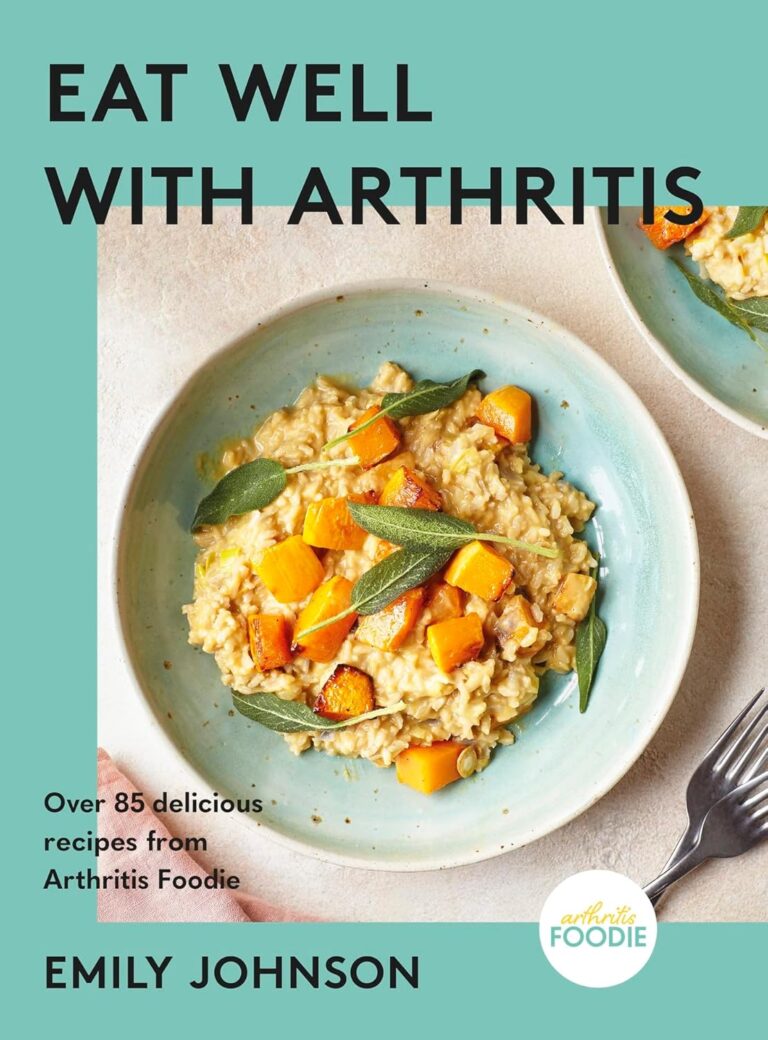
Eat More, Live Well – by Dr. Megan Rossi
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Often, eating healthily can feel restrictive. Don’t eat this, skip that, eliminate the other. Where is the joy?
Dr. Megan Rossi brings a scientific angle on positive dieting, that is to say, looking at what to add, rather than what to subtract. Now, the idea isn’t to have sugar-laden chocolate cake with berries on top and call it a net positive because of the berries, though. Rather, Dr. Rossi lays out how to include as many diverse vegetables and fruits as possible, with tasty recipes so that we’re too busy with those to crave junk food.
Speaking of recipes, there are 80, and they are easy to follow. She describes them as “plant-based”, and by this what she really means is “plant-centric” or such; she does include the use of some animal products.
This is important to note, because general convention is to use “plant-based” to mean functionally vegan, but being about the food rather than the ideology; a relevant distinction in both society and science. In the case of this book, it’s neither, but it is very healthy.
Bottom line: if you’d like to introduce more healthy diversity to your diet, rather than eating the same three fruits and five vegetables, but you’re not sure how, this book will get you where you need to be.
Click here to check out Eat More, Live Well, and diversify your diet!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
War in Ukraine affected wellbeing worldwide, but people’s speed of recovery depended on their personality
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The war in Ukraine has had impacts around the world. Supply chains have been disrupted, the cost of living has soared and we’ve seen the fastest-growing refugee crisis since World War II. All of these are in addition to the devastating humanitarian and economic impacts within Ukraine.
Our international team was conducting a global study on wellbeing in the lead up to and after the Russian invasion. This provided a unique opportunity to examine the psychological impact of the outbreak of war.
As we explain in a new study published in Nature Communications, we learned the toll on people’s wellbeing was evident across nations, not just in Ukraine. These effects appear to have been temporary – at least for the average person.
But people with certain psychological vulnerabilities struggled to recover from the shock of the war.
Tracking wellbeing during the outbreak of war
People who took part in our study completed a rigorous “experience-sampling” protocol. Specifically, we asked them to report their momentary wellbeing four times per day for a whole month.
Data collection began in October 2021 and continued throughout 2022. So we had been tracking wellbeing around the world during the weeks surrounding the outbreak of war in February 2022.
We also collected measures of personality, along with various sociodemographic variables (including age, gender, political views). This enabled us to assess whether different people responded differently to the crisis. We could also compare these effects across countries.
Our analyses focused primarily on 1,341 participants living in 17 European countries, excluding Ukraine itself (44,894 experience-sampling reports in total). We also expanded these analyses to capture the experiences of 1,735 people living in 43 countries around the world (54,851 experience-sampling reports) – including in Australia.
A global dip in wellbeing
On February 24 2022, the day Russia invaded Ukraine, there was a sharp decline in wellbeing around the world. There was no decline in the month leading up to the outbreak of war, suggesting the change in wellbeing was not already occurring for some other reason.
However, there was a gradual increase in wellbeing during the month after the Russian invasion, suggestive of a “return to baseline” effect. Such effects are commonly reported in psychological research: situations and events that impact our wellbeing often (though not always) do so temporarily.
Unsurprisingly, people in Europe experienced a sharper dip in wellbeing compared to people living elsewhere around the world. Presumably the war was much more salient for those closest to the conflict, compared to those living on an entirely different continent.
Interestingly, day-to-day fluctuations in wellbeing mirrored the salience of the war on social media as events unfolded. Specifically, wellbeing was lower on days when there were more tweets mentioning Ukraine on Twitter/X.
Our results indicate that, on average, it took around two months for people to return to their baseline levels of wellbeing after the invasion.
Different people, different recoveries
There are strong links between our wellbeing and our individual personalities.
However, the dip in wellbeing following the Russian invasion was fairly uniform across individuals. None of the individual factors assessed in our study, including personality and sociodemographic factors, predicted people’s response to the outbreak of war.
On the other hand, personality did play a role in how quickly people recovered. Individual differences in people’s recovery were linked to a personality trait called “stability”. Stability is a broad dimension of personality that combines low neuroticism with high agreeableness and conscientiousness (three traits from the Big Five personality framework).
Stability is so named because it reflects the stability of one’s overall psychological functioning. This can be illustrated by breaking stability down into its three components:
- low neuroticism describes emotional stability. People low in this trait experience less intense negative emotions such as anxiety, fear or anger, in response to negative events
- high agreeableness describes social stability. People high in this trait are generally more cooperative, kind, and motivated to maintain social harmony
- high conscientiousness describes motivational stability. People high in this trait show more effective patterns of goal-directed self-regulation.
So, our data show that people with less stable personalities fared worse in terms of recovering from the impact the war in Ukraine had on wellbeing.
In a supplementary analysis, we found the effect of stability was driven specifically by neuroticism and agreeableness. The fact that people higher in neuroticism recovered more slowly accords with a wealth of research linking this trait with coping difficulties and poor mental health.
These effects of personality on recovery were stronger than those of sociodemographic factors, such as age, gender or political views, which were not statistically significant.
Overall, our findings suggest that people with certain psychological vulnerabilities will often struggle to recover from the shock of global events such as the outbreak of war in Ukraine.
Luke Smillie, Professor in Personality Psychology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Are your Kidneys Ok? Detect Early To Protect Kidney Health (Here’s How)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tomorrow (at time of publication) will be World Kidney Day (WKD). Perhaps not the most well-known initiative, but it celebrates its 21st year this year!
For those of us who celebrated our own 21st year quite some time ago now, it’s as good a reason as any to check in on our kidney health.
Here are some things they’d like us to know about Chronic Kidney Disease (CKD):
❝CKD is a silent disease, people with CKD have no signs or symptoms until the late stage of the disease.
CKD usually does not go away, instead, it progresses, unless early treatment to slow or halt the disease is ensured.
CKD can progress to kidney failure – a condition when kidneys cannot maintain their function anymore, posing a life-threatening risk.
CKD ranks number 7 in the top ten causes of death among noncommunicable diseases worldwide.
CKD increases the risk of premature death from associated cardiovascular disease.
CKD is more common among certain ethnic groups due in part to high rates of diabetes and high blood pressure.
CKD is more common among women, here is why.❞Source: World Kidney Day: Your Amazing Kidneys
How can we check our kidney health?
There are clinical tests that can be done (they’ll just need a urine sample from you; ask your doctor about it), but there’s some screening that can be done at home already:
Are Your Kidneys Healthy? Take This One-Minute Quiz To Find out
👆 this is about medical indicators; there are also non-medical factors that affect risk, including:
- Where someone lives
- Where they work
- The foods they eat
- How much exercise they do
- If they are able to get the medical care they need
For more information on this, see: Keeping Your Kidneys Healthy (Especially After 60) ← there’s a lot more to it than just hydration!
What can we do for our kidney health, besides the obvious “hydrate”?
Some top things to do include:
Hydrate, yes. See also: Things Many People Forget When It Comes To Hydration
Don’t smoke. It’s bad for everything, including your kidneys. So, just don’t. See also: Addiction Myths That Are Hard To Quit
Look after your blood. Not just “try to keep it inside your body”, but also:
- Keep your blood sugar levels healthy (hyperglycemia can cause kidney damage)
- Keep your blood pressure healthy (hypertension can cause kidney damage)
Basically, your kidneys’ primary job of filtering blood will go much more smoothly if that blood is less problematic on the way in.
Watch your over-the-counter pill intake. A lot of PRN OTC NSAIDs (PRN = pro re nata, i.e. you take them as and when symptoms arise) (NSAIDs = Non-Steroidal Anti-Inflammatory Drugs, such as ibuprofen for example) can cause kidney damage if taken regularly.
Keep an eye on your urine. Hydration is only one side of the story, and our urine can say quite a bit about our health. Indeed, we have written about this before:
12 Things Your Urine Says About Your Health (Test At Home) ← no special equipment required!
On which note, see also: To Pee Or Not To Pee ← spoiler: there’s a flood of reasons to not hold your pee
Want to know more?
Check out the WKD website’s…
8 Golden Rules Of Kidney Disease Prevention
Take care!
Share This Post
-
Anti-Inflammatory Diet 101 (What to Eat to Fight Inflammation)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chronic inflammation is a cause and/or exacerbating factor in very many diseases. Arthritis, diabetes, and heart disease are probably top of the list, but there are lots more where they came from. And, it’s good to avoid those things. So, how to eat to avoid inflammation?
Let food be thy medicine
The key things to keep in mind, the “guiding principles” are to prioritize whole, minimally-processed foods, and enjoy foods with plenty of antioxidants. Getting a healthy balance of omega fatty acids is also important, which for most people means getting more omega-3 and less omega-6.
Shopping list (foods to prioritize) includes:
- fruits and vegetables in a variety of colors (e.g. berries, leafy greens, beats)
- whole grains, going for the most fiber-rich options (e.g. quinoa, brown rice, oats)
- healthy fats (e.g. avocados, nuts, seeds)
- fatty fish (e.g. salmon, mackerel, sardines) ← don’t worry about this if you’re vegetarian/vegan though, as the previous category can already cover it
- herbs and spices (e.g. turmeric, garlic, ginger)
Noping list (foods to avoid) includes:
- refined carbohydrates
- highly processed and/or fried foods
- red meats and/or processed meats (yes, that does mean that organic grass-fed farmers’ pinky-promise-certified holistically-raised beef is also off the menu)
- dairy products, especially if unfermented
For more information on each of these, plus advice on transitioning away from an inflammatory diet, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How to Prevent (or Reduce) Inflammation
Take care!
Share This Post
Related Posts
-
Tastes from our past can spark memories, trigger pain or boost wellbeing. Here’s how to embrace food nostalgia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever tried to bring back fond memories by eating or drinking something unique to that time and place?
It could be a Pina Colada that recalls an island holiday? Or a steaming bowl of pho just like the one you had in Vietnam? Perhaps eating a favourite dish reminds you of a lost loved one – like the sticky date pudding Nanna used to make?
If you have, you have tapped into food-evoked nostalgia.
As researchers, we are exploring how eating and drinking certain things from your past may be important for your mood and mental health.
Halfpoint/Shutterstock Bittersweet longing
First named in 1688 by Swiss medical student, Johannes Hoffer, nostalgia is that bittersweet, sentimental longing for the past. It is experienced universally across different cultures and lifespans from childhood into older age.
But nostalgia does not just involve positive or happy memories – we can also experience nostalgia for sad and unhappy moments in our lives.
In the short and long term, nostalgia can positively impact our health by improving mood and wellbeing, fostering social connection and increasing quality of life. It can also trigger feelings of loneliness or meaninglessness.
We can use nostalgia to turn around a negative mood or enhance our sense of self, meaning and positivity.
Research suggests nostalgia alters activity in the brain regions associated with reward processing – the same areas involved when we seek and receive things we like. This could explain the positive feelings it can bring.
Nostalgia can also increase feelings of loneliness and sadness, particularly if the memories highlight dissatisfaction, grieving, loss, or wistful feelings for the past. This is likely due to activation of brain areas such as the amygdala, responsible for processing emotions and the prefrontal cortex that helps us integrate feelings and memories and regulate emotion.
How to get back there
There are several ways we can trigger or tap into nostalgia.
Conversations with family and friends who have shared experiences, unique objects like photos, and smells can transport us back to old times or places. So can a favourite song or old TV show, reunions with former classmates, even social media posts and anniversaries.
What we eat and drink can trigger food-evoked nostalgia. For instance, when we think of something as “comfort food”, there are likely elements of nostalgia at play.
Foods you found comforting as a child can evoke memories of being cared for and nurtured by loved ones. The form of these foods and the stories we tell about them may have been handed down through generations.
Food-evoked nostalgia can be very powerful because it engages multiple senses: taste, smell, texture, sight and sound. The sense of smell is closely linked to the limbic system in the brain responsible for emotion and memory making food-related memories particularly vivid and emotionally charged.
But, food-evoked nostalgia can also give rise to negative memories, such as of being forced to eat a certain vegetable you disliked as a child, or a food eaten during a sad moment like a loved ones funeral. Understanding why these foods evoke negative memories could help us process and overcome some of our adult food aversions. Encountering these foods in a positive light may help us reframe the memory associated with them.
Just like mum used to make. Food might remind you of the special care you received as a child. Galina Kovalenko/Shutterstock What people told us about food and nostalgia
Recently we interviewed eight Australians and asked them about their experiences with food-evoked nostalgia and the influence on their mood. We wanted to find out whether they experienced food-evoked nostalgia and if so, what foods triggered pleasant and unpleasant memories and feelings for them.
They reported they could use foods that were linked to times in their past to manipulate and influence their mood. Common foods they described as particularly nostalgia triggering were homemade meals, foods from school camp, cultural and ethnic foods, childhood favourites, comfort foods, special treats and snacks they were allowed as children, and holiday or celebration foods. One participant commented:
I guess part of this nostalgia is maybe […] The healing qualities that food has in mental wellbeing. I think food heals for us.
Another explained
I feel really happy, and I guess fortunate to have these kinds of foods that I can turn to, and they have these memories, and I love the feeling of nostalgia and reminiscing and things that remind me of good times.
Yorkshire pudding? Don’t mind if I do. Rigsbyphoto/Shutterstock Understanding food-evoked nostalgia is valuable because it provides us with an insight into how our sensory experiences and emotions intertwine with our memories and identity. While we know a lot about how food triggers nostalgic memories, there is still much to learn about the specific brain areas involved and the differences in food-evoked nostalgia in different cultures.
In the future we may be able to use the science behind food-evoked nostalgia to help people experiencing dementia to tap into lost memories or in psychological therapy to help people reframe negative experiences.
So, if you are ever feeling a little down and want to improve your mood, consider turning to one of your favourite comfort foods that remind you of home, your loved ones or a holiday long ago. Transporting yourself back to those times could help turn things around.
Megan Lee, Senior Teaching Fellow, Psychology, Bond University; Doug Angus, Assistant Professor of Psychology, Bond University, and Kate Simpson, Sessional academic, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
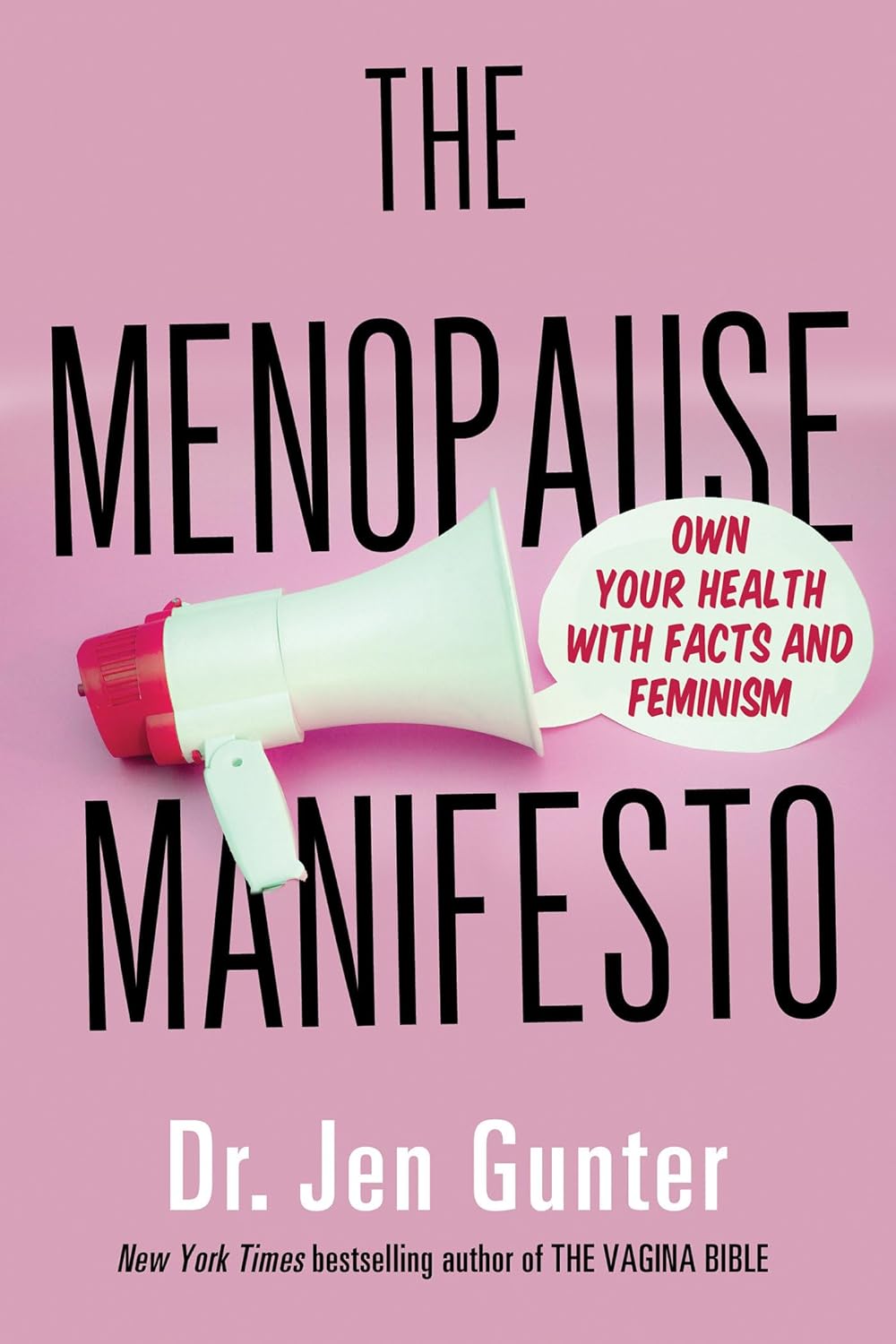
The Menopause Manifesto – by Dr. Jen Gunter
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From the subtitle, you may wonder: with facts and feminism? Is this book about biology or sociology?
And the answer is: both. It’s about biology, principally, but without ignoring the context. We do indeed “live in a society”, and that affects everything from our healthcare options to what is expected of us as women.
So, as a warning: if you dislike science and/or feminism, you won’t like this book.
Dr. Jen Gunter, herself a gynaecologist, is here to arm us with science-based facts, to demystify an important part of life that is commonly glossed over.
She talks first about the what/why/when/how of menopause, and then delivers practical advice. She also talks about the many things we can (and can’t!) usefully do about symptoms we might not want, and how to look after our health overall in the context of menopause. We learn what natural remedies do or don’t work and/or can be actively harmful, and we learn the ins and outs of different hormone therapy options too.
Bottom line: no matter whether you are pre-, peri-, or post-menopausal, this is the no-BS guide you’ve been looking for. Same goes if you’re none of the above but spend any amount of time close to someone who is.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Procrastination, and how to pay off the to-do list debt
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Procrastination, and how pay off the to-do list debt
Sometimes we procrastinate because we feel overwhelmed by the mountain of things we are supposed to be doing. If you look at your to-do list and it shows 60 overdue items, it’s little wonder if you want to bury your head in the sand!
“What difference does it make if I do one of these things now; I will still have 59 which feels as bad as having 60”
So, treat it like you might a financial debt, and make a repayment plan. Now, instead of 60 overdue items today, you have 1/day for the next 60 days, or 2/day for the next 30 days, or 3/day for the next 20 days, etc. Obviously, you may need to work out whether some are greater temporal priorities and if so, bump those to the top of the list. But don’t sweat the minutiae; your list doesn’t have to be perfectly ordered, just broadly have more urgent things to the top and less urgent things to the bottom.
Note: this repayment plan means having set repayment dates.
Up front, sit down and assign each item a specific calendar date on which you will do that thing.
This is not a deadline! It is your schedule. You’ll not try to do it sooner, and you won’t postpone it for later. You will just do that item on that date.
A productivity app like ToDoist can help with this, but paper is fine too.
What’s important here, psychologically, is that each day you’re looking not at 60 things and doing the top item; you’re just looking at today’s item (only!) and doing it.
Debt Reduction/Cancellation
Much like you might manage a financial debt, you can also look to see if any of your debts could be reduced or cancelled.
We wrote previously about the “Getting Things Done” system. It’s a very good system if you want to do that; if not, no worries, but you might at least want to borrow this one idea….
Sort your items into:
Do / Defer / Delegate / Ditch
- Do: if it can be done in under 2 minutes, do it now.
- Defer: defer the item to a specific calendar date (per the repayment plan idea we just talked about)
- Delegate: could this item be done by someone else? Get it off your plate if you reasonably can.
- Ditch: sometimes, it’s ok to realize “you know what, this isn’t that important to me anymore” and scratch it from the list.
As a last resort, consider declaring bankruptcy
Towards the end of the dot-com boom, there was a fellow who unintentionally got his 5 minutes of viral fame for “declaring email bankruptcy”.
Basically, he publicly declared that his email backlog had got so far out of hand that he would now not reply to emails from before the declaration.
He pledged to keep on top of new emails only from that point onwards; a fresh start.
We can’t comment on whether he then did, but if you need a fresh start, that can be one way to get it!
In closing…
Procrastination is not usually a matter of laziness, it’s usually a matter of overwhelm. Hopefully the above approach will help reframe things, and make things more manageable.
Sometimes procrastination is a matter of perfectionism, and not starting on tasks because we worry we won’t do them well enough, and so we get stuck in a pseudo-preparation rut. If that’s the case, our previous main feature on perfectionism may help:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: