Alzheimer’s Causative Factors To Avoid
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Best Brains Bar Nun?
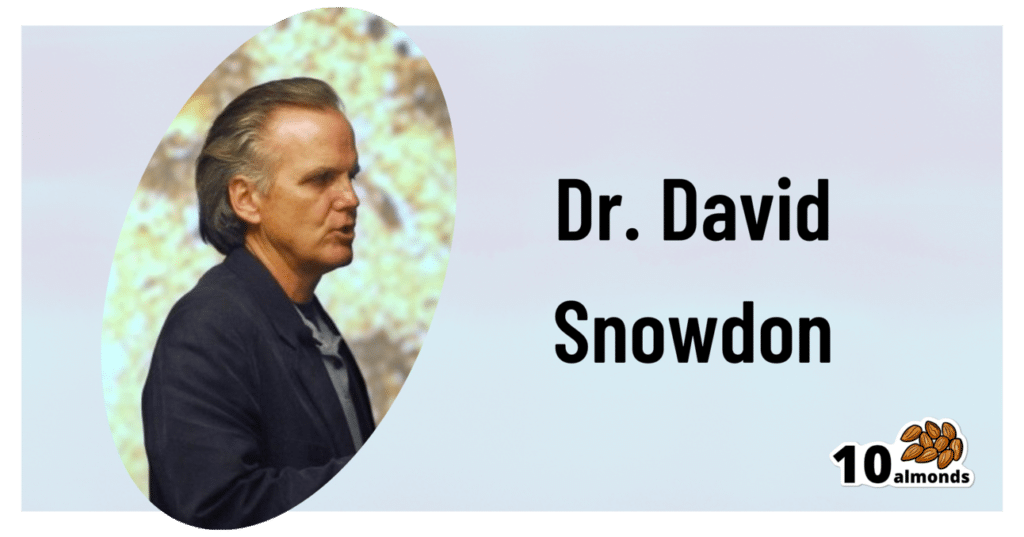
This is Dr. David Snowdon. He’s an epidemiologist, and one of the world’s foremost experts on Alzheimer’s disease. He was also, most famously, the lead researcher of what has become known as “The Nun Study”.
We recently reviewed his book about this study:
…which we definitely encourage you to check out, but we’ll do our best to summarize its key points today!
Reassurance up-front: no, you don’t have to become a nun
The Nun Study
In 1991, a large number (678) of nuns were recruited for what was to be (and until now, remains) the largest study of its kind into the impact of a wide variety of factors on aging, and in particular, Alzheimer’s disease.
Why it was so important: because the nuns were all from the same Order, had the same occupation (it’s a teaching Order), with very similar lifestyles, schedules, socioeconomic status, general background, access to healthcare, similar diets, same relationship status (celibate), same sex (female), and many other factors also similar, this meant that most of the confounding variables that confound other studies were already controlled-for here.
Enrollment in the study also required consenting to donating one’s brain for study post-mortem—and of those who have since died, indeed 98% of them have been donated (the other 2%, we presume, may have run into technical administrative issues with the donation process, due to the circumstances of death and/or delays in processing the donation).
How the study was undertaken
We don’t have enough space to describe the entire methodology here, but the gist of it is:
- Genetic testing for relevant genetic factors
- Data gathered about lives so far, including not just medical records but also autobiographies that the nuns wrote when they took their vows (at ages 19–21)
- Extensive ongoing personal interviews about habits, life choices, and attitudes
- Yearly evaluations including memory tests and physical function tests
- Brain donation upon death
What they found
Technically, The Nun Study is still ongoing. Of the original 678 nuns (aged 75–106), three are still alive (based on the latest report, at least).
However, lots of results have already been gained, including…
Genes
A year into the study, in 1992, the “apolipoprotein E” (APOE) gene was established as a likely causative factor in Alzheimer’s disease. This is probably not new to our readers in 2024, but there are interesting things being learned even now, for example:
The Alzheimer’s Gene That Varies By Race & Sex
…but watch out! Because also:
Alzheimer’s Sex Differences May Not Be What They Appear
Words
Based on the autobiographies written by the nuns in their youth upon taking their vows, there were two factors that were later correlated with not getting dementia:
- Longer sentences
- Positive outlook
- “Idea density”
That latter item means the relative linguistic density of ideas and complexity thereof, and the fluency and vivacity with which they were expressed (this was not a wishy-washy assessment; there was a hard-science analysis to determine numbers).
Want to spruce up yours? You might like to check out:
Reading, Better: Reading As A Cognitive Exercise
…for specific, evidence-based ways to tweak your reading to fight cognitive decline.
Food
While the dietary habits of the nuns were fairly homogenous, those who favored eating more and cooked greens, beans, and tomatoes, lived longer and with healthier brains.
See also: Brain Food? The Eyes Have It!
Other aspects of brain health & mental health
The study also found that nuns who avoided stroke and depression, were also less likely to get dementia.
For tending to these, check out:
- Two Things You Can Do To Improve Stroke Survival Chances
- Depression, And The Mental Health First-Aid That You’ll Hopefully Never Need
- Behavioral Activation Against Depression & Anxiety
Community & Faith
Obviously, in this matter the nuns were quite a homogenous group, scoring heavily in community and faith. What’s relevant here is the difference between the nuns, and other epidemiological studies in other groups (invariably not scoring so highly).
Community & faith are considered, separately and together, to be protective factors against dementia.
Faith may be something that “you have it or you don’t” (we’re a health science newsletter, not a theological publication, but for the interested, philosopher John Stuart Mill’s 1859 essay “On Liberty“ makes a good argument for it not being something one can choose, prompting him to argue for religious tolerance, on the grounds that religious coercion is a futile effort precisely because a person cannot choose to dis/believe something)
…but community can definitely be chosen, nurtured, and grown. We’ve written about this a bit before:
You might also like to check out this great book on the topic:
Purpose: Design A Community And Change Your Life – by Gina Bianchini
Want more?
We gave a ground-up primer on avoiding Alzheimer’s and other dementias; check it out:
How To Reduce Your Alzheimer’s Risk
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
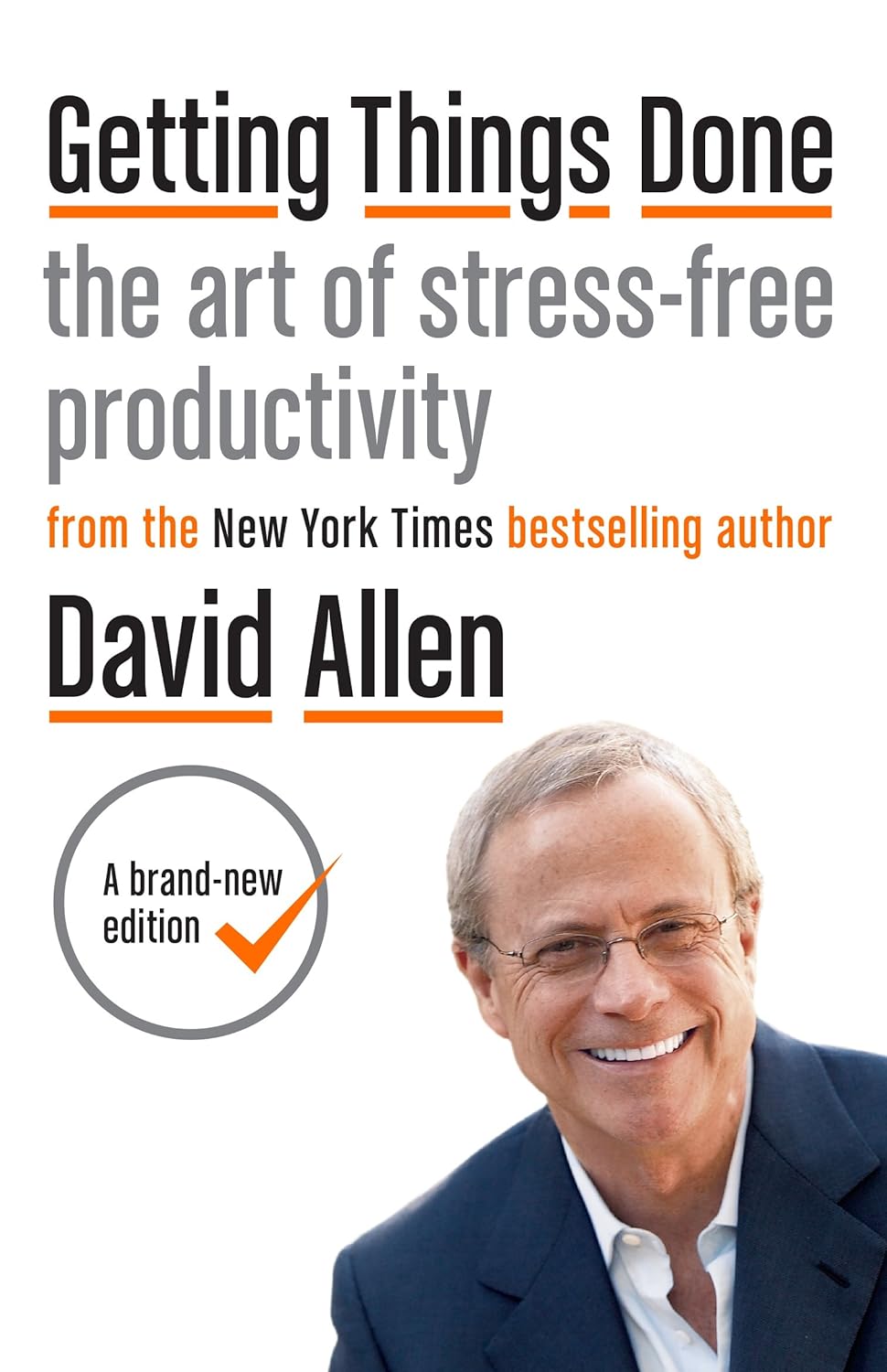
Getting Things Done – by David Allen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our “to-do” lists are usually hopelessly tangled:
“To do thing x needs thing y doing first but that can only be done with information that I must get by doing thing z”, and so on.
Suddenly that two-minute task is looking like half an hour, which is making our overall to-do list look gargantuan. Tackling tiny parts of tasks seems useless; tackling large tasks seems overwhelming. What a headache!
Getting Things Done (“GTD”, to its friends) shows us how to gather all our to-dos, and then use the quickest ways to break down a task (in reality, often a mini-project) into its constituent parts and which things can be done next, and what order to do them in (or defer, or delegate, or ditch).
In a nutshell: The GTD system aims to make all your tasks comprehensible and manageable, for stress-free productivity. No need to strategize everything every time; you have a system now, and always know where to begin.
And by popular accounts, it delivers—many put this book in the “life-changing” category.
Share This Post
-
Teen Daily Delivery Requested
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
I thoroughly enjoy your daily delivery. I’d love to see one for teens too!
That’s great to hear! The average age of our subscribers is generally rather older, but it’s good to know there’s an interest in topics for younger people. We’ll bear that in mind, and see what we can do to cater to that without alienating our older readers!
That said: it’s never too soon to be learning about stuff that affects us when we’re older—there are lifestyle factors at 20 that affect Alzheimer’s risk at 60, for example (e.g. drinking—excessive drinking at 20* is correlated to higher Alzheimer’s risk at 60).
*This one may be less of an issue for our US readers, since the US doesn’t have nearly as much of a culture of drinking under 21 as some places. Compare for example with general European practices of drinking moderately from the mid-teens, or the (happily, diminishing—but historically notable) British practice of drinking heavily from the mid-teens.
Share This Post
-
Dioscorea Villosa: Hormones, Arthritis, & Skin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
On A Wild Yam Chase?
We recently came across a supplement blend that had wild yam extract as a minor ingredient. Our plucky (and usually very knowledgable) researcher had never heard of its use before, so she set about doing her thing. This is what she found…
What health claims are made?
Wild yam extract (Dioscorea villosa) is traditionally sold and used for:
- Balancing hormones
- Combating arthritis
- Anti-aging effects for the skin
Does it balance hormones?
First, as a quick catch-up, we’ll drop a previous article of ours for your convenience:
What Does “Balance Your Hormones” Even Mean?
We couldn’t find almost any studies into wild yam extract’s hormone-balancing effects, but we did find one study, and:
❝Symptom scores showed a minor effect of both placebo and active treatment on diurnal flushing number and severity and total non-flushing symptom scores, and on nocturnal sweating after placebo, but no statistical difference between placebo and active creams.
This study suggests that short-term treatment with topical wild yam extract in women suffering from menopausal symptoms is free of side-effects, but appears to have little effect on menopausal symptoms❞
…which is a very thorough, polite, sciencey way of saying “wow, this does so many different kinds of nothing”
On the one hand, this was a small study (n=23). On the other hand, it was also literally the only study we could find.
Does it combat arthritis?
Maybe! We again didn’t find much research into this but we did find two in vitro studies that suggests that diosgenin (which can be derived from wild yam extract) helps:
- Diosgenin inhibits IL-1β-induced expression of inflammatory mediators in human osteoarthritis chondrocytes
- Diosgenin, a plant steroid, induces apoptosis in human rheumatoid arthritis synoviocytes with cyclooxygenase-2 overexpression
And we also found a rodent study that found that wild yam extract specifically helped against “acetic acid-induced writhing and formalin-induced pain“, and put that down to anti-inflammatory properties:
So, none of these studies tell us much about whether it would be helpful for humans—with or without arthritis, and hopefully without “acetic acid-induced writhing and formalin-induced pain”.
However, they do suggest that it would be reasonable to test in humans next.
You might prefer:
- Tips For Avoiding/Managing Osteoarthritis
- Tips For Avoiding/Managing Rheumatoid Arthritis
- How to Prevent (or Reduce) Inflammation
Does it keep skin young?
Again, research is thin on the ground, but we did find some! A study with wild-yam-derived diosgenin found that it didn’t make anything worse, and otherwise performed a similar role to vitamin A:
Read: Novel effects of diosgenin on skin aging
That was on rats with breast cancer though, so its applicability to healthy humans may be tenuous (while in contrast, simply getting vitamin A instead is a known deal).
Summary
- Does it balance hormones? It probably does little to nothing in this regard
- Does it combat arthritis? It probably has anti-inflammatory effects, but we know of no studies in humans. There are much more well-established anti-inflammatories out there.
- Does it keep the skin young? We know that it performs a role similar to vitamin A for rats with breast cancer, and didn’t make anything worse for them. That’s the extent of what we know.
Where can I get some?
In the unlikely event that the above research review has inspired you with an urge to buy wild yam extract, here is an example product for your convenience.
Some final words…
If you are surprised that we’re really not making any effort to persuade you of its merits, please know that (outside of the clearly-marked sponsor section, which helps us keep the lights on, so please do visit those) we have no interest in selling you anything. We’re genuinely just here to inform 🙂
If you are wondering why we ran this article at all if the supplement has negligible merits, it’s because science is science, knowledge is knowledge, and knowing that something has negligible merit can be good knowledge to have!
Also, running articles like this from time to time helps you to know that when we do sing the praises of something, it’s with good reason
Take care!
Share This Post
Related Posts
-
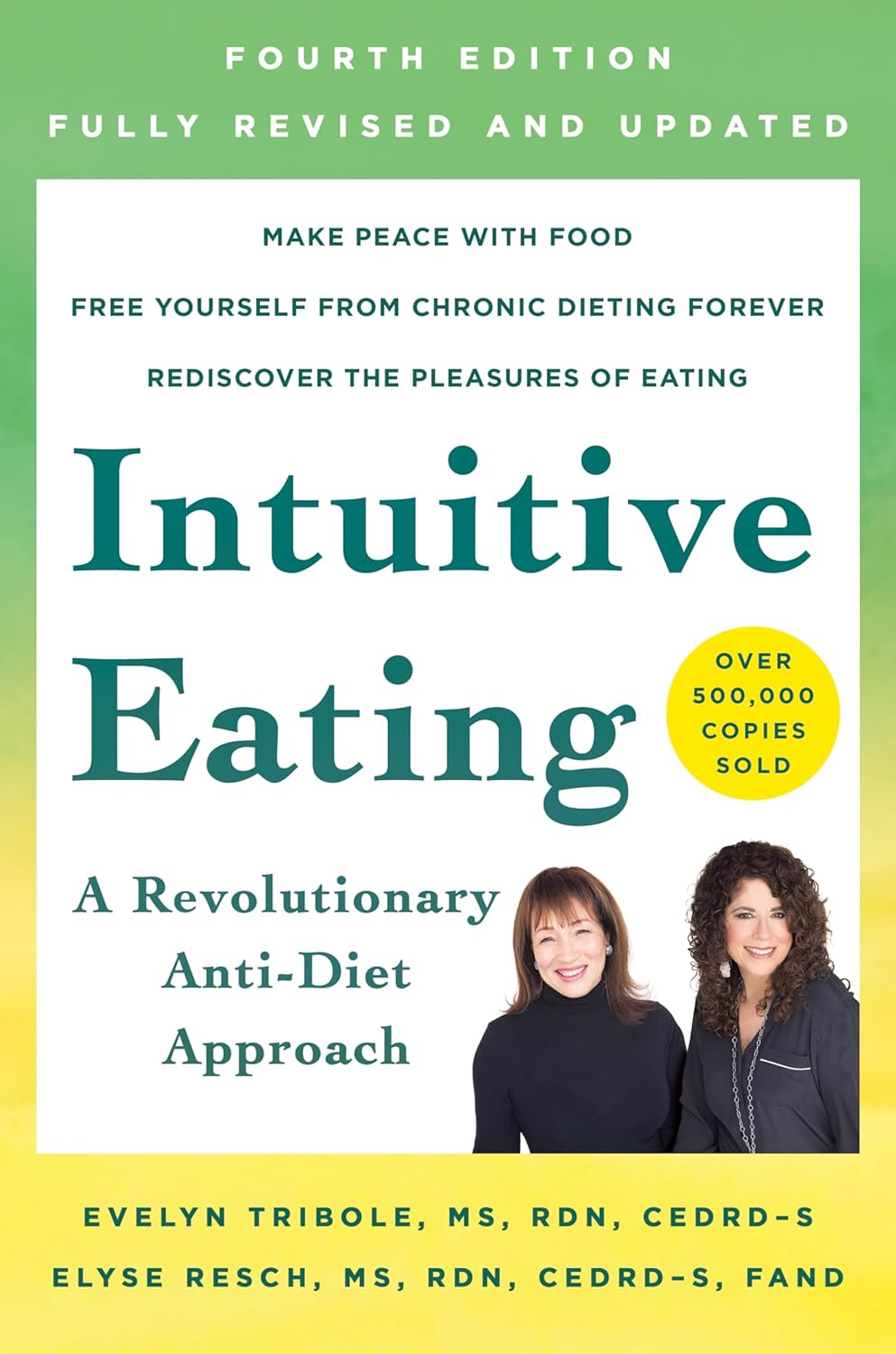
Intuitive Eating – by Evelyn Tribole and Elyse Resch
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be given to wonder: if this is about intuitive eating, and an anti-diet approach, why a whole book?
There’s a clue in the other part of the title: “4th Edition”.
The reason there’s a 4th edition (and before it, a 3rd and 2nd edition) is because this book is very much full of science, and science begets more science, and the evidence just keeps on rolling in.
While neither author is a doctor, each has a sizeable portion of the alphabet after their name (more than a lot of doctors), and this is an incredibly well-evidenced book.
The basic premise from many studies is that restrictive dieting does not work well long-term for most people, and instead, better is to make use of our bodies’ own interoceptive feedback.
You see, intuitive eating is not “eat randomly”. We do not call a person “intuitive” because they speak or act randomly, do we? Same with diet.
Instead, the authors give us ten guiding principles (yes, still following the science) to allow us a consistent “finger on the pulse” of what our body has to say about what we have been eating, and what we should be eating.
Bottom line: if you want to be a lot more in tune with your body and thus better able to nourish it the way it needs, this book is literally on the syllabus for many nutritional science classes, and will stand you in very good stead!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eat To Beat Chronic Fatigue!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Eat To Beat Chronic Fatigue
Chronic fatigue is on the rise, and it can make life a living Hell. Days blur into one, and you try to take each day as it comes, but sometimes several days gang up on you at once.
You probably know some lifestyle changes that might help—if only you had the energy to implement them.
You’d like to eat well, but you need to…
- Buy the fresh produce (and take a little rest after)
- Put the groceries away (and take a little rest after)
- Wash the vegetables (and take a little rest after)
- Chop the things as necessary (and take a little rest after)
- Cook dinner (and take a little rest after)
…and now you’re too exhausted to eat it.
So, what can be done?
First, avoid things that cause inflammation, as this is a major contributor to chronic fatigue. You might like our previous main feature:
Next up, really do stay hydrated. It’s less about quantity, and more about ubiquity. Hydrate often.
Best is if you always have some (hydrating) drink on the go.
Do experiment with your diet, and/but keep a food journal of what you eat and how you feel 30–60 minutes after eating it. Only make one change at a time, otherwise you won’t know which change made the difference.
Notice what patterns emerge over time, and adjust your ingredients accordingly.
Limit your caffeine intake. We know that sometimes it seems like the only way to get through the day, but you will always crash later, because it was only ever taxing your adrenal system (thus: making you more tired in the long run) and pulling the wool over the eyes of your adenosine receptors (blocking you from feeling how tired you are, but not actually reducing your body’s tiredness).
Put simply, caffeine is the “payday loan” of energy.
Eat more non-starchy vegetables, and enjoy healthy fats. Those healthy fats can come from nuts and seeds, avocado, or fish (not fried, though!).
The non-starchy vegetables will boost your vitamins and fiber while being easy on your beleaguered metabolism, while the healthy fats will perk up your energy levels without spiking insulin like sugars would.
Pay the fatigue tax up front. What this means is… Instead of throwing away vegetables that didn’t get used because it would take too much effort and you just need an easier dinner today, buy ready-chopped vegetables, for example.
And if you buy vegetables frozen, they’re also often not only cheaper, but also (counterintuitively) contain more nutrients.
A note of distinction:
Many more people have chronic fatigue (the symptom: being exhausted all the time) than have chronic fatigue syndrome (the illness: myalgic encephalomyelitis).
This is because fatigue can be a symptom of many, many other conditions, and can be heavily influenced by lifestyle factors too.
A lot of the advice for dealing with chronic fatigue is often the same in both cases, but some will be different, because for example:
- If your fatigue is from some other condition, that condition probably impacts what lifestyle factors you are (and are not) able to change, too
- If your fatigue is from lifestyle factors, that hopefully means you can change those and enjoy less fatigue…
- But if it’s not from lifestyle factors, as in ME/CFS, then advice to “exercise more” etc is not going to help so much.
There are ways to know the difference though:
Check out: Do You Have Chronic Fatigue Syndrome?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Not to Age – by Dr. Michael Greger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First things first: it’s a great book, and it’s this reviewer’s favorite of Dr. Greger’s so far (for posterity: it’s just been published and this reviewer has just finished reading the copy she got on pre-order)
Unlike many popular physician authors, Dr. Greger doesn’t rehash a lot of old material, and instead favours prioritizing new material in each work. Where appropriate, he’ll send the reader to other books for more specific information (e.g: you want to know how to avoid premature death? Go read How Not To Die. You want to know how to lose weight? How Not To Diet. Etc).
In the category of new information, he has a lot to offer here. And with over 8,000 references, it’s information, not conjecture. On which note, we recommend the e-book version if that’s possible for you, for three reasons:
- It’s possible to just click the references and be taken straight to the cited paper itself online
- To try to keep the book’s size down, Dr. Greger has linked to other external resources too
- The only negative reviews on Amazon, so far, are people complaining that the print copy’s text is smaller than they’d like
For all its information-density (those 8,000+ references are packed into 600ish pages), the book is very readable even to a lay reader; the author is a very skilled writer.
As for the content, we can’t fit more than a few sentences here so forgive the brevity, but we’ll mention that he covers:
- Slowing 11 pathways of aging
- The optimal anti-aging regimen according to current best science
- Preserving function (specific individual aspects of aging, e.g. hearing, sight, cognitive function, sexual function, hair, bones, etc)
- “Dr. Greger’s Anti-Aging Eight”
In terms of “flavor” of anti-aging science, his approach can be summed up as: diet and lifestyle as foundation; specific supplements and interventions as cornerstones.
Bottom line: this is now the anti-aging book.
Click here to check out How Not To Age, and look after yourself with the best modern science!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: