Does intermittent fasting have benefits for our brain?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Intermittent fasting has become a popular dietary approach to help people lose or manage their weight. It has also been promoted as a way to reset metabolism, control chronic disease, slow ageing and improve overall health.
Meanwhile, some research suggests intermittent fasting may offer a different way for the brain to access energy and provide protection against neurodegenerative diseases like Alzheimer’s disease.
This is not a new idea – the ancient Greeks believed fasting enhanced thinking. But what does the modern-day evidence say?
First, what is intermittent fasting?
Our diets – including calories consumed, macronutrient composition (the ratios of fats, protein and carbohydrates we eat) and when meals are consumed – are factors in our lifestyle we can change. People do this for cultural reasons, desired weight loss or potential health gains.
Intermittent fasting consists of short periods of calorie (energy) restriction where food intake is limited for 12 to 48 hours (usually 12 to 16 hours per day), followed by periods of normal food intake. The intermittent component means a re-occurrence of the pattern rather than a “one off” fast.
Food deprivation beyond 24 hours typically constitutes starvation. This is distinct from fasting due to its specific and potentially harmful biochemical alterations and nutrient deficiencies if continued for long periods.
4 ways fasting works and how it might affect the brain
The brain accounts for about 20% of the body’s energy consumption.
Here are four ways intermittent fasting can act on the body which could help explain its potential effects on the brain.
1. Ketosis
The goal of many intermittent fasting routines is to flip a “metabolic switch” to go from burning predominately carbohydrates to burning fat. This is called ketosis and typically occurs after 12–16 hours of fasting, when liver and glycogen stores are depleted. Ketones – chemicals produced by this metabolic process – become the preferred energy source for the brain.
Due to this being a slower metabolic process to produce energy and potential for lowering blood sugar levels, ketosis can cause symptoms of hunger, fatigue, nausea, low mood, irritability, constipation, headaches, and brain “fog”.
At the same time, as glucose metabolism in the brain declines with ageing, studies have shown ketones could provide an alternative energy source to preserve brain function and prevent age-related neurodegeneration disorders and cognitive decline.
Consistent with this, increasing ketones through supplementation or diet has been shown to improve cognition in adults with mild cognitive decline and those at risk of Alzheimer’s disease respectively.
2. Circadian syncing
Eating at times that don’t match our body’s natural daily rhythms can disrupt how our organs work. Studies in shift workers have suggested this might also make us more prone to chronic disease.
Time-restricted eating is when you eat your meals within a six to ten-hour window during the day when you’re most active. Time-restricted eating causes changes in expression of genes in tissue and helps the body during rest and activity.
A 2021 study of 883 adults in Italy indicated those who restricted their food intake to ten hours a day were less likely to have cognitive impairment compared to those eating without time restrictions.

Shutterstock
3. Mitochondria
Intermittent fasting may provide brain protection through improving mitochondrial function, metabolism and reducing oxidants.
Mitochondria’s main role is to produce energy and they are crucial to brain health. Many age-related diseases are closely related to an energy supply and demand imbalance, likely attributed to mitochondrial dysfunction during ageing.
Rodent studies suggest alternate day fasting or reducing calories by up to 40% might protect or improve brain mitochondrial function. But not all studies support this theory.
4. The gut-brain axis
The gut and the brain communicate with each other via the body’s nervous systems. The brain can influence how the gut feels (think about how you get “butterflies” in your tummy when nervous) and the gut can affect mood, cognition and mental health.
In mice, intermittent fasting has shown promise for improving brain health by increasing survival and formation of neurons (nerve cells) in the hippocampus brain region, which is involved in memory, learning and emotion.

Shutterstock
There’s no clear evidence on the effects of intermittent fasting on cognition in healthy adults. However one 2022 study interviewed 411 older adults and found lower meal frequency (less than three meals a day) was associated with reduced evidence of Alzheimer’s disease on brain imaging.
Some research has suggested calorie restriction may have a protective effect against Alzheimer’s disease by reducing oxidative stress and inflammation and promoting vascular health.
When we look at the effects of overall energy restriction (rather than intermittent fasting specifically) the evidence is mixed. Among people with mild cognitive impairment, one study showed cognitive improvement when participants followed a calorie restricted diet for 12 months.
Another study found a 25% calorie restriction was associated with slightly improved working memory in healthy adults. But a recent study, which looked at the impact of calorie restriction on spatial working memory, found no significant effect.
Bottom line
Studies in mice support a role for intermittent fasting in improving brain health and ageing, but few studies in humans exist, and the evidence we have is mixed.
Rapid weight loss associated with calorie restriction and intermittent fasting can lead to nutrient deficiencies, muscle loss, and decreased immune function, particularly in older adults whose nutritional needs may be higher.
Further, prolonged fasting or severe calorie restriction may pose risks such as fatigue, dizziness, and electrolyte imbalances, which could exacerbate existing health conditions.
If you’re considering intermittent fasting, it’s best to seek advice from a health professional such as a dietitian who can provide guidance on structuring fasting periods, meal timing, and nutrient intake. This ensures intermittent fasting is approached in a safe, sustainable way, tailored to individual needs and goals.
Hayley O’Neill, Assistant Professor, Faculty of Health Sciences and Medicine, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A Urologist Explains Edging: What, Why, & Is It Safe?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Edging” is the practice of intentionally delaying orgasm, which can be enjoyed by anyone, with a partner or alone.
On the edge
Question: why?
Answer: the more tension is built up, the stronger the orgasm can be at the end of it. And, even before then, pleasure along the way is pleasure along the way, which is generally considered a good thing—especially for any (usually but not always women, for hormonal and social reasons) who find it difficult to orgasm. It’s also a great way to experiment and learn more about one’s own body and/or that of one’s partner(s), personal responses, and so forth. Also, for any (usually but not always men, for hormonal reasons) who find they usually orgasm sooner than they’d like, it’s a great way to change that, if changing that is what’s wanted.
Bonus answer: for some (usually but not always men, for hormonal reasons) who find they have an uncomfortable slump in mood after orgasm, that can simply be skipped entirely, postponed for another time, etc, with pleasure being derived from the sexual activity rather than orgasm. That way, there’s a lasting dopamine high, with no prolactin crash afterwards ← this is very much tied to male hormones, by the way. If you have female hormones, there’s usually no prolactin crash either way, and instead, the post-orgasm spike in oxytocin is stronger, and a wave of serotonin makes the later decline of dopamine much more gentle.
Question: can it cause any problems?
Answer: yep! Or rather, subjectively, it may be considered so—this is obviously a personal matter and your mileage may vary. The main problem it may cause is that if practised habitually, it may result in greater difficulty achieving orgasm, simply because the body has got used to “ok, when we do this (sex/masturbation), we are in no particular rush to do that (orgasm)”. So whether not this would be a worry for you is down to any given individual. Lastly, if your intent was a long edging session with an orgasm at the end and then something happened to interrupt that, then your orgasm may be unintentionally postponed to another time, which again, may be more or less of an issue depending on your feelings about that.
For more on these things including advice on how to try it, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Mythbusting The Big O ← 10almonds main feature on orgasms, health, and associated myths
- Come Together: The Science (and Art) of Creating Lasting Sexual Connections – by Dr. Emily Nagoski
- Better Sex Through Mindfulness: How Women Can Cultivate Desire – by Dr. Lori Brotto
Take care!
Share This Post
-
5 Ways To Beat Cancer (And Other Diseases)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Systematic Approach To Healthy Eating
This is Dr. William Li. He’s a physician, cancer researcher, and educator. He also founded the Angiogenesis Foundation back in 1994.
We recently reviewed one of his books, “Eat To Beat Disease”.
He has another book that we haven’t reviewed at time of writing, “Eat To Beat Your Diet“, which you might like to check out.
What does he want us to know?
He wants us to know how to eat to beat cancer and other diseases, by means of five specific angles:
Angiogenesis
This is about replacing blood vessels, which of course happens all the time, but it becomes a problem when it is feeding a cancer in the process.
Here, based on Dr. Li’s work, is what can be done about it:
A List of Anti-Angiogenic Foods for a Cancer-Fighting Diet
Regeneration
Generally speaking, we want to replace healthy cells early, because if we wait until they get damaged, then that damage will be copied forwards. As well as intermittent fasting, there are other things we can do to promote this—even, Dr. Li’s research shows, for stem cells:
Doctor’s Tip: Regeneration (stem cells)—one of your body’s five defense systems
Microbiome health
Healthy gut, healthy rest of the body. We’ve written about this before:
Making Friends With Your Gut (You Can Thank Us Later)
DNA protection
DNA gets unravelled and damaged with age, the telomere caps get shorter, and mistakes get copied forward. So there more we can protect our DNA, the longer we can live healthily. There are many ways to do this, but Dr. Li was one of the first to bring to light the DNA-protecting benefits of kiwi fruit:
Immunity
Paradoxically, what’s good for your immune system (making it stronger) also helps to protect against autoimmune diseases (for most people, for the most part).
In short: it’s good to have an immune system that’s powerful not just in its counterattacks, but also in its discerning nature. There are dietary and other lifestyle approaches to both, and they’re mostly the same things:
Beyond Supplements: The Real Immune-Boosters!
and thus see also:
Want to know more?
You might enjoy his blog or podcast, and here’s his TED talk:
Want to watch it, but not right now? Bookmark it for later
Enjoy!
Share This Post
-
Podiatrists Debunk 11 Feet Myths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Podiatrists Dr. Sarah Haller and Dr. Brad Schaeffer put us on a better path:
Don’t get wrong-footed
We’ll not keep the 11 myths a mystery; they are…
- “You have warts because your feet are dirty.”
False! Warts are caused by a virus, not dirt. Viruses can be picked up from surfaces like yoga mats, pools, gyms, and showers. - “Bunions are caused by wearing heels.”
False! Bunions are genetic deformities where the bone behind the big toe shifts. Heels might worsen them but don’t cause them. - “Cutting the sides of my toenail will prevent an ingrown toenail.”
False! Toenails should be cut straight across. Cutting the sides can make ingrown toenails worse. - “Pedicures gave me toenail fungus.”
Partially true! You can get fungus from many places, but safe, sterile pedicures are generally fine. - “Only athletes get athlete’s foot.”
False! Athlete’s foot is a fungal infection caused by warm, moist environments. Anyone can get it, not just athletes. - “My feet are fine because I trained them to walk in stilettos.”
False! You can get used to stilettos, but they aren’t healthy long-term. They shorten the Achilles tendon and put pressure on the foot. - “You can’t do anything for a broken toe.”
False! Broken toes can be treated and should be checked by a doctor. They may need to be set for proper healing. - “It’s normal for your feet to hurt from standing all day.”
False! Foot pain isn’t normal and can be prevented with proper footwear, support, and compression socks. - “All inserts are the same.”
False! Everyone’s feet are different. Some may benefit from over-the-counter insoles, but others need custom orthotics. - “Sprained ankles are no big deal.”
False! Sprains can damage ligaments and lead to instability or arthritis if untreated. Proper stabilization is essential. - “If I can walk after an injury, I don’t need to see a doctor.”
False! You can still have serious injuries like fractures even if you can walk. Always get checked after an injury.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Steps For Keeping Your Feet A Healthy Foundation
Take care!
Share This Post
- “You have warts because your feet are dirty.”
Related Posts
-
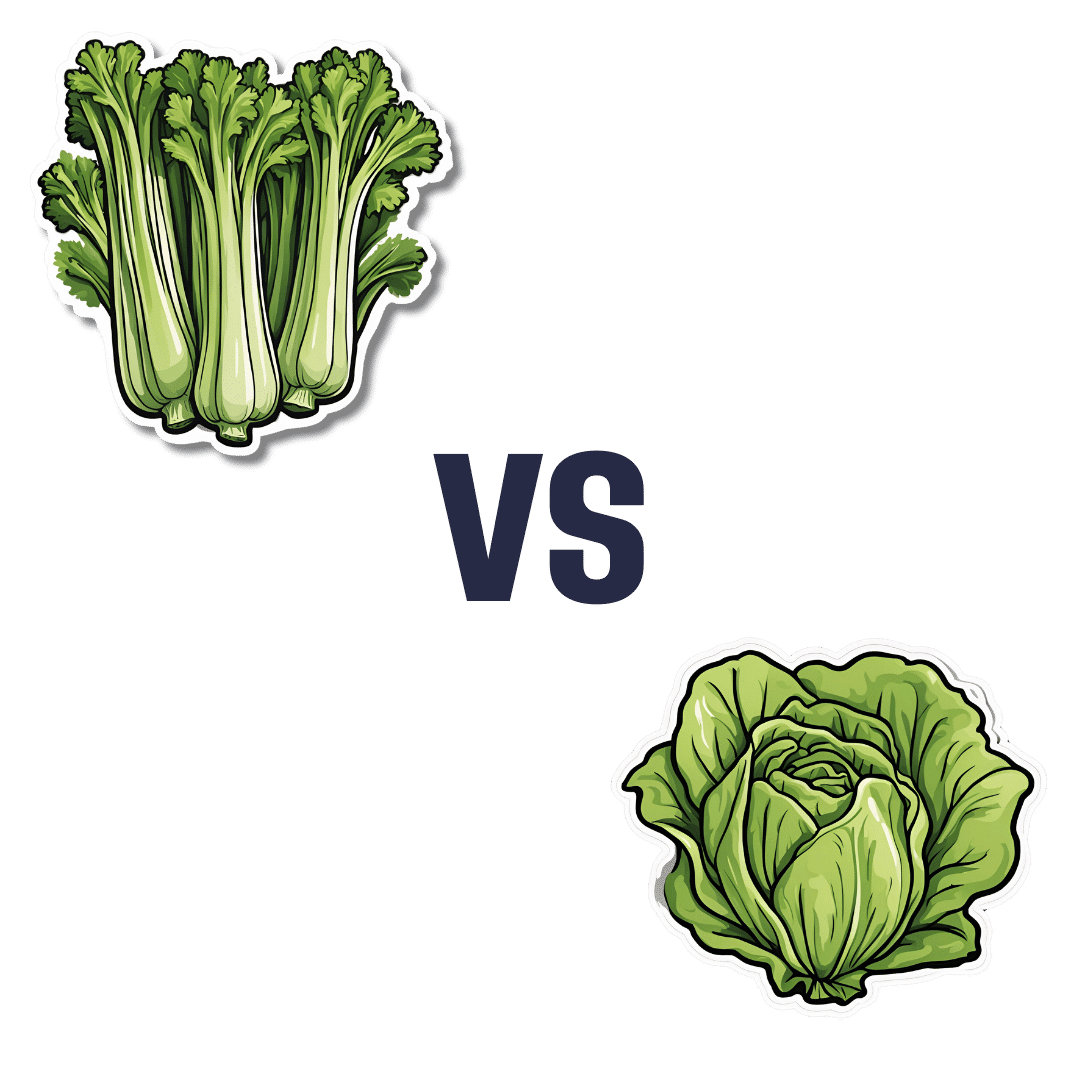
Celery vs Lettuce – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to lettuce, we picked the lettuce.
Why?
Let us consider the macros first: lettuce has 2x the protein, but of course the numbers are tiny and probably nobody is eating this for the protein. Both of these salad items are roughly comparable in terms of carbs and fiber, being both mostly water with just enough other stuff to hold their shape. Nominally this section is a slight win for lettuce on account of the protein, but in realistic practical terms, it’s a tie.
In terms of vitamins, celery has more of vitamins B5 and E, while lettuce has more of vitamins A, B1, B2, B3, B6, B7, B9, C, K, and choline. An easy win for lettuce here.
In the category of minerals, celery has more calcium, copper, and potassium, while lettuce has more iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. So, a fair win for lettuce.
Adding up the sections makes for an overall win for lettuce; of course, enjoy both, though!
Want to learn more?
You might like to read:
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Triple Your Breast Cancer Survival Chances
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Keeping Abreast Of Your Cancer Risk
It’s the kind of thing that most people think won’t happen to them. And hopefully, it won’t!
But…
- Anyone (who has not had a double mastectomy*, anyway) can get breast cancer.
- *and even this depends on the type of double mastectomy and other circumstances, and technically there will always be a non-zero risk, because of complicating factors.
- Breast cancer, if diagnosed early (before it spreads), has a 98% survival rate.
- That survival rate drops to 31% if diagnosed after it has spread through the body.
(The US CDC’s breast cancer “stat bite” page has more stats and interactive graphs, so click here to see those charts and get the more detailed low-down on mortality/survival rates with various different situations)
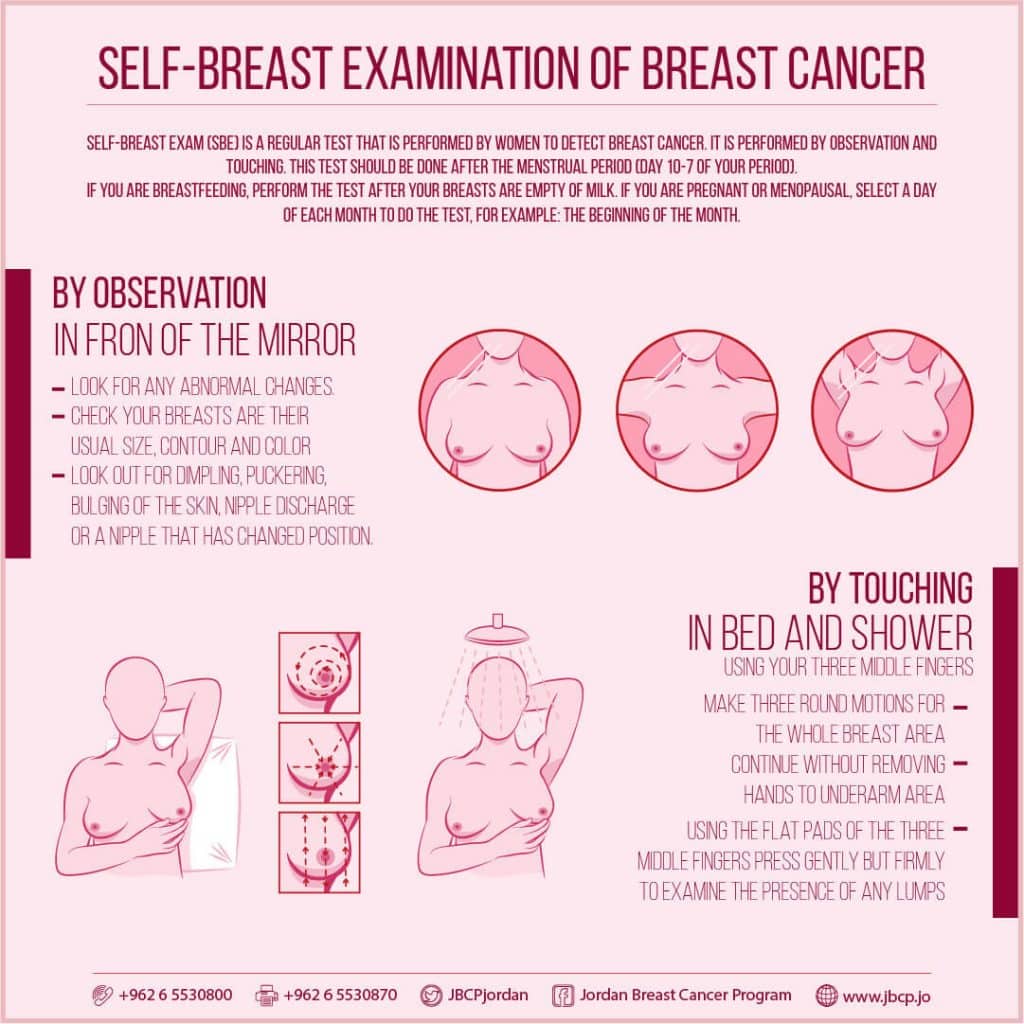
We think that the difference between 98% and 31% survival rates is more than enough reason to give ourselves a monthly self-check at the very least! You’ve probably seen how-to diagrams before, but here are instructions for your convenience:
(This graphic was created by the Jordan Breast Cancer Program—check them out, as they have lots of resources)
If you don’t have the opportunity to take matters into your own hands right now, rather than just promise yourself “I’ll do that later”, take this free 4-minute Breast Health Assessment from Aurora Healthcare. Again, we think the difference early diagnosis can make to your survival chances make these tests well worth it:
Click Here To Take The Free 4-Minute Breast Health Assessment!
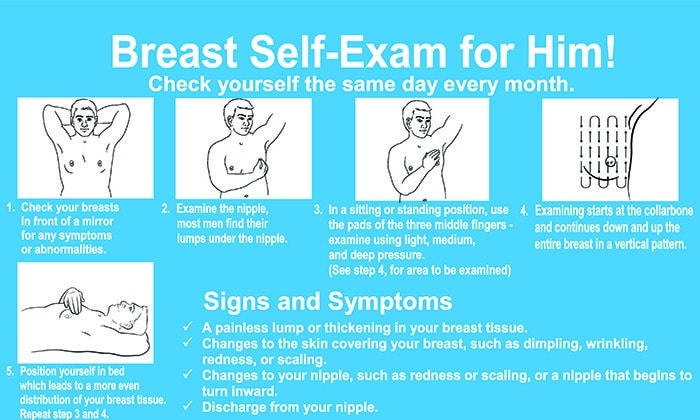
Lest we forget, men can also get breast cancer (the CDC has a page for men too), especially if over 50. But how do you check for breast cancer, when you don’t have breasts in the commonly-understood sense of the word?
So take a moment to do this (yes, really actually do it!), and set a reminder in your calendar to repeat it monthly—there really is no reason not to!
Take care of yourself; you’re important.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Anyone (who has not had a double mastectomy*, anyway) can get breast cancer.
-
Glucomannan For Weight Loss, Gut Health, & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Glucomannan is a water-soluble dietary fiber found in the root of the konjac plant.
If you’ve had konjac noodles, also called shirataki, that’s what those are mostly made of, and it’s why they have next-to-no calories.
You may be wondering: if it’s water-soluble, how do the noodles not dissolve in water? And the answer is that the noodle-making process involves making a gel out of the fiber and water, which is then extruded into noodle shapes. In this gelatinous form, they’re fairly stable (it’s one of the most viscous dietary fibers), but yes, if you were to boil them for a long time, they would indeed turn the entire liquid contents of the saucepan into gel.
How it works for weight loss
Because of its viscosity, adding even a small amount of powdered* glucomannan to a glass of water will turn the whole thing into gel in seconds. This means that if you take glucomannan capsules with a glass of water, then so far as your stomach is concerned, you just ate a cup of gel, and the water is now processed as food, staying longer in the stomach than it otherwise would, and promoting feelings of fullness.
*i.e. dry powder, not in a gelatinous form like the noodles
As for its efficacy in weight loss, see for example:
❝Glucomannan was well-tolerated and resulted in significant weight loss in overweight and obese individuals❞
Read more: Glucomannan and obesity: a critical review
So, that covers the basic requirements, but may be wondering: does it have other benefits? And the answer is yes, it does:
❝Glucomannan appears to beneficially affect total cholesterol, LDL cholesterol, triglycerides, body weight, and fasting blood glucose❞
To further corroborate that and comment on safety…
❝Results showed a significant mean weight loss using glucomannan over an eight-week period. Serum cholesterol and low-density lipoprotein cholesterol were significantly reduced in the glucomannan treated group. No adverse reactions to glucomannan were reported.❞
Read more: Effect of glucomannan on obese patients: a clinical study
As to whether other gel-making agents work the same way, the answer is no, they don’t seem to:
❝Glucomannan induced body weight reduction in healthy overweight subjects, whereas the addition of guar gum and alginate did not seem to cause additional loss of weight❞
Read more: Experiences with three different fiber supplements in weight reduction
How it works for gut health
In the words of Dr. Yu Li et al.,
❝Konjaku flour can achieve positive effects on treating obesity, which manifest on reducing BMI, fat mass, blood glucose, and blood lipid, improving hepatic function, and also regulating intestinal microfloral structure.
Therefore, changes in gut microbiota may explain in part the effects of konjaku flour.❞
Read in full: Effects of Konjaku Flour on the Gut Microbiota of Obese Patients
This has extra positive knock-on effects too:
Want to try some?
We don’t sell it, but here for your convenience are example products on Amazon:
Konjac noodles | Glucomannan capsules
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: