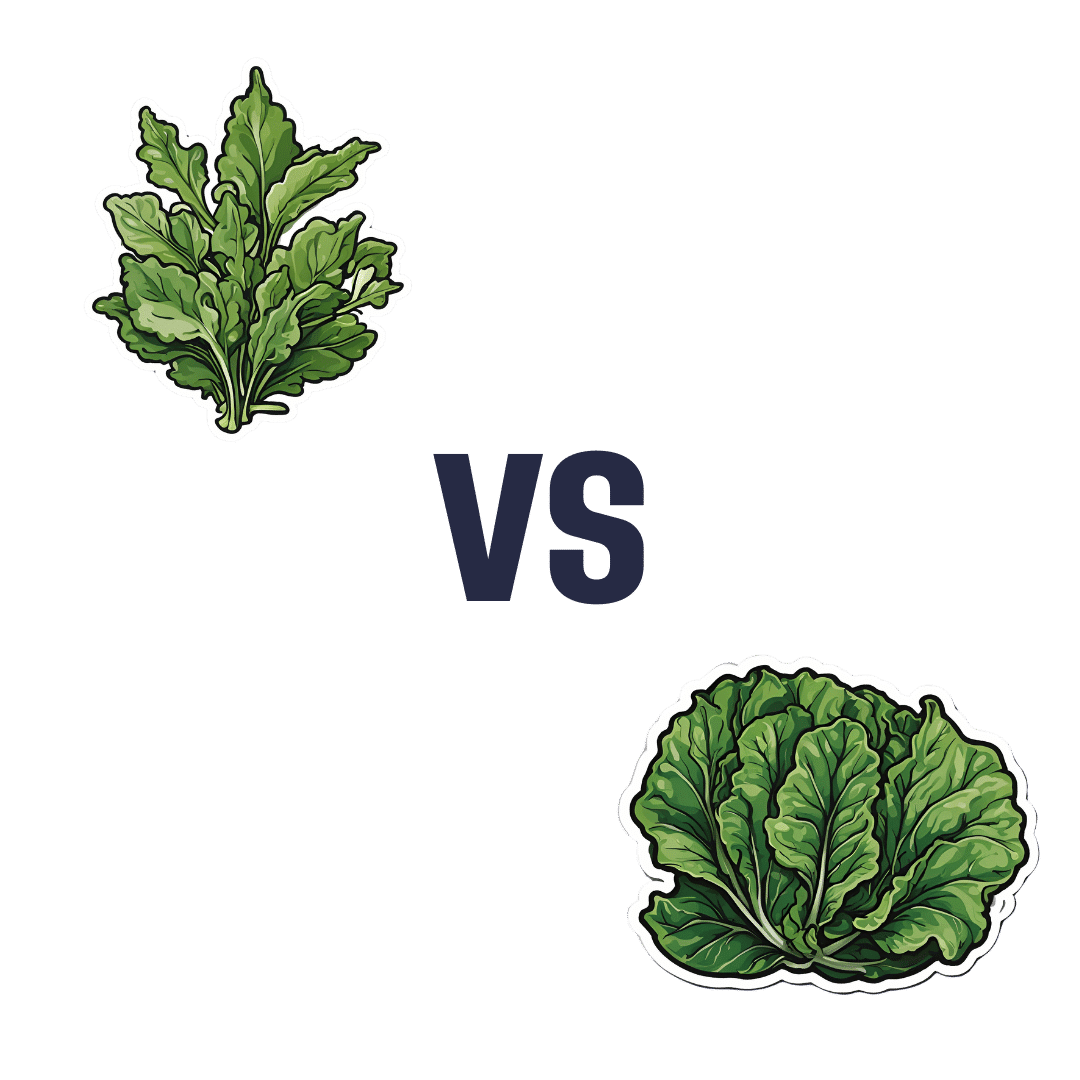
Dandelion Greens vs Collard Greens – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dandelion greens to collard greens, we picked the dandelion greens.
Why?
Collard greens are great—they even beat kale in one of our previous “This or That” articles!—but dandelion greens simply pack more of a nutritional punch:
In terms of macros, dandelions have slightly more carbs (+3g/100g) for the same protein and fiber, and/but the glycemic index is equal (zero), so those carbs aren’t anything to worry about. Nobody is getting metabolic disease by getting their carbs from dandelion leaves. In short, we’re calling it a tie on macros, though it could nominally swing either way if you have an opinion (one way or the other) about the extra 3g of carbs.
In the category of vitamins, things are more exciting: dandelion greens have more of vitamins A, B1, B2, B3, B6, B7, B9, C, E, and K, while collard greens have more vitamin B5. An easy and clear win for dandelions.
Looking at the minerals tells a similar story; dandelion greens have much more calcium, copper, iron, magnesium, phosphorus, potassium, and zinc, while collard greens have slightly more manganese. Another overwhelming win for dandelions.
One more category, polyphenols. We’d be here until next week if we listed all the polyphenols that dandelion greens have, but suffice it to say, dandelion greens have a total of 385.55mg/100g polyphenols, while collard greens have a total of 0.08mg/100g polyphenols. Grabbing a calculator, we see that this means dandelions have more than 4819x the polyphenol content that collard greens do.
So, “eat leafy greens” is great advice, but they are definitely not all created equal!
Let us take this moment to exhort: if you have any space at home where you can grow dandelions, grow them!
Not only are they great for pollinators, but also they beat the collard greens that beat kale. And you can have as much as you want, for free, right there.
Want to learn more?
You might like to read:
Collard Greens vs Kale – Which is Healthier?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Your Brain on Art – by Susan Magsamen & Ivy Ross
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The notion of art therapy is popularly considered a little wishy-washy. As it turns out, however, there are thousands of studies showing its effectiveness.
Nor is this just a matter of self-expression. As authors Magsamen and Ross explore, different kinds of engagement with art can convey different benefits.
That’s one of the greatest strengths of this book: “this form of engagement with art will give these benefits, according to these studies”
With benefits ranging from reducing stress and anxiety, to overcoming psychological trauma or physical pain, there’s a lot to be said for art!
And because the book covers many kinds of art, if you can’t imagine yourself taking paintbrush to canvas, that’s fine too. We learn of the very specific cognitive benefits of coloring in mandalas (yes, really), of sculpting something terrible in clay, or even just of repainting the kitchen, and more. Each thing has its set of benefits.
The book’s main goal is to encourage the reader to cultivate what the authors call an aesthetic mindset, which involves four key attributes:
- a high level of curiosity
- a love of playful, open-ended exploration
- a keen sensory awareness
- a drive to engage in creative activities
And, that latter? It’s as a maker and/or a beholder. We learn about what we can gain just by engaging with art that someone else made, too.
Bottom line: come for the evidence-based cognitive benefits; stay for the childlike wonder of the universe. If you already love art, or have thought it’s just “not for you”, then this book is for you.
Click here to check out Your Brain On Art, and open up whole new worlds of experience!
Share This Post
-
The Lost Art of Silence – by Sarah Anderson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From “A Room Of One’s Own” to “Silent Mondays”, from spiritual retreats to noise-cancelling headphones, this book covers the many benefits of silence—and a couple of downsides too.
In an age where most things are available at the touch of a button, a little peaceful solitude can come at quite a premium, but what it offers can effect all manner of physical changes, from reduced stress responses to increased neurogenesis (growing new brain cells).
The tone throughout is a combination of personal and pop-science, and it’s very motivating to find a little more space-between-the-things in life.
The book is best enjoyed in a quiet room.
Bottom line: if you get the feeling sometimes that you could rest and recover fully and properly if you could just find the downtime, this book will help you find exactly that.
Click here to check out the Lost Art of Silence, and find peace and strength in it!
Share This Post
-
Traveling To Die: The Latest Form of Medical Tourism
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the 18 months after Francine Milano was diagnosed with a recurrence of the ovarian cancer she thought she’d beaten 20 years ago, she traveled twice from her home in Pennsylvania to Vermont. She went not to ski, hike, or leaf-peep, but to arrange to die.
“I really wanted to take control over how I left this world,” said the 61-year-old who lives in Lancaster. “I decided that this was an option for me.”
Dying with medical assistance wasn’t an option when Milano learned in early 2023 that her disease was incurable. At that point, she would have had to travel to Switzerland — or live in the District of Columbia or one of the 10 states where medical aid in dying was legal.
But Vermont lifted its residency requirement in May 2023, followed by Oregon two months later. (Montana effectively allows aid in dying through a 2009 court decision, but that ruling doesn’t spell out rules around residency. And though New York and California recently considered legislation that would allow out-of-staters to secure aid in dying, neither provision passed.)
Despite the limited options and the challenges — such as finding doctors in a new state, figuring out where to die, and traveling when too sick to walk to the next room, let alone climb into a car — dozens have made the trek to the two states that have opened their doors to terminally ill nonresidents seeking aid in dying.
At least 26 people have traveled to Vermont to die, representing nearly 25% of the reported assisted deaths in the state from May 2023 through this June, according to the Vermont Department of Health. In Oregon, 23 out-of-state residents died using medical assistance in 2023, just over 6% of the state total, according to the Oregon Health Authority.
Oncologist Charles Blanke, whose clinic in Portland is devoted to end-of-life care, said he thinks that Oregon’s total is likely an undercount and he expects the numbers to grow. Over the past year, he said, he’s seen two to four out-of-state patients a week — about one-quarter of his practice — and fielded calls from across the U.S., including New York, the Carolinas, Florida, and “tons from Texas.” But just because patients are willing to travel doesn’t mean it’s easy or that they get their desired outcome.
“The law is pretty strict about what has to be done,” Blanke said.
As in other states that allow what some call physician-assisted death or assisted suicide, Oregon and Vermont require patients to be assessed by two doctors. Patients must have less than six months to live, be mentally and cognitively sound, and be physically able to ingest the drugs to end their lives. Charts and records must be reviewed in the state; neglecting to do so constitutes practicing medicine out of state, which violates medical licensing requirements. For the same reason, the patients must be in the state for the initial exam, when they request the drugs, and when they ingest them.
State legislatures impose those restrictions as safeguards — to balance the rights of patients seeking aid in dying with a legislative imperative not to pass laws that are harmful to anyone, said Peg Sandeen, CEO of the group Death With Dignity. Like many aid-in-dying advocates, however, she said such rules create undue burdens for people who are already suffering.
Diana Barnard, a Vermont palliative care physician, said some patients cannot even come for their appointments. “They end up being sick or not feeling like traveling, so there’s rescheduling involved,” she said. “It’s asking people to use a significant part of their energy to come here when they really deserve to have the option closer to home.”
Those opposed to aid in dying include religious groups that say taking a life is immoral, and medical practitioners who argue their job is to make people more comfortable at the end of life, not to end the life itself.
Anthropologist Anita Hannig, who interviewed dozens of terminally ill patients while researching her 2022 book, “The Day I Die: The Untold Story of Assisted Dying in America,” said she doesn’t expect federal legislation to settle the issue anytime soon. As the Supreme Court did with abortion in 2022, it ruled assisted dying to be a states’ rights issue in 1997.
During the 2023-24 legislative sessions, 19 states (including Milano’s home state of Pennsylvania) considered aid-in-dying legislation, according to the advocacy group Compassion & Choices. Delaware was the sole state to pass it, but the governor has yet to act on it.
Sandeen said that many states initially pass restrictive laws — requiring 21-day wait times and psychiatric evaluations, for instance — only to eventually repeal provisions that prove unduly onerous. That makes her optimistic that more states will eventually follow Vermont and Oregon, she said.
Milano would have preferred to travel to neighboring New Jersey, where aid in dying has been legal since 2019, but its residency requirement made that a nonstarter. And though Oregon has more providers than the largely rural state of Vermont, Milano opted for the nine-hour car ride to Burlington because it was less physically and financially draining than a cross-country trip.
The logistics were key because Milano knew she’d have to return. When she traveled to Vermont in May 2023 with her husband and her brother, she wasn’t near death. She figured that the next time she was in Vermont, it would be to request the medication. Then she’d have to wait 15 days to receive it.
The waiting period is standard to ensure that a person has what Barnard calls “thoughtful time to contemplate the decision,” although she said most have done that long before. Some states have shortened the period or, like Oregon, have a waiver option.
That waiting period can be hard on patients, on top of being away from their health care team, home, and family. Blanke said he has seen as many as 25 relatives attend the death of an Oregon resident, but out-of-staters usually bring only one person. And while finding a place to die can be a problem for Oregonians who are in care homes or hospitals that prohibit aid in dying, it’s especially challenging for nonresidents.
When Oregon lifted its residency requirement, Blanke advertised on Craigslist and used the results to compile a list of short-term accommodations, including Airbnbs, willing to allow patients to die there. Nonprofits in states with aid-in-dying laws also maintain such lists, Sandeen said.
Milano hasn’t gotten to the point where she needs to find a place to take the meds and end her life. In fact, because she had a relatively healthy year after her first trip to Vermont, she let her six-month approval period lapse.
In June, though, she headed back to open another six-month window. This time, she went with a girlfriend who has a camper van. They drove six hours to cross the state border, stopping at a playground and gift shop before sitting in a parking lot where Milano had a Zoom appointment with her doctors rather than driving three more hours to Burlington to meet in person.
“I don’t know if they do GPS tracking or IP address kind of stuff, but I would have been afraid not to be honest,” she said.
That’s not all that scares her. She worries she’ll be too sick to return to Vermont when she is ready to die. And, even if she can get there, she wonders whether she’ll have the courage to take the medication. About one-third of people approved for assisted death don’t follow through, Blanke said. For them, it’s often enough to know they have the meds — the control — to end their lives when they want.
Milano said she is grateful she has that power now while she’s still healthy enough to travel and enjoy life. “I just wish more people had the option,” she said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
Rise And (Really) Shine!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Q&A with 10almonds Subscribers!
Q: Would love to hear more ideas about effective first thing in the morning time management to get a great start on your day.
A: There are a lot of schools of thought about what’s best in this regard! Maybe we’ll do a main feature sometime. But some things that are almost universally agreed upon are:
- Prepare your to-do list the night before
- Have some sort of buffer between waking up and getting to productivity.
- For me (hi, your writer here) it’s my first coffee of the day. It’s not even about the caffeine, it’s about the ritual of it, it’s a marker that separates my night from the day and tells my brain what gear to get into.
- Others may like to exercise first thing in the morning
- For still yet others, it could be a shower, cold or otherwise
- Some people like a tall glass of lemon water to rehydrate after sleeping!
- If you take drinkable morning supplements such as this pretty awesome nootropic stack, it’s a great time for that and an excellent way to get the brain-juices flowing!
- When you do get to productivity: eat the frog first! What this means is: if eating a frog is the hardest thing you’ll have to do all day, do that first. Basically, tackle the most intimidating task first. That way, you won’t spend your day stressed/anxious and/or subconsciously wasting time in order to procrastinate and avoid it.
- Counterpart to the above: a great idea is to also plan something to look forward to when your working day is done. It doesn’t matter much what it is, provided it’s rewarding to you, that makes you keen to finish your tasks to get to it.
Have a question you’d like to see answered here? Hit reply to this email, or use the feedback widget at the bottom! We always love to hear from you
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Four Ways To Upgrade The Mediterranean Diet
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Four Ways To Upgrade The Mediterranean Diet
The Mediterranean Diet is considered by many to be the current “gold standard” of healthy eating, and with good reason. With 10,000+ studies underpinning it and counting, it has a pretty hefty weight of evidence.
(For contrast, the Ketogenic Diet for example has under 5,000 studies at time of writing, and many of those include mentioning the problems with it. That’s not to say the Keto is without its merits! It certainly can help achieve some short term goals, but that’s a topic for another day)
Wondering what the Mediterranean Diet consists of? We outlined it in a previous main feature, so here it is for your convenience 😎
To get us started today, we’ll quickly drop some links to a few of those Mediterranean Diet studies from the top:
- Definition of the Mediterranean Diet; a Literature Review
- Mediterranean Diet In Healthy Aging
- Cancer and Mediterranean Diet: A Review
- Impact of Mediterranean Diet on Chronic Non-Communicable Diseases and Longevity
- Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies
- Adherence to Mediterranean diet and health status: meta-analysis
The short version is: it glows, in a good way.
The anti-inflammatory upgrade
One thing about the traditional Mediterranean Diet is… where are the spices?!
A diet focusing on fruits and non-starchy vegetables, healthy oils and minimal refined carbs, can be boosted by adding uses of spices such as chili, turmeric, cumin, fenugreek, and coriander:
The gut-healthy upgrade:
The Mediterranean Diet already gives for having a small amount of dairy, mostly in the form of cheeses, but this can be tweaked:
Mediterranean diet with extra dairy could be a gut gamechanger
The heart-healthy upgrade
The Mediterranean Diet is already highly recommended for heart health, and it offers different benefits to different parts of cardiovascular health:
The DASH (Dietary Approaches to Stop Hypertension) diet can boost it further, specifically in the category of, as the name suggests, lowering blood pressure.
It’s basically the Mediterranean Diet with a few tweaks. Most notably, red meat no longer features (the Mediterranean Diet allows for a small amount of red meat), and fish has gone up in the list:
Description of the DASH Eating Plan
The brain-healthy upgrade:
The MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay) diet combines several elements from the above, as the name suggests. It also adds extra portions of specific brain-foods, that already exist in the above diets, but get a more substantial weighting in this one:
MIND and Mediterranean diets linked to fewer signs of Alzheimer’s brain pathology
See also: The cognitive effects of the MIND diet
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
3 signs your diet is causing too much muscle loss – and what to do about it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When trying to lose weight, it’s natural to want to see quick results. So when the number on the scales drops rapidly, it seems like we’re on the right track.
But as with many things related to weight loss, there’s a flip side: rapid weight loss can result in a significant loss of muscle mass, as well as fat.
So how you can tell if you’re losing too much muscle and what can you do to prevent it?
EvMedvedeva/Shutterstock Why does muscle mass matter?
Muscle is an important factor in determining our metabolic rate: how much energy we burn at rest. This is determined by how much muscle and fat we have. Muscle is more metabolically active than fat, meaning it burns more calories.
When we diet to lose weight, we create a calorie deficit, where our bodies don’t get enough energy from the food we eat to meet our energy needs. Our bodies start breaking down our fat and muscle tissue for fuel.
A decrease in calorie-burning muscle mass slows our metabolism. This quickly slows the rate at which we lose weight and impacts our ability to maintain our weight long term.
How to tell you’re losing too much muscle
Unfortunately, measuring changes in muscle mass is not easy.
The most accurate tool is an enhanced form of X-ray called a dual-energy X-ray absorptiometry (DXA) scan. The scan is primarily used in medicine and research to capture data on weight, body fat, muscle mass and bone density.
But while DEXA is becoming more readily available at weight-loss clinics and gyms, it’s not cheap.
There are also many “smart” scales available for at home use that promise to provide an accurate reading of muscle mass percentage.
Some scales promise to tell us our muscle mass. Lee Charlie/Shutterstock However, the accuracy of these scales is questionable. Researchers found the scales tested massively over- or under-estimated fat and muscle mass.
Fortunately, there are three free but scientifically backed signs you may be losing too much muscle mass when you’re dieting.
1. You’re losing much more weight than expected each week
Losing a lot of weight rapidly is one of the early signs that your diet is too extreme and you’re losing too much muscle.
Rapid weight loss (of more than 1 kilogram per week) results in greater muscle mass loss than slow weight loss.
Slow weight loss better preserves muscle mass and often has the added benefit of greater fat mass loss.
One study compared people in the obese weight category who followed either a very low-calorie diet (500 calories per day) for five weeks or a low-calorie diet (1,250 calories per day) for 12 weeks. While both groups lost similar amounts of weight, participants following the very low-calorie diet (500 calories per day) for five weeks lost significantly more muscle mass.
2. You’re feeling tired and things feel more difficult
It sounds obvious, but feeling tired, sluggish and finding it hard to complete physical activities, such as working out or doing jobs around the house, is another strong signal you’re losing muscle.
Research shows a decrease in muscle mass may negatively impact your body’s physical performance.
3. You’re feeling moody
Mood swings and feeling anxious, stressed or depressed may also be signs you’re losing muscle mass.
Research on muscle loss due to ageing suggests low levels of muscle mass can negatively impact mental health and mood. This seems to stem from the relationship between low muscle mass and proteins called neurotrophins, which help regulate mood and feelings of wellbeing.
So how you can do to maintain muscle during weight loss?
Fortunately, there are also three actions you can take to maintain muscle mass when you’re following a calorie-restricted diet to lose weight.
1. Incorporate strength training into your exercise plan
While a broad exercise program is important to support overall weight loss, strength-building exercises are a surefire way to help prevent the loss of muscle mass. A meta-analysis of studies of older people with obesity found resistance training was able to prevent almost 100% of muscle loss from calorie restriction.
Relying on diet alone to lose weight will reduce muscle along with body fat, slowing your metabolism. So it’s essential to make sure you’ve incorporated sufficient and appropriate exercise into your weight-loss plan to hold onto your muscle mass stores.
Strength-building exercises help you retain muscle. BearFotos/Shutterstock But you don’t need to hit the gym. Exercises using body weight – such as push-ups, pull-ups, planks and air squats – are just as effective as lifting weights and using strength-building equipment.
Encouragingly, moderate-volume resistance training (three sets of ten repetitions for eight exercises) can be as effective as high-volume training (five sets of ten repetitions for eight exercises) for maintaining muscle when you’re following a calorie-restricted diet.
2. Eat more protein
Foods high in protein play an essential role in building and maintaining muscle mass, but research also shows these foods help prevent muscle loss when you’re following a calorie-restricted diet.
But this doesn’t mean just eating foods with protein. Meals need to be balanced and include a source of protein, wholegrain carb and healthy fat to meet our dietary needs. For example, eggs on wholegrain toast with avocado.
3. Slow your weight loss plan down
When we change our diet to lose weight, we take our body out of its comfort zone and trigger its survival response. It then counteracts weight loss, triggering several physiological responses to defend our body weight and “survive” starvation.
Our body’s survival mechanisms want us to regain lost weight to ensure we survive the next period of famine (dieting). Research shows that more than half of the weight lost by participants is regained within two years, and more than 80% of lost weight is regained within five years.
However, a slow and steady, stepped approach to weight loss, prevents our bodies from activating defence mechanisms to defend our weight when we try to lose weight.
Ultimately, losing weight long-term comes down to making gradual changes to your lifestyle to ensure you form habits that last a lifetime.
At the Boden Group, Charles Perkins Centre, we are studying the science of obesity and running clinical trials for weight loss. You can register here to express your interest.
Nick Fuller, Charles Perkins Centre Research Program Leader, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: