Mythbusting Cookware Materials
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
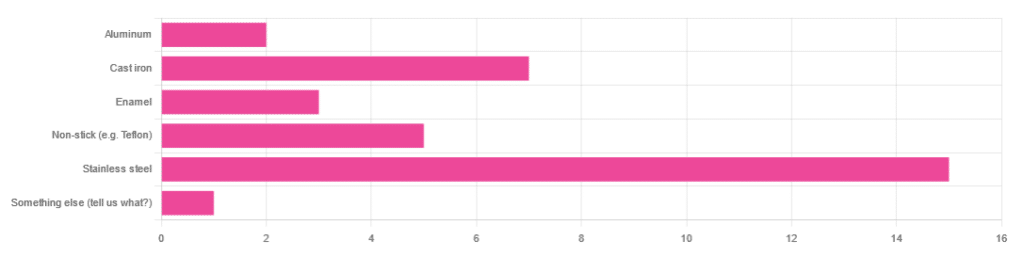
In Wednesday’s newsletter, we asked you what kind of cookware you mostly use, and got the above-depicted, below-described, set of responses:
- About 45% said stainless steel
- About 21% said cast iron
- About 15% said non-stick (e.g. Teflon)
- About 9% said enamel
- About 6% said aluminum
- And 1 person selected “something else”, but then commented to the contrary, writing “I use all of the above”
So, what does the science say about these options?
Stainless steel cookware is safe: True or False?
True! Assuming good quality and normal use, anyway. There really isn’t a lot to say about this, because it’s very unexciting. So long as it is what it is labelled as: there’s nothing coating it, nothing comes out of it unless you go to extremes*, and it’s easy to clean.
*If you cook for long durations at very high temperatures, it can leach nickel and chromium into food. What this means in practical terms: if you are using stainless steel to do deep-frying, then maybe stop that, and also consider going easy on deep-frying in general anyway, because obviously deep-frying is unhealthy for other reasons.
Per normal use, however: pretty much the only way (good quality) stainless steel cookware will harm you is if you touch it while it’s hot, or if it falls off a shelf onto your head.
That said, do watch out for cheap stainless steel cookware that can contain a lot of impurities, including heavy metals. Since you probably don’t have a mass spectrometer and/or chemistry lab at home to check for those impurities, your best guard here is simply to buy from a reputable brand with credible certifications.
Ceramic cookware is safe: True or False?
True… Most of the time! Ceramic pans usually have metal parts and a ceramic cooking surface coated with a very thin layer of silicon. Those metal parts will be as safe as the metals used, so if that’s stainless steel, you’re just as safe as the above. As for the silicon, it is famously inert and body-safe (which is why it’s used in body implants).
However: ceramic cookware that doesn’t have an obvious metal part and is marketed as being pure ceramic, will generally be sealed with some kind of glaze that can leach heavy metals contaminants into the food; here’s an example:
Lead toxicity from glazed ceramic cookware
Copper cookware is safe: True or False?
False! This is one we forgot to mention in the poll, as one doesn’t see a lot of it nowadays. The copper from copper pans can leach into food. Now, of course copper is an important mineral that we must get from our diet, but the amount of copper that that can leach into food from copper pans is far too much, and can induce copper toxicity.
In addition, copper cookware has been found to be, on average, highly contaminated with lead:
Non-stick cookware contaminates the food with microplastics: True or False?
True! If we were to discuss all the common non-stick contaminants here, this email would no longer fit (there’s a size limit before it gets clipped by most email services).
Suffice it to say: the non-stick coating, polytetrafluoroethylene, is itself a PFAS, that is to say, part of the category of chemicals considered environmental pollutants, and associated with a long list of health issues in humans (wherein the level of PFAS in our bloodstream is associated with higher incidence of many illnesses):
You may have noticed, of course, that the “non-stick” coating doesn’t stick very well to the pan, either, and will tend to come off over time, even if used carefully.
Also, any kind of wet cooking (e.g. saucepans, skillets, rice cooker inserts) will leach PFAS into the food. In contrast, a non-stick baking tray lined with baking paper (thus: a barrier between the tray and your food) is really not such an issue.
We wrote about PFAS before, so if you’d like a more readable pop-science article than the scientific paper above, then check out:
PFAS Exposure & Cancer: The Numbers Are High
Aluminum cookware contaminates the food with aluminum: True or False?
True! But not usually in sufficient quantities to induce aluminum toxicity, unless you are aluminum pans Georg who eats half a gram of aluminum per day, who is a statistical outlier and should not be counted.
That’s a silly example, but an actual number; the dose required for aluminum toxicity in blood is 100mg/L, and you have about 5 liters of blood.
Unless you are on kidney dialysis (because 95% of aluminum is excreted by the kidneys, and kidney dialysis solution can itself contain aluminum), you will excrete aluminum a lot faster than you can possibly absorb it from cookware. On the other hand, you can get too much of it from it being a permitted additive in foods and medications, for example if you are taking antacids they often have a lot of aluminum oxide in them—but that is outside the scope of today’s article.
However, aluminum may not be the real problem in aluminum pans:
❝In addition, aluminum (3.2 ± 0.25 to 4.64 ± 0.20 g/kg) and copper cookware (2.90 ± 0.12 g/kg) were highly contaminated with lead.
The time and pH-dependent study revealed that leaching of metals (Al, Pb, Ni, Cr, Cd, Cu, and Fe, etc.) into food was predominantly from anodized and non-anodized aluminum cookware.
More metal leaching was observed from new aluminum cookware compared to old. Acidic food was found to cause more metals to leach during cooking.❞
~ the same paper we cited when talking about copper
Cast iron cookware contaminates the food with iron: True or False?
True, but unlike with the other metals discussed, this is purely a positive, and indeed, it’s even recommended as a good way to fortify one’s diet with iron:
The only notable counterpoint we could find for this is if you have hemochromatosis, a disorder in which the body is too good at absorbing iron and holding onto it.
Thinking of getting some new cookware?
Here are some example products of high-quality safe materials on Amazon, but of course feel free to shop around:
Stainless Steel | Ceramic* | Cast Iron
*it says “non-stick” in the description, but don’t worry, it’s ceramic, not Teflon etc, and is safe
Bonus: rice cooker with stainless steel inner pot
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is pathological demand avoidance – and how is it different to ‘acting out’?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Charlie” is an eight-year-old child with autism. Her parents are worried because she often responds to requests with insults, aggression and refusal. Simple demands, such as being asked to get dressed, can trigger an intense need to control the situation, fights and meltdowns.
Charlie’s parents find themselves in a constant cycle of conflict, trying to manage her and their own reactions, often unsuccessfully. Their attempts to provide structure and consequences are met with more resistance.
What’s going on? What makes Charlie’s behaviour – that some are calling “pathological demand avoidance” – different to the defiance most children show their parents or carers from time-to-time?
What is pathological demand avoidance?
British developmental psychologist Elizabeth Newson coined the term “pathological demand avoidance” (commonly shortened to PDA) in the 1980s after studying groups of children in her practice.
A 2021 systematic review noted features of PDA include resistance to everyday requests and strong emotional and behavioural reactions.
Children with PDA might show obsessive behaviour, struggle with persistence, and seek to control situations. They may struggle with attention and impulsivity, alongside motor and coordination difficulties, language delay and a tendency to retreat into role play or fantasy worlds.
PDA is also known as “extreme demand avoidance” and is often described as a subtype of autism. Some people prefer the term persistent drive for autonomy or pervasive drive for autonomy.
What does the evidence say?
Every clinician working with children and families recognises the behavioural profile described by PDA. The challenging question is why these behaviours emerge.
PDA is not currently listed in the two diagnostic manuals used in psychiatry and psychology to diagnose mental health and developmental conditions, the current Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the World Health Organization’s International Classification of Diseases (ICD-11).
Researchers have reported concerns about the science behind PDA. There are no clear theories or explanations of why or how the profile of symptoms develop, and little inclusion of children or adults with lived experience of PDA symptoms in the studies. Environmental, family or other contextual factors that may contribute to behaviour have not been systematically studied.
A major limitation of existing PDA research and case studies is a lack of consideration of overlapping symptoms with other conditions, such as autism, attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder, anxiety disorder, selective mutism and other developmental disorders. Diagnostic labels can have positive and negative consequences and so need to be thoroughly investigated before they are used in practice.
Classifying a “new” condition requires consistency across seven clinical and research aspects: epidemiological data, long-term patient follow-up, family inheritance, laboratory findings, exclusion from other conditions, response to treatment, and distinct predictors of outcome. At this stage, these domains have not been established for PDA. It is not clear whether PDA is different from other formal diagnoses or developmental differences.
When a child is stressed, demands or requests might tip them into fight, flight or freeze mode. Shutterstock Finding the why
Debates over classification don’t relieve distress for a child or those close to them. If a child is “intentionally” engaged in antisocial behaviour, the question is then “why?”
Beneath the behaviour is almost always developmental difference, genuine distress and difficulty coping. A broad and deep understanding of developmental processes is required.
Interestingly, while girls are “under-represented” in autism research, they are equally represented in studies characterising PDA. But if a child’s behaviour is only understood through a “pathologising” or diagnostic lens, there is a risk their agency may be reduced. Underlying experiences of distress, sensory overload, social confusion and feelings of isolation may be missed.
So, what can be done to help?
There are no empirical studies to date regarding PDA treatment strategies or their effectiveness. Clinical advice and case studies suggest strategies that may help include:
- reducing demands
- giving multiple options
- minimising expectations to avoid triggering avoidance
- engaging with interests to support regulation.
Early intervention in the preschool and primary years benefits children with complex developmental differences. Clinical care that involves a range of medical and allied health clinicians and considers the whole person is needed to ensure children and families get the support they need.
It is important to recognise these children often feel as frustrated and helpless as their caregivers. Both find themselves stuck in a repetitive cycle of distress, frustration and lack of progress. A personalised approach can take into account the child’s unique social, sensory and cognitive sensitivities.
In the preschool and early primary years, children have limited ability to manage their impulses or learn techniques for managing their emotions, relationships or environments. Careful watching for potential triggers and then working on timetables and routines, sleep, environments, tasks, and relationships can help.
As children move into later primary school and adolescence, they are more likely to want to influence others and be able to have more self control. As their autonomy and ability to collaborate increases, the problematic behaviours tend to reduce.
Strategies that build self-determination are crucial. They include opportunities for developing confidence, communication and more options to choose from when facing challenges. This therapeutic work with children and families takes time and needs to be revisited at different developmental stages. Support to engage in school and community activities is also needed. Each small step brings more capacity and more effective ways for a child to understand and manage themselves and their worlds.
What about Charlie?
The current scope to explain and manage PDA is limited. Future research must include the voices and views of children and adults with PDA symptoms.
Such emotional and behavioural difficulties are distressing and difficult for children and families. They need compassion and practical help.
For a child like Charlie, this could look like a series of sessions where she and her parents meet with clinicians to explore Charlie’s perspective, experiences and triggers. The family might come to understand that, in addition to autism, Charlie has complex developmental strengths and challenges, anxiety, and some difficulties with adjustment related to stress at home and school. This means Charlie experiences a fight, flight, freeze response that looks like aggression, avoidance or shutting down.
With carefully planned supports at home and school, Charlie’s options can broaden and her distress and avoidance can soften. Outside the clinic room, Charlie and her family can be supported to join an inclusive local community sporting or creative activity. Gradually she can spend more time engaged at home, school and in the community.
Nicole Rinehart, Professor, Child and Adolescent Psychology, Director, Krongold Clinic (Research), Monash University; David Moseley, Senior Research Fellow, Deputy Director (Clinical), Monash Krongold Clinic, Monash University, and Michael Gordon, Associate Professor, Psychiatry, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
30 Days Of Weight Vest Use: Lessons Learned
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Robin, from “The Science of Self-Care”, has insights:
How to have an easier time of it
Per peer-reviewed science (linked under the video on YouTube), there are some benefits:
- Cardiovascular fitness: increases workout intensity, improving heart and lung health.
- Muscle strength & endurance: strengthens core, legs, glutes, and calves.
- Bone density: helps prevent osteoporosis through weight-bearing exercise.
- Caloric expenditure: burns more calories, aiding in weight loss.
- Balance & posture: improves balance, though posture effects were mixed.
She chose a 30 lb weighted vest, which felt much heavier than expected. Initially, this was uncomfortable but became comforting over time (much like a weighted blanket). She also found that walks became noticeably more intense, leading to increased sweating and hunger.
Over the course of the month, she found:
- Week 1: adjusting to the extra weight; walks felt significantly harder.
- Weeks 2-3: strength improvements; carrying groceries felt easier, walking without the vest felt effortless.
- Week 3: started craving the weighted vest, but also began experiencing shoulder discomfort.
- Week 4: reduced walk duration to 20 minutes due to shoulder strain.
She concluded that the vest design was flawed—all weight rested on shoulders instead of distributing across the body, which led to shoulder discomfort and posture issues. To mitigate these things, she switched to wearing the vest around the waist like a skirt. She now plans to try a weighted belt for better weight distribution, though also simply a different kind of vest would work better (the kind that looks like combat body armor distributes the weight a lot more easily)
In short, her verdict:
- Weighted walking: 10/10, highly beneficial and easy to incorporate into daily routines.
- Vest used: 2/10, poor weight distribution, causing discomfort and shoulder strain.
For more on all of this, plus links to the relevant scientific papers, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Weight Vests Against Osteoporosis: Do They Really Build Bone?
Take care!
Share This Post
-
You’ve Got Questions? We’ve Got Answers!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From Cucumbers To Kindles
Q: Where do I get cucumber extract?
A: You can buy it from BulkSupplements.com (who, despite their name, start at 100g packs)
Alternatively: you want it as a topical ointment (for skin health) rather than as a dietary supplement (for bone and joint health), you can extract it yourself! No, it’s not “just juice cucumbers”, but it’s also not too tricky.
Click Here For A Quick How-To Guide!
Q: Tips for reading more and managing time for it?
A: We talked about this a little bit in yesterday’s edition, so you may have seen that, but aside from that:
- If you don’t already have one, consider getting a Kindle or similar e-reader. They’re very convenient, and also very light and ergonomic—no more wrist strain as can occur with physical books. No more eye-strain, either!
- Consider making reading a specific part of your daily routine. A chapter before bed can be a nice wind-down, for instance! What’s important is it’s a part of your day that’ll always, or at least almost always, allow you to do a little reading.
- If you drive, walk, run, or similar each day, a lot of people find that’s a great time to listen to an audiobook. Please be safe, though!
- If your lifestyle permits such, a “reading retreat” can be a wonderful vacation! Even if you only “retreat” to your bedroom, the point is that it’s a weekend (or more!) that you block off from all other commitments, and curl up with the book(s) of your choice.
Q: Any study tips as we approach exam season? A lot of the productivity stuff is based on working life, but I can’t be the only student!
A: We’ve got you covered:
- Be passionate about your subject! We know of no greater study tip than that.
- Find a willing person and lecture them on your subject. When one teaches, two learn!
- Your mileage may vary depending on your subject, but, find a way of studying that’s fun to you!
- If you can get past papers, get as many as you can, and use those as your “last minute” studying in the week before your exam(s). This will prime you for answering exam-style questions (and leverage state-dependent memory). As a bonus, it’ll also help ease any anxiety, because by the time of your exam it’ll be “same old, same old”!
Q: Energy drinks for biohacking, yea or nay?
A: This is definitely one of those “the dose makes the poison” things!
- Caffeine, in and of itself, can be healthy in moderation for most people.
- Taurine has assorted benefits at safe dosages:
- Other ingredients often have health benefits too.
But… The generally agreed safe dose of taurine is around 3g/day for most people; a standard Red Bull contains 1g.
That math would be simple, but… if you eat meat (including poultry or fish), that can also contain 10–950mg per 100g. For example, tuna is at the high end of that scale, with a standard 12oz (340g) tin already containing up to 3.23g of taurine!
And sweetened carbonated beverages in general have so many health issues that it’d take us a full article to cover them.
Short version? Enjoy in moderation if you must, but there are definitely better ways of getting the benefits they may offer.
Q: Best morning routine?
A: The best morning routine is whatever makes you feel most ready to take on your day!
This one’s going to vary a lot—one person’s morning run could be another person’s morning coffee and newspaper, for example.
In a nutshell, though, ask yourself these questions:
- How long does it take me to fully wake up in the morning, and what helps or hinders that?
- When I get out of bed, what do I really need before I can take on my day?
- If I could have the perfect morning, what would it look like?
- What can evening me do, to look after morning me’s best interests? (Semi-prepare breakfast ready? Lay out clothes ready? Running shoes? To-Do list?)
Q: I’m curious how much of these things you actually use yourselves, and are there any disagreements in the team? In a lot of places things can get pretty heated when it’s paleo vs vegan / health benefits of tea/coffee vs caffeine-abstainers / you need this much sleep vs rise and grinders, etc?
A: We are indeed genuinely enthusiastic about health and productivity, and that definitely includes our own! We may or may not all do everything, but between us, we probably have it all covered. As for disagreements, we’ve not done a survey, but if you take an evidence-based approach, any conflict will tend to be minimized. Plus, sometimes you can have the best of both!
- You could have a vegan paleo diet (you’d better love coconut if you do, though!
- There is decaffeinated coffee and tea (your taste may vary)
- You can get plenty of sleep and rise early (so long as an “early to bed, early to rise” schedule suits you!)
Interesting note: humans are social creatures on an evolutionary level. Evolution has resulted in half of us being “night owls” and the other half “morning larks”, the better to keep each other safe while sleeping. Alas, modern life doesn’t always allow us to have the sleep schedule that’d suit each of us best individually!
Have a question you’d like answered? Reply to this email, or use the feedback widget at the bottom! We always love to hear from you
Share This Post
Related Posts
-
Measles cases are rising—here’s how to protect your family
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The U.S. is currently experiencing a spike in measles cases across several states. Measles a highly contagious and potentially life-threatening disease caused by a virus. The measles-mumps-rubella (MMR) vaccine prevents measles; unvaccinated people put themselves and everyone around them at risk, including babies who are too young to receive the vaccine.
Read on to learn more about measles: what it is, how to stay protected, and what to do if a measles outbreak happens near you.
What are the symptoms of measles?
Measles symptoms typically begin 10 to 14 days after exposure. The disease starts with a fever followed by a cough, runny nose, and red eyes and then produces a rash of tiny red spots on the face and body. Measles can affect anyone, but is most serious for children under 5, immunocompromised people, and pregnant people, who may give birth prematurely or whose babies may have low birth weight as a result of a measles infection.
Measles isn’t just a rash—the disease can cause serious health problems and even death. About one in five unvaccinated people in the U.S. who get measles will be hospitalized and could suffer from pneumonia, dehydration, or brain swelling.
If you get measles, it can also damage your immune system, making you more vulnerable to other diseases.
How do you catch measles?
Measles spreads through the air when an infected person coughs or sneezes. It’s so contagious that unvaccinated people have a 90 percent chance of becoming infected if exposed.
An infected person can spread measles to others before they have symptoms.
Why are measles outbreaks happening now?
The pandemic caused many children to miss out on routine vaccinations, including the MMR vaccine. Delayed vaccination schedules coincided with declining confidence in vaccine safety and growing resistance to vaccine requirements.
Skepticism about the safety and effectiveness of COVID-19 vaccines has resulted in some people questioning or opposing the MMR vaccine and other routine immunizations.
How do I protect myself and my family from measles?
Getting an MMR vaccine is the best way to prevent getting sick with measles or spreading it to others. The CDC recommends that children receive the MMR vaccine at 12 to 15 months and again at 4 to 6 years, before starting kindergarten.
One dose of the MMR vaccine provides 93 percent protection and two doses provide 97 percent protection against all strains of measles. Because some children are too young to be immunized, it’s important that those around them are vaccinated to protect them.
Is the MMR vaccine safe?
The MMR vaccine has been rigorously tested and monitored over 50 years and determined to be safe. Adverse reactions to the vaccine are extremely rare.
Receiving the MMR vaccine is much safer than contracting measles.
What do I do if there’s a measles outbreak in my community?
Anyone who is not fully vaccinated for measles should be immunized with a measles vaccine as soon as possible. Measles vaccines given within 72 hours after exposure may prevent or reduce the severity of disease.
Children as young as 6 months old can receive the MMR vaccine if they are at risk during an outbreak. If your child isn’t fully vaccinated with two doses of the MMR vaccine—or three doses, if your child received the first dose before their first birthday—talk to your pediatrician.
Unvaccinated people who have been exposed to the virus should stay home from work, school, day care, and other activities for 21 days to avoid spreading the disease.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
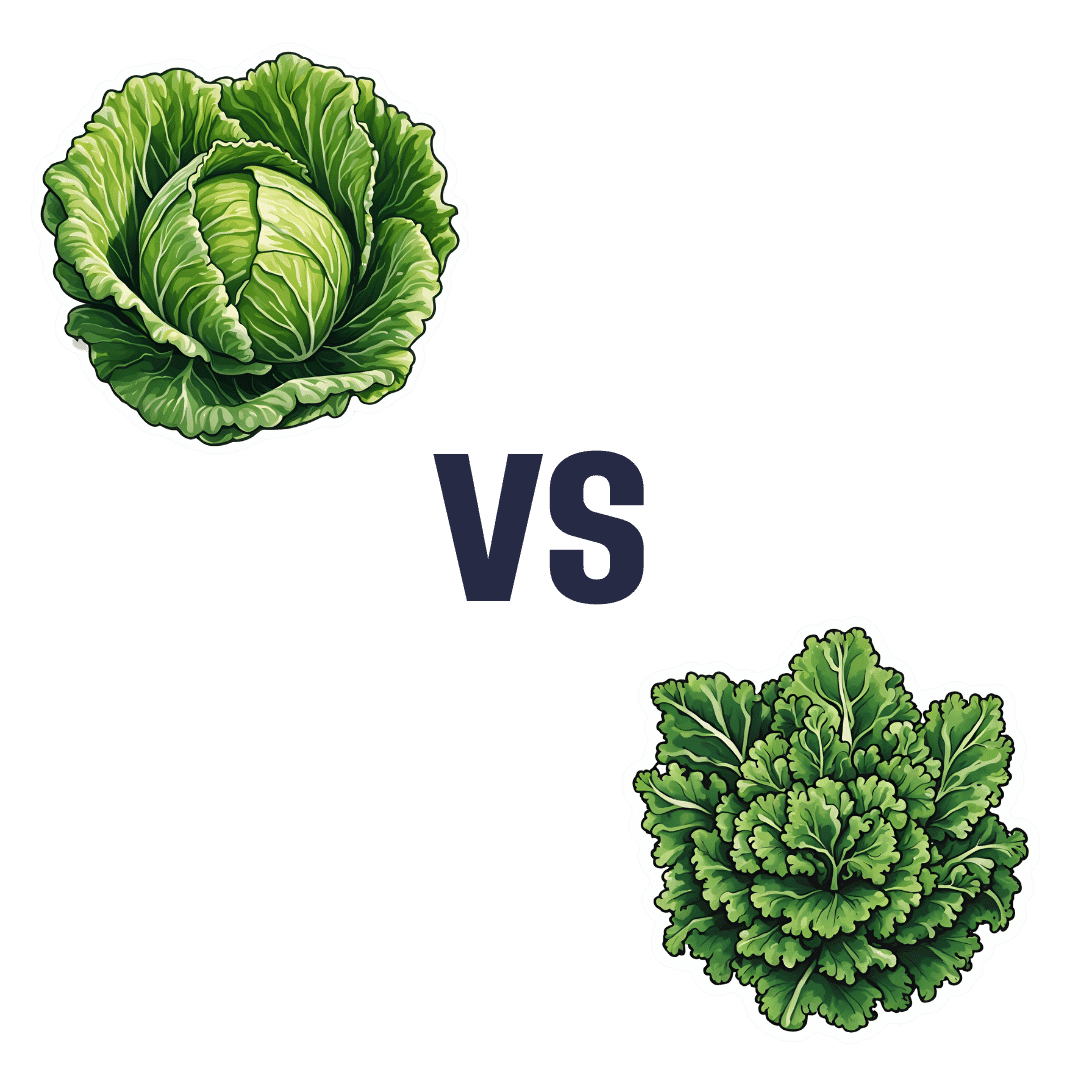
Cabbage vs Kale – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cabbage to kale, we picked the kale.
Why?
Here we go again, pitting Brassica oleracea vs Brassica oleracea. One species, many cultivars! Notwithstanding being the same species, there are important nutritional differences:
In terms of macros, kale has more protein, carbs, and fiber, and even has the lower glycemic index, not that cabbage is bad at all, of course. But nominally, kale gets the win on all counts in this category.
In the category of vitamins, cabbage has more of vitamins B5 and choline, while kale has more of vitamins A, B1, B2, B3, B6, B7, B9, C, E, and K. An easy win for kale!
When it comes to minerals, it’s even more decisive: cabbage is not higher in any minerals, while kale has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. Another clear win for kale.
Adding up the sections makes it very clear that kale wins the day, but we’d like to mention that cabbage was good in all of these metrics too; kale was just better!
Want to learn more?
You might like to read:
21 Most Beneficial Polyphenols & What Foods Have Them
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s Your Ikigai?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ikigai: A Closer Look
We’ve mentioned ikigai from time to time, usually when discussing the characteristics associated with Blue Zone centenarians, for example as number 5 of…
It’s about finding one’s “purpose”. Not merely a function, but what actually drives you in life. And, if Japanese studies can be extrapolated to the rest of the world, it has a significant and large impact on mortality (other factors being controlled for); not having a sense of ikigai is associated with an approximately 47%* increase in 7-year mortality risk in the categories of cardiovascular disease and external cause mortality:
Sense of life worth living (ikigai) and mortality in Japan: Ohsaki Study
*we did a lot of averaging and fuzzy math to get this figure; the link will show you the full stats though!
In case that huge (n=43,391) study didn’t convince you, here’s another comparably-sized (n=43,117) one that found similarly, albeit framing the numbers the other way around, i.e. a comparable decrease in mortality risk for having a sense of ikigai:
This study was even longer (12 years rather than 7), so the fact that it found pretty much the same results the 7-year study we cited just before is quite compelling evidence. Again, multivariate hazard ratios were adjusted for age, BMI, drinking and smoking status, physical activity, sleep duration, education, occupation, marital status, perceived mental stress, and medical history—so all these things were effectively controlled for statistically.
Three kinds of ikigai
There are three principal kinds of ikigai:
- Social ikigai: for example, a caring role in the family or community, volunteer work, teaching
- Asocial ikigai: for example, a solitary practice of self-discipline, spirituality, or study without any particular intent to teach others
- Antisocial ikigai: for example, a strong desire to outlive an enemy, or to harm a person or group that one hates
You may be thinking: wait, aren’t those last things bad?
And… Maybe! But ikigai is not a matter of morality or even about “warm fuzzy feelings”. The fact is, having a sense of purpose increases longevity regardless of moral implications or niceness.
Nevertheless, for obvious reasons there is a lot more focus on the first two categories (social and asocial), and of those, especially the first category (social), because on a social level, “we all do well when we all do well”.
We exemplified them above, but they can be defined:
- Social: working for the betterment of society
- Asocial: working for the betterment of oneself
Of course, for many people, the same ikigai may cover both of those—often somebody who excels at something for its own sake and/but shares it with others to enrich their lives also, for example a teacher, an artist, a scientist, etc.
For it to cover both, however, requires that both parts of it are genuinely part of their feeling of ikigai, and not merely unintended consequences.
For example, a piano teacher who loves music in general and the piano in particular, and would gladly spend every waking moment studying/practising/performing, but hates having to teach it, but needs to pay the bills so teaches it anyway, cannot be said to be living any kind of social ikigai there, just asocial. And in fact, if teaching the piano is causing them to not have the time or energy to pursue it for its own sake, they might not even be living any ikigai at all.
One other thing to watch out for
There is one last stumbling block, which is that while we can find ikigai, we can also lose it! Examples of this may include:
- A professional whose job is their ikigai, until they face mandatory retirement or are otherwise unable to continue their work (perhaps due to disability, for example)
- A parent whose full-time-parent role is their ikigai, until their children leave for school, university, life in general
- A married person whose “devoted spouse” role is their ikigai, until their partner dies
For this reason, people of any age can have a “crisis of identity” that’s actually more of a “crisis of purpose”.
There are two ways of handling this:
- Have a back-up ikigai ready! For example, if your profession is your ikigai, maybe you have a hobby waiting in the wings, that you can smoothly jump ship to upon retirement.
- Embrace the fluidity of life! Sometimes, things don’t happen the way we expect. Sometimes life’s surprises can trip us up; sometimes they can leave us a sobbing wreck. But so long as life continues, there is an opportunity to pick ourselves up and decide where to go from that point. Note that this is not fatalism, by the way, it doesn’t have to be “this bad thing happened so that we could find this good thing, so really it was a good thing all along”. Rather, it can equally readily be “well, we absolutely did not want that bad thing to happen, but since it did, now we shall take it this way from here”.
For more on developing/maintaining psychological resilience in the face of life’s less welcome adversities, see:
Psychological Resilience Training
…and:
Putting The Abs Into Absurdity ← do not underestimate the power of this one
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: