You’ve Got Questions? We’ve Got Answers!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From Cucumbers To Kindles
Q: Where do I get cucumber extract?
A: You can buy it from BulkSupplements.com (who, despite their name, start at 100g packs)
Alternatively: you want it as a topical ointment (for skin health) rather than as a dietary supplement (for bone and joint health), you can extract it yourself! No, it’s not “just juice cucumbers”, but it’s also not too tricky.
Click Here For A Quick How-To Guide!
Q: Tips for reading more and managing time for it?
A: We talked about this a little bit in yesterday’s edition, so you may have seen that, but aside from that:
- If you don’t already have one, consider getting a Kindle or similar e-reader. They’re very convenient, and also very light and ergonomic—no more wrist strain as can occur with physical books. No more eye-strain, either!
- Consider making reading a specific part of your daily routine. A chapter before bed can be a nice wind-down, for instance! What’s important is it’s a part of your day that’ll always, or at least almost always, allow you to do a little reading.
- If you drive, walk, run, or similar each day, a lot of people find that’s a great time to listen to an audiobook. Please be safe, though!
- If your lifestyle permits such, a “reading retreat” can be a wonderful vacation! Even if you only “retreat” to your bedroom, the point is that it’s a weekend (or more!) that you block off from all other commitments, and curl up with the book(s) of your choice.
Q: Any study tips as we approach exam season? A lot of the productivity stuff is based on working life, but I can’t be the only student!
A: We’ve got you covered:
- Be passionate about your subject! We know of no greater study tip than that.
- Find a willing person and lecture them on your subject. When one teaches, two learn!
- Your mileage may vary depending on your subject, but, find a way of studying that’s fun to you!
- If you can get past papers, get as many as you can, and use those as your “last minute” studying in the week before your exam(s). This will prime you for answering exam-style questions (and leverage state-dependent memory). As a bonus, it’ll also help ease any anxiety, because by the time of your exam it’ll be “same old, same old”!
Q: Energy drinks for biohacking, yea or nay?
A: This is definitely one of those “the dose makes the poison” things!
- Caffeine, in and of itself, can be healthy in moderation for most people.
- Taurine has assorted benefits at safe dosages:
- Other ingredients often have health benefits too.
But… The generally agreed safe dose of taurine is around 3g/day for most people; a standard Red Bull contains 1g.
That math would be simple, but… if you eat meat (including poultry or fish), that can also contain 10–950mg per 100g. For example, tuna is at the high end of that scale, with a standard 12oz (340g) tin already containing up to 3.23g of taurine!
And sweetened carbonated beverages in general have so many health issues that it’d take us a full article to cover them.
Short version? Enjoy in moderation if you must, but there are definitely better ways of getting the benefits they may offer.
Q: Best morning routine?
A: The best morning routine is whatever makes you feel most ready to take on your day!
This one’s going to vary a lot—one person’s morning run could be another person’s morning coffee and newspaper, for example.
In a nutshell, though, ask yourself these questions:
- How long does it take me to fully wake up in the morning, and what helps or hinders that?
- When I get out of bed, what do I really need before I can take on my day?
- If I could have the perfect morning, what would it look like?
- What can evening me do, to look after morning me’s best interests? (Semi-prepare breakfast ready? Lay out clothes ready? Running shoes? To-Do list?)
Q: I’m curious how much of these things you actually use yourselves, and are there any disagreements in the team? In a lot of places things can get pretty heated when it’s paleo vs vegan / health benefits of tea/coffee vs caffeine-abstainers / you need this much sleep vs rise and grinders, etc?
A: We are indeed genuinely enthusiastic about health and productivity, and that definitely includes our own! We may or may not all do everything, but between us, we probably have it all covered. As for disagreements, we’ve not done a survey, but if you take an evidence-based approach, any conflict will tend to be minimized. Plus, sometimes you can have the best of both!
- You could have a vegan paleo diet (you’d better love coconut if you do, though!
- There is decaffeinated coffee and tea (your taste may vary)
- You can get plenty of sleep and rise early (so long as an “early to bed, early to rise” schedule suits you!)
Interesting note: humans are social creatures on an evolutionary level. Evolution has resulted in half of us being “night owls” and the other half “morning larks”, the better to keep each other safe while sleeping. Alas, modern life doesn’t always allow us to have the sleep schedule that’d suit each of us best individually!
Have a question you’d like answered? Reply to this email, or use the feedback widget at the bottom! We always love to hear from you
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

The Path To Revenue – by Theresa Marcroft
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So many books about start-ups skip right over the elephant in the room: survivorship bias. Not so for Marcroft! This book contains the most comprehensive and unapologetic treatment of it we’ve seen.
Less “here’s what Steve Jobs did right and here’s what Chocolate-Teapots-For-Dogs-R-Us did wrong; don’t mess up that badly and you’ll be fine”… and more realism. Marcroft gives us a many-angled critical analytic approach. In it, she examines why many things can seem similar in both content and presentation… but can cause growth or failure (and how and why), based on more than anecdotes and luck.
The book is information-dense (taking a marketing-centric approach) and/but well-presented in a very readable format.
If we can find any criticism of the book, it’s less about what’s in it and more about what’s not in it. This can never be a “your start-up bible!” book because it’s not comprehensive. It doesn’t cover assembling your team, for example. Nor does it give a lot of attention to management, preferring to focus on strategy.
But no single book can be all things, and we highly recommend this one—the marketing advice alone is more than worth the cost of the book!
Take Your First Step Along The Path To Revenue By Checking It Out On Amazon!
Share This Post

People with dementia aren’t currently eligible for voluntary assisted dying. Should they be?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dementia is the second leading cause of death for Australians aged over 65. More than 421,000 Australians currently live with dementia and this figure is expected to almost double in the next 30 years.
There is ongoing public discussion about whether dementia should be a qualifying illness under Australian voluntary assisted dying laws. Voluntary assisted dying is now lawful in all six states, but is not available for a person living with dementia.
The Australian Capital Territory has begun debating its voluntary assisted dying bill in parliament but the government has ruled out access for dementia. Its view is that a person should retain decision-making capacity throughout the process. But the bill includes a requirement to revisit the issue in three years.
The Northern Territory is also considering reform and has invited views on access to voluntary assisted dying for dementia.
Several public figures have also entered the debate. Most recently, former Australian Chief Scientist, Ian Chubb, called for the law to be widened to allow access.
Others argue permitting voluntary assisted dying for dementia would present unacceptable risks to this vulnerable group.

Inside Creative House/Shutterstock Australian laws exclude access for dementia
Current Australian voluntary assisted dying laws exclude access for people who seek to qualify because they have dementia.
In New South Wales, the law specifically states this.
In the other states, this occurs through a combination of the eligibility criteria: a person whose dementia is so advanced that they are likely to die within the 12 month timeframe would be highly unlikely to retain the necessary decision-making capacity to request voluntary assisted dying.
This does not mean people who have dementia cannot access voluntary assisted dying if they also have a terminal illness. For example, a person who retains decision-making capacity in the early stages of Alzheimer’s disease with terminal cancer may access voluntary assisted dying.
What happens internationally?
Voluntary assisted dying laws in some other countries allow access for people living with dementia.
One mechanism, used in the Netherlands, is through advance directives or advance requests. This means a person can specify in advance the conditions under which they would want to have voluntary assisted dying when they no longer have decision-making capacity. This approach depends on the person’s family identifying when those conditions have been satisfied, generally in consultation with the person’s doctor.
Another approach to accessing voluntary assisted dying is to allow a person with dementia to choose to access it while they still have capacity. This involves regularly assessing capacity so that just before the person is predicted to lose the ability to make a decision about voluntary assisted dying, they can seek assistance to die. In Canada, this has been referred to as the “ten minutes to midnight” approach.
But these approaches have challenges
International experience reveals these approaches have limitations. For advance directives, it can be difficult to specify the conditions for activating the advance directive accurately. It also requires a family member to initiate this with the doctor. Evidence also shows doctors are reluctant to act on advance directives.
Particularly challenging are scenarios where a person with dementia who requested voluntary assisted dying in an advance directive later appears happy and content, or no longer expresses a desire to access voluntary assisted dying.

What if the person changes their mind? Jokiewalker/Shutterstock Allowing access for people with dementia who retain decision-making capacity also has practical problems. Despite regular assessments, a person may lose capacity in between them, meaning they miss the window before midnight to choose voluntary assisted dying. These capacity assessments can also be very complex.
Also, under this approach, a person is required to make such a decision at an early stage in their illness and may lose years of otherwise enjoyable life.
Some also argue that regardless of the approach taken, allowing access to voluntary assisted dying would involve unacceptable risks to a vulnerable group.
More thought is needed before changing our laws
There is public demand to allow access to voluntary assisted dying for dementia in Australia. The mandatory reviews of voluntary assisted dying legislation present an opportunity to consider such reform. These reviews generally happen after three to five years, and in some states they will occur regularly.
The scope of these reviews can vary and sometimes governments may not wish to consider changes to the legislation. But the Queensland review “must include a review of the eligibility criteria”. And the ACT bill requires the review to consider “advanced care planning”.
Both reviews would require consideration of who is able to access voluntary assisted dying, which opens the door for people living with dementia. This is particularly so for the ACT review, as advance care planning means allowing people to request voluntary assisted dying in the future when they have lost capacity.

The legislation undergoes a mandatory review. Jenny Sturm/Shutterstock This is a complex issue, and more thinking is needed about whether this public desire for voluntary assisted dying for dementia should be implemented. And, if so, how the practice could occur safely, and in a way that is acceptable to the health professionals who will be asked to provide it.
This will require a careful review of existing international models and their practical implementation as well as what would be feasible and appropriate in Australia.
Any future law reform should be evidence-based and draw on the views of people living with dementia, their family caregivers, and the health professionals who would be relied on to support these decisions.
Ben White, Professor of End-of-Life Law and Regulation, Australian Centre for Health Law Research, Queensland University of Technology; Casey Haining, Research Fellow, Australian Centre for Health Law Research, Queensland University of Technology; Lindy Willmott, Professor of Law, Australian Centre for Health Law Research, Queensland University of Technology, Queensland University of Technology, and Rachel Feeney, Postdoctoral research fellow, Queensland University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post

Get The Right Help For Your Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Much Does It Hurt?
Sometimes, a medical professional will ask us to “rate your pain on a scale of 1–10”.
It can be tempting to avoid rating one’s pain too highly, because if we say “10” then where can we go from there? There is always a way to make pain worse, after all.
But that kind of thinking, however logical, is folly—from a practical point of view. Instead of risking having to give an 11 later, you have now understated your level-10 pain as a “7” and the doctor thinks “ok, I’ll give Tylenol instead of morphine”.
A more useful scale
First, know this:
Zero is not “this is the lowest level of pain I get to”.
Zero is “no pain”.
As for the rest…
- My pain is hardly noticeable.
- I have a low level of pain; I am aware of my pain only when I pay attention to it.
- My pain bothers me, but I can ignore it most of the time.
- I am constantly aware of my pain, but can continue most activities.
- I think about my pain most of the time; I cannot do some of the activities I need to do each day because of the pain.
- I think about my pain all of the time; I give up many activities because of my pain.
- I am in pain all of the time; It keeps me from doing most activities.
- My pain is so severe that it is difficult to think of anything else. Talking and listening are difficult.
- My pain is all that I can think about; I can barely move or talk because of my pain.
- I am in bed and I can’t move due to my pain; I need someone to take me to the emergency room because of my pain.
10almonds tip: are you reading this on your phone? Screenshot the above, and keep it for when you need it!
One extra thing to bear in mind…
Medical staff will be more likely to believe a pain is being overstated, on a like-for-like basis, if you are a woman, or not white, or both.
There are some efforts to compensate for this:
A new government inquiry will examine women’s pain and treatment. How and why is it different?
Some other resources of ours:
- The 7 Approaches To Pain Management ← a pain specialist discusses the options available
- Managing Chronic Pain (Realistically!) ← when there’s no quick fix, but these things can buy you some hours’ relief at least / stop the pain from getting worse in the moment
- Science-Based Alternative Pain Relief ← for when you’re maxxed out on painkillers, and need something more/different, these are the things the science says will work
Take care!
Share This Post
Related Posts

The Burden of Getting Medical Care Can Exhaust Older Patients
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Susanne Gilliam, 67, was walking down her driveway to get the mail in January when she slipped and fell on a patch of black ice.
Pain shot through her left knee and ankle. After summoning her husband on her phone, with difficulty she made it back to the house.
And then began the run-around that so many people face when they interact with America’s uncoordinated health care system.
Gilliam’s orthopedic surgeon, who managed previous difficulties with her left knee, saw her that afternoon but told her “I don’t do ankles.”
He referred her to an ankle specialist who ordered a new set of X-rays and an MRI. For convenience’s sake, Gilliam asked to get the scans at a hospital near her home in Sudbury, Massachusetts. But the hospital didn’t have the doctor’s order when she called for an appointment. It came through only after several more calls.
Coordinating the care she needs to recover, including physical therapy, became a part-time job for Gilliam. (Therapists work on only one body part per session, so she has needed separate visits for her knee and for her ankle several times a week.)
“The burden of arranging everything I need — it’s huge,” Gilliam told me. “It leaves you with such a sense of mental and physical exhaustion.”
The toll the American health care system extracts is, in some respects, the price of extraordinary progress in medicine. But it’s also evidence of the poor fit between older adults’ capacities and the health care system’s demands.
“The good news is we know so much more and can do so much more for people with various conditions,” said Thomas H. Lee, chief medical officer at Press Ganey, a consulting firm that tracks patients’ experiences with health care. “The bad news is the system has gotten overwhelmingly complex.”
That complexity is compounded by the proliferation of guidelines for separate medical conditions, financial incentives that reward more medical care, and specialization among clinicians, said Ishani Ganguli, an associate professor of medicine at Harvard Medical School.
“It’s not uncommon for older patients to have three or more heart specialists who schedule regular appointments and tests,” she said. If someone has multiple medical problems — say, heart disease, diabetes, and glaucoma — interactions with the health care system multiply.
Ganguli is the author of a new study showing that Medicare patients spend about three weeks a year having medical tests, visiting doctors, undergoing treatments or medical procedures, seeking care in emergency rooms, or spending time in the hospital or rehabilitation facilities. (The data is from 2019, before the covid pandemic disrupted care patterns. If any services were received, that counted as a day of health care contact.)
That study found that slightly more than 1 in 10 seniors, including those recovering from or managing serious illnesses, spent a much larger portion of their lives getting care — at least 50 days a year.
“Some of this may be very beneficial and valuable for people, and some of it may be less essential,” Ganguli said. “We don’t talk enough about what we’re asking older adults to do and whether that’s realistic.”
Victor Montori, a professor of medicine at the Mayo Clinic in Rochester, Minnesota, has for many years raised an alarm about the “treatment burden” that patients experience. In addition to time spent receiving health care, this burden includes arranging appointments, finding transportation to medical visits, getting and taking medications, communicating with insurance companies, paying medical bills, monitoring health at home, and following recommendations such as dietary changes.
Four years ago — in a paper titled “Is My Patient Overwhelmed?” — Montori and several colleagues found that 40% of patients with chronic conditions such as asthma, diabetes, and neurological disorders “considered their treatment burden unsustainable.”
When this happens, people stop following medical advice and report having a poorer quality of life, the researchers found. Especially vulnerable are older adults with multiple medical conditions and low levels of education who are economically insecure and socially isolated.
Older patients’ difficulties are compounded by medical practices’ increased use of digital phone systems and electronic patient portals — both frustrating for many seniors to navigate — and the time pressures afflicting physicians. “It’s harder and harder for patients to gain access to clinicians who can problem-solve with them and answer questions,” Montori said.
Meanwhile, clinicians rarely ask patients about their capacity to perform the work they’re being asked to do. “We often have little sense of the complexity of our patients’ lives and even less insight into how the treatments we provide (to reach goal-directed guidelines) fit within the web of our patients’ daily experiences,” several physicians wrote in a 2022 paper on reducing treatment burden.
Consider what Jean Hartnett, 53, of Omaha, Nebraska, and her eight siblings went through after their 88-year-old mother had a stroke in February 2021 while shopping at Walmart.
At the time, the older woman was looking after Hartnett’s father, who had kidney disease and needed help with daily activities such as showering and going to the bathroom.
During the year after the stroke, both of Hartnett’s parents — fiercely independent farmers who lived in Hubbard, Nebraska — suffered setbacks, and medical crises became common. When a physician changed her mom’s or dad’s plan of care, new medications, supplies, and medical equipment had to be procured, and new rounds of occupational, physical, and speech therapy arranged.
Neither parent could be left alone if the other needed medical attention.
“It wasn’t unusual for me to be bringing one parent home from the hospital or doctor’s visit and passing the ambulance or a family member on the highway taking the other one in,” Hartnett explained. “An incredible amount of coordination needed to happen.”
Hartnett moved in with her parents during the last six weeks of her father’s life, after doctors decided he was too weak to undertake dialysis. He passed away in March 2022. Her mother died months later in July.
So, what can older adults and family caregivers do to ease the burdens of health care?
To start, be candid with your doctor if you think a treatment plan isn’t feasible and explain why you feel that way, said Elizabeth Rogers, an assistant professor of internal medicine at the University of Minnesota Medical School.
“Be sure to discuss your health priorities and trade-offs: what you might gain and what you might lose by forgoing certain tests or treatments,” she said. Ask which interventions are most important in terms of keeping you healthy, and which might be expendable.
Doctors can adjust your treatment plan, discontinue medications that aren’t yielding significant benefits, and arrange virtual visits if you can manage the technological requirements. (Many older adults can’t.)
Ask if a social worker or a patient navigator can help you arrange multiple appointments and tests on the same day to minimize the burden of going to and from medical centers. These professionals can also help you connect with community resources, such as transportation services, that might be of help. (Most medical centers have staff of this kind, but physician practices do not.)
If you don’t understand how to do what your doctor wants you to do, ask questions: What will this involve on my part? How much time will this take? What kind of resources will I need to do this? And ask for written materials, such as self-management plans for asthma or diabetes, that can help you understand what’s expected.
“I would ask a clinician, ‘If I chose this treatment option, what does that mean not only for my cancer or heart disease, but also for the time I’ll spend getting care?’” said Ganguli of Harvard. “If they don’t have an answer, ask if they can come up with an estimate.”
We’re eager to hear from readers about questions you’d like answered, problems you’ve been having with your care, and advice you need in dealing with the health care system. Visit http://kffhealthnews.org/columnists to submit your requests or tips.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

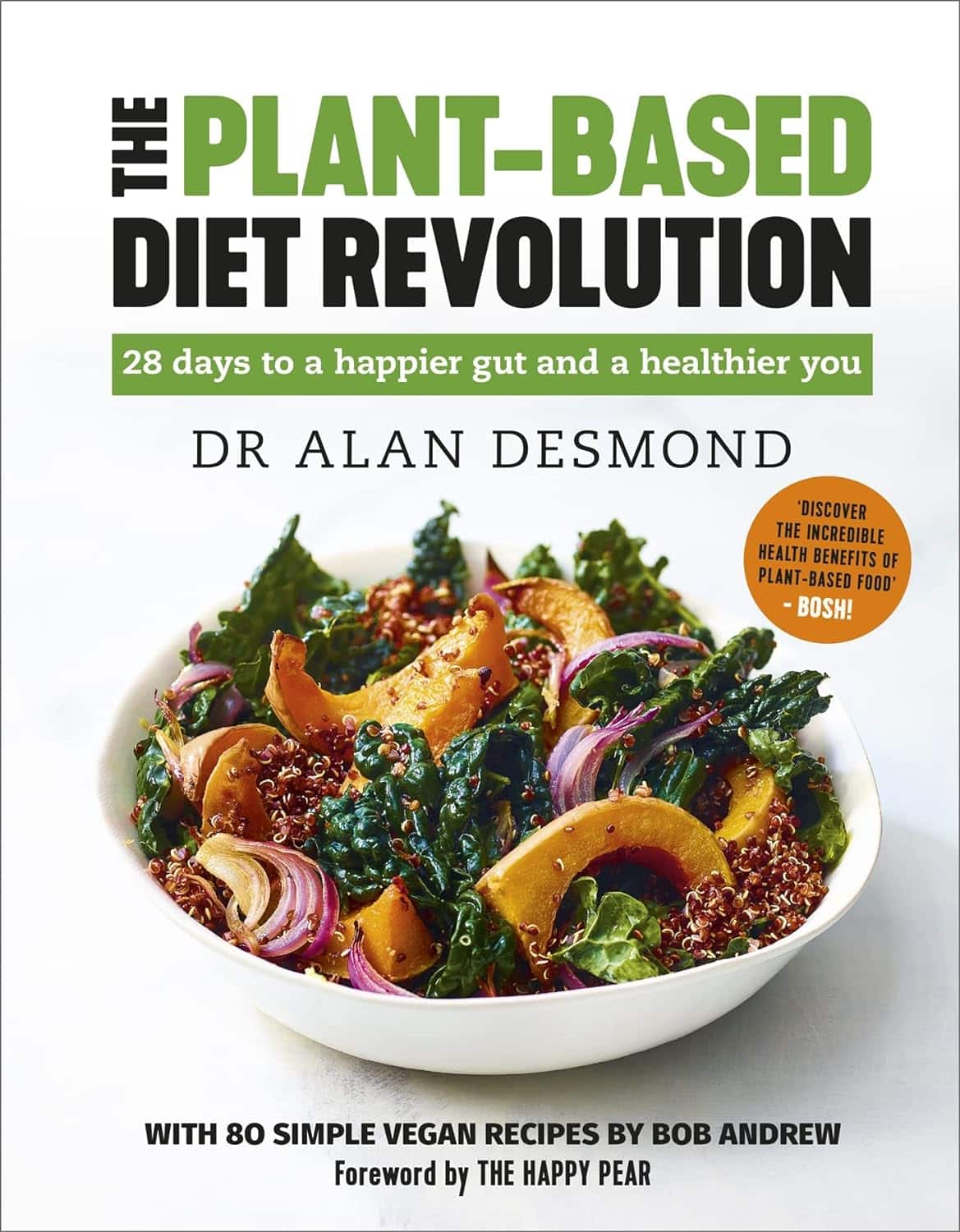
The Plant-Based Diet Revolution – by Dr. Alan Desomond
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is this just another gut-healthy cooking guide? Not entirely…
For a start, it’s not just about giving you a healthy gut; it also covers a healthy heart and a healthy brain. There’s lots of science in here!
It’s also aimed as a transitional guide to eating more plants and fewer animal products, if you so choose. And if you don’t so choose, at least having the flexibility to cook both ways.
The recipes themselves (organized into basics, breakfasts, lunches, mains, desserts) are clear and easy while also being calculated to please readers (and their families) who are used to eating more meat. There are, for instance, plenty of healthy proteins, healthy fats, and comfort foods.
The “28 days” of the title refers to a meal plan using the recipes from the book; it’s not a big feature of the book though, so use it or don’t, but the cooking advice itself is more than worth the price of the book and the recipes are certainly great.
Bottom line: if you’re thinking of taking a “Meatless Mondays” approach to making your diet healthier, this book can help you do that in style!
Click here to check out The Plant-Based Diet Revolution, and upgrade your culinary repertoire!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

A Fresh Take On Hypothyroidism
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Three Rs To Boost Thyroid-Related Energy Levels

This is Dr. Izabella Wentz. She’s a doctor of pharmacology, and after her own diagnosis with Hashimoto’s thyroiditis, she has taken it up as her personal goal to educate others on managing hypothyroidism.
Dr. Wentz is also trained in functional medicine through The Institute for Functional Medicine, Kalish Functional Medicine, and the American Academy of Anti-Aging Medicine. She is a Fellow of the American Society of Consultant Pharmacists, and holds certifications in Medication Therapy Management as well as Advanced Diabetes Care through the American Pharmacists Association. In 2013, she received the Excellence in Innovation Award from the Illinois Pharmacists Association.
Dr. Wentz’s mission
Dr. Wentz was disenchanted by the general medical response to hypothyroidism in three main ways. She tells us:
- Thyroid patients are not diagnosed appropriately.
- For this, she criticises over-reliance on TSH tests that aren’t a reliable marker of thyroid function, especially if you have Hashimoto’s.
- Patients should be better optimized on their medications.
- For this, she criticizes many prescribed drugs that are actually pro-drugs*, that don’t get converted adequately if you have an underactive thyroid.
- Lifestyle interventions are often ignored by mainstream medicine.
- Medicines are great; they truly are. But medicating without adjusting lifestyle can be like painting over the cracks in a crumbling building.
*a “pro-drug” is what it’s called when the drug we take is not the actual drug the body needs, but is a precursor that will get converted to that actual drug we need, inside our body—usually by the liver, but not always. An example in this case is T4, which by definition is a pro-drug and won’t always get correctly converted to the T3 that a thyroid patient needs.
Well that does indeed sound worthy of criticism. But what does she advise instead?
First, she recommends a different diagnostic tool
Instead of (or at least, in addition to) TSH tests, she advises to ask for TPO tests (thyroid peroxidase), and a test for Tg antibodies (thyroglobulin). She says these are elevated for many years before a change in TSH is seen.
Next, identify the root cause and triggers
These can differ from person to person, but in countries that add iodine to salt, that’s often a big factor. And while gluten may or may not be a factor, there’s a strong correlation between celiac disease and Hashimoto’s disease, so it is worth checking too. Same goes for lactose.
By “checking”, here we mean testing eliminating it and seeing whether it makes a difference to energy levels—this can be slow, though, so give it time! It is best to do this under the guidance of a specialist if you can, of course.
Next, get to work on repairing your insides.
Remember we said “this can be slow”? It’s because your insides won’t necessarily bounce back immediately from whatever they’ve been suffering from for what’s likely many years. But, better late than never, and the time will pass anyway, so might as well get going on it.
For this, she recommends a gut-healthy diet with specific dietary interventions for hypothyroidism. Rather than repeat ourselves unduly here, we’ll link to a couple of previous articles of ours, as her recommendations match these:
She also recommends regular blood testing to see if you need supplementary TSH, TPO antibodies, and T3 and T4 hormones—as well as vitamin B12.
Short version
After diagnosis, she recommends the three Rs:
- Remove the causes and triggers of your hypothyroidism, so far as possible
- Repair the damage caused to your body, especially your gut
- Replace the thyroid hormones and related things in which your body has become deficient
Learn more
If you’d like to learn more about this, she offers a resource page, with resources ranging from on-screen information, to books you can get, to links to hook you up with blood tests if you need them, as well as recommended supplements to consider.
She also has a blog, which has an interesting relevant article added weekly.
Enjoy, and take care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Thyroid patients are not diagnosed appropriately.