Tranquility by Tuesday?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
I Know How She Does It: How Successful Women Make The Most of Their Time

This is Laura Vanderkam, author of “Tranquility By Tuesday” (amongst other books). Her “thing” is spending more time on what’s important, and less on what isn’t. Sounds simple, but she’s made a career out of it, so condensed here for you are…
Laura’s 7 Keys To Productivity
Key One: Plan your weeks on Fridays
You don’t want your Monday morning to be a “James Bond intro” (where everything is already in action and you’re just along for the ride, trying to figure out what’s going on). So, take some time last thing each Friday, to plan ahead for the following week!
Key Two: Measure what matters
Whatever that means to you. Laura tracks her use of time in half-hour blocks, and likes keeping track of streaks. For her, that means running daily and keeping a log of it. She also keeps track of the books she reads. For someone else it could be music practice, or a Duolingo streak, or eating fruit each day.
On which note…
“Dr. Greger’s Daily Dozen” is simpler than most nutrition trackers (where you must search for everything you eat, or scan barcodes for all ingredients).
Instead, it keeps track of whether you are having certain key health-giving foods often enough to maintain good health.
We might feature his method in a future edition of 10almonds, but for now, check the app out for yourself here:
Get Dr. Greger’s Daily Dozen on iOS / Get Dr. Greger’s Daily Dozen on Android
Dr. Greger’s Daily Dozen @ Nutrition Facts
Key Three: Figure out 2–3 “anchor” events for the weekend
Otherwise, it can become a bit of a haze and on Monday you find yourself thinking “where did the weekend go?”. So, plan some stuff! It doesn’t have to be anything out-of-this-world, just something that you can look forward to in advance and remember afterwards. It could be a meal out with your family, or a session doing some gardening, or a romantic night in with your partner. Whatever makes your life “living” and not passing you by!
Key Four: Tackle the toughest work first
You’ve probably heard about “swallowing frogs”. If not, there are various versions, usually attributed to Mark Twain.
Here’s one:
“If it’s your job to eat a frog, it’s best to do it first thing in the morning. And if it’s your job to eat two frogs, it’s best to eat the biggest one first.”
Top Productivity App “ToDoist” has an option for this, by the way!
Laura’s key advice here is: get the hard stuff done now! Before you get distracted or tired and postpone it to tomorrow (and then lather rinse repeat, so it never gets done)
10almonds Tip:
“But what if something’s really important but not as pressing as some less important, but more urgent tasks?”
Simple!
Set a timer (we love the Pomodoro method, by the way) and do one burst of the important-but-not-urgent task first. Then you can get to the more urgent stuff.
Repeat each day until the important-but-not-urgent task is done!
The 10almonds Team
Key Five: Use bits of time well
If, like many of us, you’ve a neverending “to read” list, use the 5–10 minute breaks that get enforced upon us periodically through the day!
- Use those few minutes before a meeting/phonecall!
- Use the time you spend waiting for public transport or riding on it!
- Use the time you spent waiting for a family member to finish doing a thing!
All those 5–10 minute bits soon add up… You might as well spend that time reading something you know will add value to your life, rather than browsing social media, for example.
Key Six: Make very short daily to-do lists
By “short”, Laura considers this “under 10 items”. Do this as the last part of your working day, ready for tomorrow. Not at bedtime! Bedtime is for winding down, not winding up
Key Seven: Have a bedtime
Laura shoots for 10:30pm, but whatever works for you and your morning responsibilities. Your morning responsibilities aren’t tied to a specific time? Lucky you, but try to keep a bedtime anyway. Otherwise, your daily rhythm can end up sliding around the clock, especially if you work from home!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Zucchini vs Okra – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing zucchini to okra, we picked the okra.
Why?
Looking at the macros first, okra has nearly 2x the protein and more than 3x the fiber (for about 2x the carbs).
In terms of vitamins, things are also quite one-sided; zucchini has a little more vitamin B2, while okra has a lot more of vitamins A, B1, B3, B5, B6, B9, C, E, K, and choline.
Nor does the mineral situation make any compelling counterargument; zucchini is higher only in sodium, while okra has a lot more calcium, copper, iron, magnesium, manganese, phosphorus, potassium*, selenium, and zinc.
*Actually it’s only a little more potassium. But the rest are with big margins of difference.
Both of these on-the-cusp-of-being-pungent vegetables have beneficial antioxidant polyphenols (especially various forms of quercetin), but okra has more.
In short: enjoy both, of course, but there’s a clear winner here and it’s okra.
Want to learn more?
You might like to read:
Enjoy Bitter/Astringent/Pungent Foods For Your Heart & Brain
Take care!
Share This Post
-
6 Signs Of A Heart Attack… A Month In Advance
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many people know the signs of a heart attack when it’s happening, but how about before it’s too late to avoid it?
The signs
- Unusual fatigue: persistent tiredness that doesn’t improve with rest
- Shortness of breath: unexplained breathlessness during light activities or rest, which can be caused by fluid buildup in the lungs (because the heart isn’t circulating blood as well as it should)
- Chest discomfort: pain, pressure, tightness, or aching in the chest due to reduced blood flow to the heart muscle—often occurring during physical exertion or emotional stress
- Frequent indigestion: means that heartburn could be heart-related! This is about persistently reoccurring discomfort or pain in the upper abdomen
- Sleep disturbances: difficulties falling asleep, staying asleep, or waking up abruptly
- Excessive sweating: unexplained cold sweats or sudden sweating without physical exertion or excessive heat, can be a response to the decreased oxygen levels caused by less efficient blood flow
Note: this is a list of warning signs, not a diagnostic tool. Any or even all of these could be caused by something else. Just, don’t ignore the signs and do get yourself checked out.
For more details on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
What Weston Price Got Right (And Wrong)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Weston Price: What Stood The Test of Time?
This is Dr. Weston Price, a dentist. You may guess from the photo, or perhaps already knew, his work is not new in 2023. We usually feature current health experts here, but we’re taking a day to do a blast from the past, because his ideas endure today, and inform a lot of people’s health views. So, he’s a good one to at least know about.
What was his deal?
Dr. Price (1870–1948) wanted to study focal infection theory—the idea that repairing root canals allowed bacterial infections that caused everything from heart disease to arthritis. His solution was that the teeth should be extracted instead.
This theory was popular in the 1920s, was challenged in the 1930s, ignored in the 1940s (the world was a bit busy), and by broad medical consensus anyway, rejected in the 1950s. But, while it was being challenged in the 1930s, Dr. Price decided to find more evidence for its support.
The result was his famous world tour of peoples living traditional lifestyles without the influence of “modern” diet. His findings, and the conclusions he drew from them, extended to far more than just dental health.
What did he find?
Dr. Price found that people living traditional lifestyles, with their traditional diets based on locally-sourced foods, had much better overall health. Of course, he was a dentist and not a general practitioner, so aside from examining their teeth, he largely relied on self-reported diagnoses of illness, or lack thereof.
In short: he found that people in places without modern medical institutions had fewer diagnoses of disease. From this, he concluded that incidence of disease was much lower.
There was also an unexamined element of survivorship bias—an undiagnosed disease is more likely to be fatal, and he questioned only living people, which skewed the stats rather. Nor did he examine infant mortality rate nor adult life expectancy, both of which were not great.
Was it all useless, then?
Actually no! He did hit upon some observations that have stood the test of time:
- He correctly concluded that modern diets with sugar and white flour were ruinous to the health.
- He correctly concluded that locally-sourced food, and grass-fed in the case of pastoral farming, tended to have much more nutritional value than the mass-produced results of intensive farming.
- He correctly concluded that many modern preservation methods robbed foods of their nutrients.
- He correctly concluded that many grains and seeds are more nutritions when fermented/soaked/sprouted.
About that “locally-sourced food”: the reason locally-sourced food tends to be more nutritious is that it has required less in the way of preservation for a long trip around the world, and will also tend to be fresher.
On the other hand, this does mean a lot of the foods that Dr. Price recommends are very much subject to availability. It may well be true that the Inuit people do not eat a lot of fruit and veg (which mostly do not grow there), but if you live in Nevada, maybe locally-sourced whale fat is just as difficult to find.
One person’s “this fatty organ meat contains the vitamin C we need” may be another person’s “that’s great; I have an apple tree in my garden though”.
Want to learn more?
Dr. Price’s most influential work is his magnum opus, “Nutrition and Physical Degeneration”. It’s a fascinating book in its historical context, but do be warned, it was written by a rich white man in 1939 and the writing is as racist as you might expect. Even when making favourable comparisons, the tone is very much “and here is what these savages are doing well”.
If you don’t fancy reading all that, here are two other sources about Weston Price’s work and conclusions, presented for balance:
- The Weston A. Price Foundation (Official Website)
- Weston Price’s Appalling Legacy (Science-Based Medicine.org)
Enjoy!
Share This Post
Related Posts
-
Healthy Butternut Macaroni Cheese
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A comfort food classic, healthy and plant-based, without skimping on the comfort.
You will need
- ½ butternut squash, peeled and cut into small pieces (if buying ready-chopped, this should be about 1 lb)
- 1 onion, chopped
- ¼ bulb garlic
- 2 tbsp extra virgin olive oil
- 12 oz (or thereabouts) wholegrain macaroni, or similar pasta shape (even penne works fine—which is good, as it’s often easier to buy wholegrain penne than wholegrain macaroni) (substitute with a gluten-free pasta such as buckwheat pasta, if avoiding gluten)
- 6 oz (or thereabouts) cashews, soaked in hot water for at least 15 minutes (but longer is better)
- ½ cup milk (your preference what kind; we recommend hazelnut for its mellow nutty flavor)
- 3 tbsp nutritional yeast
- Juice of ½ lemon
- 2 tsp black pepper, coarse ground
- ½ tsp MSG, or 1 tsp low-sodium salt
- Optional: smoked paprika, to serve
Note: if you are allergic to nuts, please accept our apologies that there’s no substitution available in this one. Simply put, removing the cashews would mean changing most of the rest of the recipe to compensate, so there’s no easy “or substitute with…” that we can mention. We’ll have to find/develop a good healthy plant-based no-nuts recipe for you at a later date.
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉ / 200℃.
2) Combine the butternut squash, onion, and garlic with the olive oil, in a large roasting tin, tossing thoroughly to ensure an even coat of oil. Roast them for about 25 minutes until soft.
3) Cook the macaroni while you wait (this should take about 10 minutes or so in salted water), drain, and rinse thoroughly in cold water, before setting aside. This cooling increases the pasta’s resistant starch content (that’s good, for your gut and for your blood sugars, and thus also for your heart and brain), and it will maintain this benefit even when we reheat it later.
4) Drain the cashews, and tip them into a high-speed blender with the milk, and process until smooth. Add the roasted vegetables and the remaining ingredients apart from the pasta, and continue to process until again smooth. You can add a little more milk if you need to, but go easy with it.
5) Heat the sauce (that you just made in the food processor) gently in a saucepan, and refresh the pasta by pouring a kettle of boiling water through it in a colander.
6) Optional: combine the pasta and sauce in an ovenproof dish or cast iron pan, and give it a few minutes under the hottest grill (or browning iron, if you have such) your oven can muster. Alternatively, use a culinary blowtorch, if you have one.
7) Serve; and if you didn’t do the optional step above, this means combining the pasta and sauce. You can also dust the top with some extra seasonings if you like. Smoked paprika works well for this.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Butternut Squash vs Pumpkin – Which is Healthier?
- Cashew Nuts vs Coconut – Which is Healthier?
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Sea Salt vs MSG – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
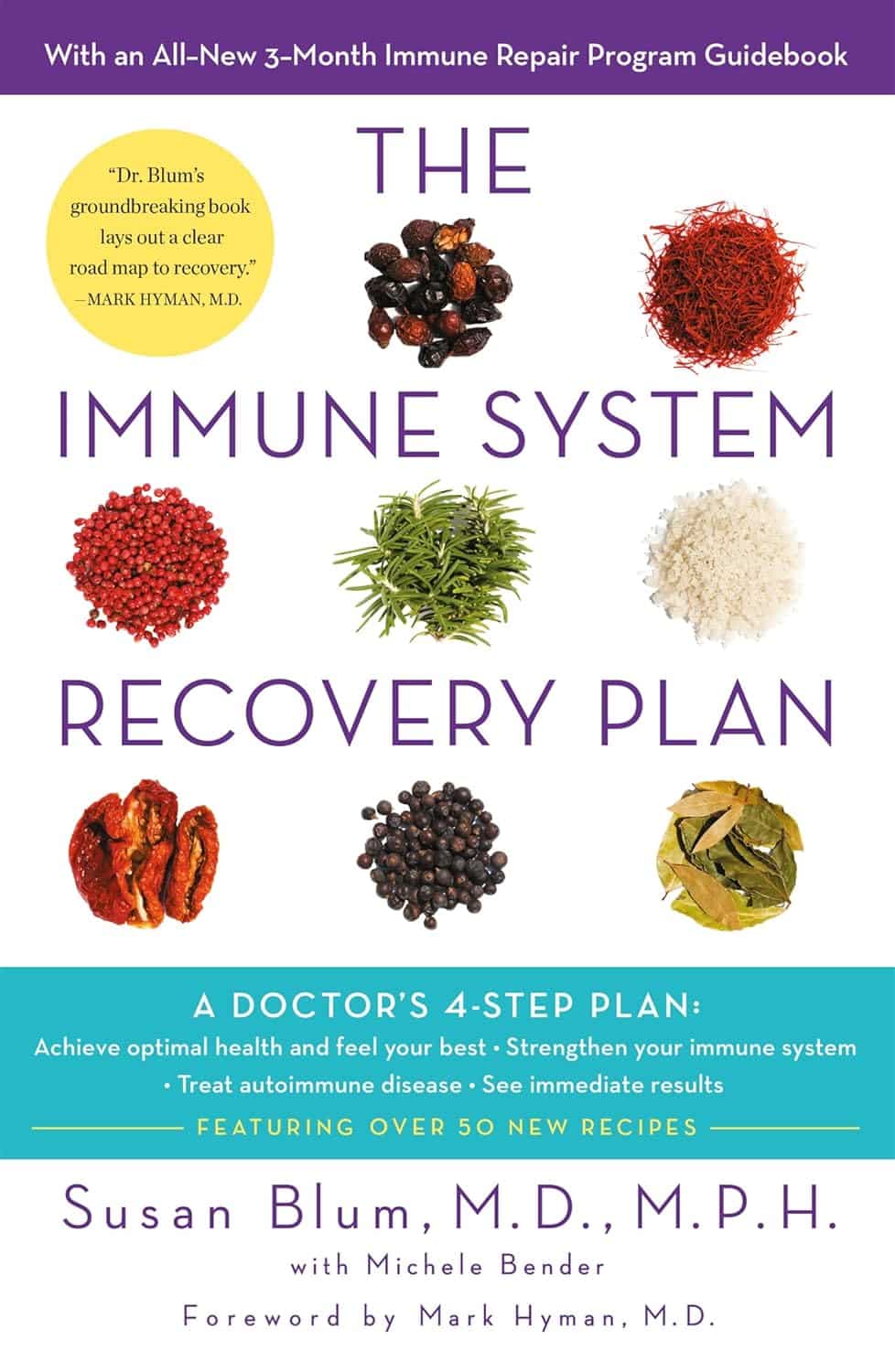
The Immune System Recovery Plan – by Dr. Susan Blum
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The subtitle of the book is “A Doctor’s 4-Step Program to Treat Autoimmune Disease”, so we’ll not keep the four steps a secret; they are:
- Using food as medicine
- Understanding the stress connection
- Healing your gut and digestive system
- Optimizing liver function
Each of these sections gives a primer in the relevant science, worksheets for personalizing your own plan to your own situation, condition, and goals, and of course lots of practical advice.
This is important and perhaps the book’s greatest strength, since there are dozens of possible autoimmune conditions, and getting a professional diagnosis is often a long, arduous process. So while this book can’t necessarily speed that up, what it can do is give you a good head-start on managing your symptoms based on things that are most likely to help, and certainly, there will be no harm trying.
While it’s not primarily a recipe book, there are also recipes targeting each part of the whole, as well as an extensive herb and supplement guide, before getting into lots of additional resources.
Bottom line: if you are, or suspect you are, suffering from an autoimmune condition, the information in this book can make your life a lot easier.
Click here to check out The Immune System Recovery Plan, and help yours to help you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Much Does A Vegan Diet Affect Biological Aging?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Slow Your Aging, One Meal At A Time
This one’s a straightforward one today, and the ““life hack” can be summed up:
Enjoy a vegan diet to enjoy younger biological age.
First, what is biological age?
Biological age is not one number, but a collection of numbers, as per different biomarkers of aging, including:
- Visual markers of aging (e.g. wrinkles, graying hair)
- Performative markers of aging (e.g. mobility tests)
- Internal functional markers of aging (e.g. tests for cognitive decline, eyesight, hearing, etc)
- Cellular markers of aging (e.g. telomere length)
We wrote more about this here:
Age & Aging: What Can (And Can’t) We Do About It?
A vegan diet may well impact multiple of those categories of aging, but today we’re highlighting a study (hot off the press; published only a few days ago!) that looks at its effect on that last category: cellular markers of aging.
There’s an interesting paradox here, because this category is:
- the most easily ignorable; because we all feel it if our knees are giving out or our skin is losing elasticity, but who notices if telomeres’ T/S ratio changed by 0.0407? ← the researchers, that’s who, as this difference is very significant
- the most far-reaching in its impact, because cellular aging in turn has an effect on all the other markers of aging
Second, how much difference does it make, and how do we know?
The study was an eight-week interventional identical twin study. This means several things, to start with:
- Eight weeks is a rather short period of time to accumulate cellular aging, let alone for an intervention to accumulate a significant difference in cellular aging—but it did. So, just imagine what difference it might make in a year or ten!
- Doing an interventional study with identical twin pairs already controlled for a lot of factors, that are usually confounding variables in population / cohort / longitudinal / observational studies.
Factors that weren’t controlled for by default by using identical twins, were controlled for in the experiment design. For example, twin pairs were rejected if one or more twin in a given pair already had medical conditions that could affect the outcome:
❝Inclusion criteria involved participants aged ≥18, part of a willing twin pair, with BMI <40, and LDL-C <190 mg/dL. Exclusions included uncontrolled hypertension, metabolic disease, diabetes, cancer, heart/renal/liver disease, pregnancy, lactation, and medication use affecting body weight or energy.
Eligibility was determined via online screening, followed by an orientation meeting and in-person clinic visit. Randomization occurred only after completing baseline visits, dietary recalls, and questionnaires for both twins❞
~ Dr. Varun Dwaraka et al. ← there’s a lot of “et al.” to this one; the paper had 16 collaborating authors!
As to the difference it made over the course of the 8 weeks…
❝Various measures of epigenetic age acceleration (PC GrimAge, PC PhenoAge, DunedinPACE) were assessed, along with system-specific effects (Inflammation, Heart, Hormone, Liver, and Metabolic).
Distinct responses were observed, with the vegan cohort exhibiting significant decreases in overall epigenetic age acceleration, aligning with anti-aging effects of plant-based diets. Diet-specific shifts were noted in the analysis of methylation surrogates, demonstrating the influence of diet on complex trait prediction through DNA methylation markers.❞
~ Ibid.
You can read the whole paper here (it goes into a lot more detail than we have room to here, and also gives infographics, charts, numbers, the works):
Were they just eating more healthily, though?
Well, arguably yes, as the results show, but to be clear:
The omnivorous diet compared to the vegan diet in this study was also controlled; both groups were given a healthy meal plan for their respective diet. So this wasn’t a case of “any omnivorous diet vs healthy vegan diet”, but rather “healthy omnivorous diet vs healthy vegan diet”.
Again, the paper itself has the full details—a short version is that it involved a healthy meal kit delivery service, followed by ongoing dietician involvement in an equal and carefully-controlled fashion.
So, aside from that one group had an omnivorous meal plan and the other vegan, both groups received the same level of “healthy eating” support, guidance, and oversight.
But isn’t [insert your preferred animal product here] healthy?
Quite possibly! For general health, general scientific consensus is that eating at least mostly plants is best, red meat is bad, poultry is neutral in moderation, fish is good in moderation, dairy is good in moderation if fermented, eggs are good in moderation if not fried.
This study looked at the various biomarkers of aging that we listed, and not every possible aspect of health—there’s more science yet to be done, and the researchers themselves are calling for it.
It also bears mentioning that for some (relatively few, but not insignificantly few) people, extant health conditions may make a vegan diet unhealthy or otherwise untenable. Do speak with your own doctor and/or dietician if unsure.
See also: Do We Need Animal Products To Be Healthy?
We would hypothesize, by the way, that the anti-aging benefits of a vegan diet are probably proportional to abstention from animal products—meaning that even if you simply have some “vegan days”, while still consuming animal products other days, you’ll still get benefit for the days you abstained. That’s just our hypothesis though.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: