Considering taking Wegovy to lose weight? Here are the risks and benefits – and how it differs from Ozempic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The weight-loss drug Wegovy is now available in Australia.
Wegovy is administered as a once-weekly injection and is approved specifically for weight management. It’s intended to be used in combination with a reduced-energy diet and increased physical activity.
So how does Wegovy work and how much weight can you expect to lose while taking it? And what are the potential risks – and costs – for those who use it?
Let’s look at what the science says.

What is Wegovy?
Wegovy is a brand name for the medication semaglutide. Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1RA). This means it makes your body’s own glucagon-like peptide-1 hormone, called GLP-1 for short, work better.
Normally when you eat, the body releases the GLP-1 hormone which helps signal to your brain that you are full. Semaglutides enhance this effect, leading to a feeling of fullness, even when you haven’t eaten.
Another role of GLP-1 is to stimulate the body to produce more insulin, a hormone which helps lower the level of glucose (sugar) in the blood. That’s why semaglutides have been used for several years to treat type 2 diabetes.

How does Wegovy differ from Ozempic?
Like Wegovy, Ozempic is a semaglutide. The way Wegovy and Ozempic work in the body are essentially the same. They’re made by the same pharmaceutical company, Novo Nordisk.
But there are two differences:
1) They are approved for two different (but related) reasons.
In Australia (and the United States), Ozempic is approved for use to improve blood glucose levels in adults with type 2 diabetes. By managing blood glucose levels effectively, the medication aims to reduce the risk of major complications, such as heart disease.
Wegovy is approved for use alongside diet and exercise for people with a body mass index (BMI) of 30 or greater, or 27 or greater but with other conditions such as high blood pressure.
Wegovy can also be used in people aged 12 years and older. Like Ozempic, Wegovy aims to reduce the risk of future health complications, including heart disease.
2) They are both injected but come in different strengths.
Ozempic is available in pre-loaded single-dose pens with varying dosages of 0.25 mg, 0.5 mg, 1 mg, or 2 mg per injection. The dose can be slowly increased, up to a maximum of 2 mg per week, if needed.
Wegovy is available in prefilled single-dose pens with doses of 0.25 mg, 0.5 mg, 1 mg, 1.7 mg, or 2.4 mg. The treatment starts with a dose of 0.25 mg once weekly for four weeks, after which the dose is gradually increased until reaching a maintenance dose of 2.4 mg weekly.
While it’s unknown what the impact of Wegovy’s introduction will be on Ozempic’s availability, Ozempic is still anticipated to be in low supply for the remainder of 2024.
Is Wegovy effective for weight loss?
Given Wegovy is a semaglutide, there is very strong evidence it can help people lose weight and maintain this weight loss.
A recent study found that over four years, participants taking Wevovy as indicated experienced an average weight loss of 10.2% body weight and a reduction in waist circumference of 7.7cm.
For those who stop taking the medication, analyses have shown that about two-thirds of weight lost is regained.

What are the side effects of Wegovy?
The most common side effects are nausea and vomiting.
However, other serious side effects are also possible because of the whole-of-body impact of the medication. Thyroid tumours and cancer have been detected as a risk in animal studies, yet are rarely seen in human scientific literature.
In the four-year Wegovy trial, 16.6% of participants who received Wegovy (1,461 people) experienced an adverse event that led to them permanently discontinuing their use of the medication. This was higher than the 8.2% of participants (718 people) who received the placebo (with no active ingredient).
Side effects included gastrointestinal disorders (including nausea and vomiting), which affected 10% of people who used Wegovy compared to 2% of people who used the placebo.
Gallbladder-related disorders occurred in 2.8% of people who used Wegovy, and 2.3% of people who received the placebo.
Recently, concerns about suicidal thoughts and behaviours have been raised, after a global analysis reviewed more than 36 million reports of adverse events from semaglutide (Ozempic or Wegovy) since 2000.
There were 107 reports of suicidal thoughts and self-harm among people taking semaglutide, sadly including six actual deaths. When people stopped the medication, 62.5% found the thoughts went away. What we don’t know is whether dose, weight loss, or previous mental health status or use of antidepressants had a role to play.
Finally, concerns are growing about the negative effect of semaglutides on our social and emotional connection with food. Anecdotal and scientific evidence suggests people who use semaglutides significantly reduce their daily dietary intake (as anticipated) by skipping meals and avoiding social occasions – not very enjoyable for people and their loved ones.
How can people access Wegovy?
Wegovy is available for purchase at pharmacists with a prescription from a doctor.
But there is a hefty price tag. Wegovy is not currently subsidised through the Pharmaceutical Benefits Scheme, leaving patients to cover the cost. The current cost is estimated at around A$460 per month dose.
If you’re considering Wegovy, make an appointment with your doctor for individual advice.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
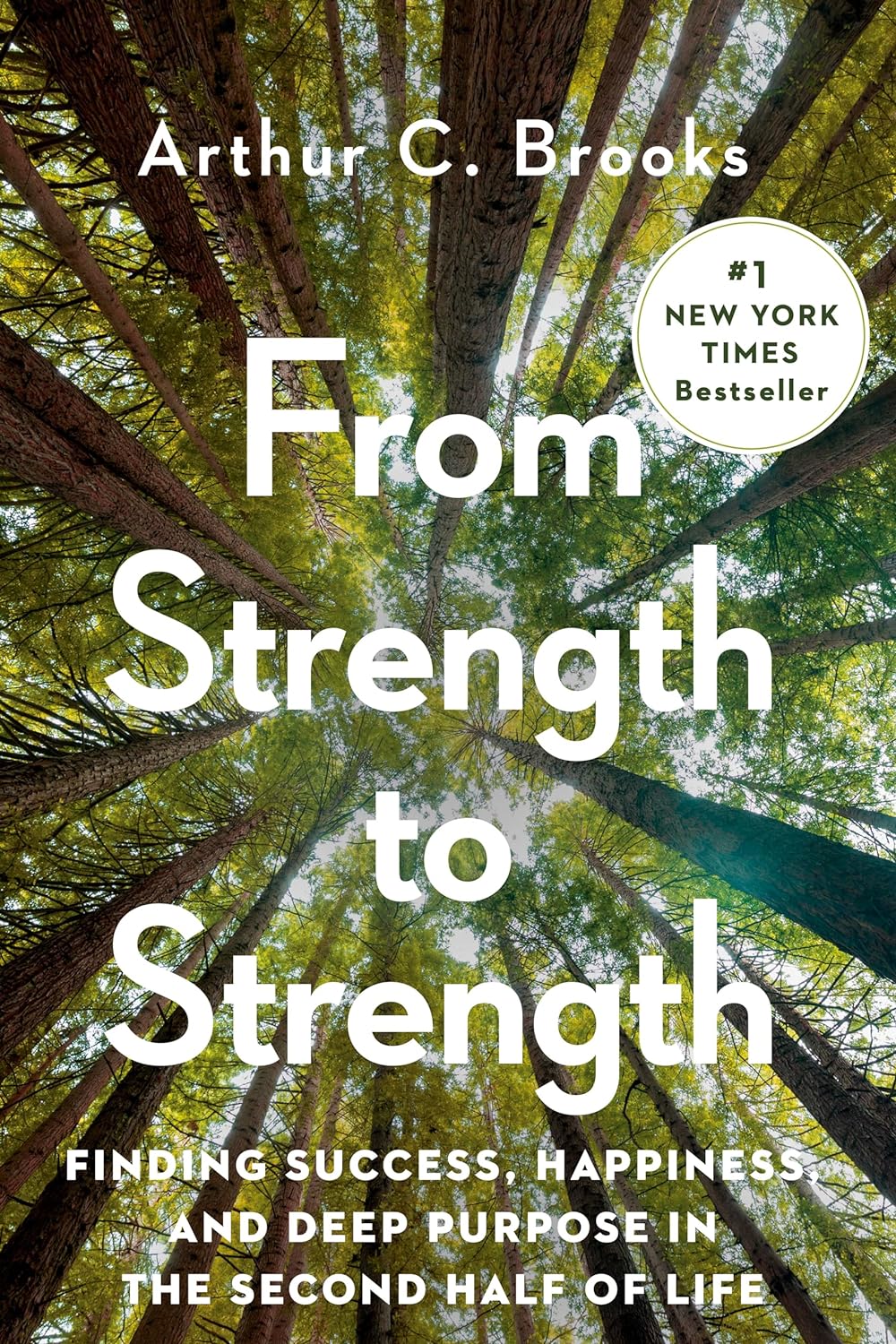
From Strength to Strength – by Dr. Arthur Brooks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For most professions, there are ways in which performance can be measured, and the average professional peak varies by profession, but averages are usually somewhere in the 30–45 range, with a pressure to peak between 25–35.
With a peak by age 45 or perhaps 50 at the latest (aside from some statistical outliers, of course), what then to expect at age 50+? Not long after that, there’s a reason for mandatory retirement ages in some professions.
Dr. Brooks examines the case for accepting that rather than fighting it, and/but making our weaknesses into our strengths as we go. If our fluid intelligence slows, our accumulated crystal intelligence (some might call it “wisdom“) can make up for it, for example.
But he also champions the idea of looking outside of ourselves; of the importance of growing and fostering connections; giving to those around us and receiving support in turn; not transactionally, but just as a matter of mutualism of the kind found in many other species besides our own. Indeed, Dr. Brooks gives the example of a grove of aspen trees (hence the cover art of this book) that do exactly that.
The style is very accessible in terms of language but with frequent scientific references, so very much a “best of both worlds” in terms of readability and information-density.
Bottom line: if ever you’ve wondered at what age you might outlive your usefulness, this book will do as the subtitle suggests, and help you carve out your new place.
Click here to check out From Strength To Strength, and find yours!
Share This Post
-
Do Try This At Home: The 12-Week Brain Fitness Program
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
12 Weeks To Measurably Boost Your Brain
This is Dr. Majid Fotuhi. From humble beginnings (being smuggled out of Iran in 1980 to avoid death in the war), he went on (after teaching himself English, French, and German, hedging his bets as he didn’t know for sure where life would lead him) to get his MD from Harvard Medical School and his PhD in neuroscience from Johns Hopkins University. Since then, he’s had a decades-long illustrious career in neurology and neurophysiology.
What does he want us to know?
The Brain Fitness Program
This is not, by the way, something he’s selling. Rather, it was a landmark 12-week study in which 127 people aged 60–80, of which 63% female, all with a diagnosis of mild cognitive impairment, underwent an interventional trial—in other words, a 12-week brain fitness course.
After it, 84% of the participants showed statistically significant improvements in cognitive function.
Not only that, but of those who underwent MRI testing before and after (not possible for everyone due to practical limitations), 71% showed either no further deterioration of the hippocampus, or actual growth above the baseline volume of the hippocampus (that’s good, and it means functionally the memory center of the brain has been rejuvenated).
You can read a little more about the study here:
As for what the program consisted of, and what Dr. Fotuhi thus recommends for everyone…
Cognitive stimulation
This is critical, so we’re going to spend most time on this one—the others we can give just a quick note and a pointer.
In the study this came in several forms and had the benefit of neurofeedback technology, but he says we can replicate most of the effects by simply doing something cognitively stimulating. Whatever challenges your brain is good, but for maximum effect, it should involve the language faculties of the brain, since these are what tend to get hit most by age-related cognitive decline, and are also what tends to have the biggest impact on life when lost.
If you lose your keys, that’s an inconvenience, but if you can’t communicate what is distressing you, or understand what someone is explaining to you, that’s many times worse—and that kind of thing is a common reality for many people with dementia.
To keep the lights brightly lit in that part of the brain: language-learning is good, at whatever level suits you personally. In other words: there’s a difference between entry-level Duolingo Spanish, and critically analysing Rumi’s poetry in the original Persian, so go with whatever is challenging and/but accessible for you—just like you wouldn’t go to the gym for the first time and try to deadlift 500lbs, but you also probably wouldn’t do curls with the same 1lb weights every day for 10 years.
In other words: progressive overloading is key, for the brain as well as for muscles. Start easy, but if you’re breezing through everything, it’s time to step it up.
If for some reason you’re really set against the idea of learning another language, though, check out:
Reading As A Cognitive Exercise ← there are specific tips here for ensuring your reading is (and remains) cognitively beneficial
Mediterranean diet
Shocking nobody, this is once again recommended. You might like to check out the brain-healthy “MIND” tweak to it, here:
Four Ways To Upgrade The Mediterranean Diet ← it’s the fourth one
Omega-3 supplementation
Nothing complicated here. The brain needs a healthy balance of these fatty acids to function properly, and most people have an incorrect balance (too little omega-3 for the omega-6 present):
What Omega-3 Fatty Acids Really Do For Us ← scroll to “against cognitive decline”
Increasing fitness
There’s a good rule of thumb: what’s healthy for your heart, is healthy for your brain. This is because, like every other organ in your body, the brain does not function well without good circulation bringing plenty of oxygen and nutrients, which means good cardiovascular health is necessary. The brain is extra sensitive to this because it’s a demanding organ in terms of how much stuff it needs delivering via blood, and also because of the (necessary; we’d die quickly and horribly without it) impediment of the blood-brain barrier, and the possibility of beta-amyloid plaques and similar woes (they will build up if circulation isn’t good).
How To Reduce Your Alzheimer’s Risk ← number two on the list here
Practising mindfulness medication
This is also straightforward, but not to be underestimated or skipped over:
No-Frills, Evidence-Based Mindfulness
Want to step it up? Check out:
Meditation Games That You’ll Actually Enjoy
Lastly…
Dr. Fotuhi wants us to consider looking after our brain the same way we look after our teeth. No, he doesn’t want us to brush our brain, but he does want us to take small measurable actions multiple times per day, every day.
You can’t just spend the day doing nothing but brushing your teeth for the entirety of January the 1st and then expect them to be healthy for the rest of the year; it doesn’t work like that—and it doesn’t work like that for the brain, either.
So, make the habits, and keep them going
Take care!
Share This Post
-
What does lion’s mane mushroom actually do, anyway?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may know it as an ingredient in nootropic supplements. You may have heard of lion’s mane mushroom coffee. You may know it as the big shaggy white mushroom that grows in nature and can look very impressive.
What’s special about it?
The lion’s mane mushroom, or Hericium erinaceus (we mention, as studies we’ll cite often use the botanical name) is an adaptogenic agent that has an established ability to promote nerve regeneration through nerve growth factor neurotrophic activity. In other words, it helps (re)grow neurons.
In a 2023 study, researchers wondered if its abilities (well-established in the peripheral nervous system) would work in the central nervous system too, namely the brain, specifically the hippocampus (responsible for memory).
To boil what they found down to a single line, they concluded:
❝[Lion’s mane extract] therefore acts through a novel pan-neurotrophic signaling pathway, leading to improved cognitive performance.❞
You can read the full study for yourself (with pictures!) here:
Limitations of the study
It’s worth noting that the above study was performed on mice brains, not those of humans. As there is a shortage of human volunteers willing to have their brains sliced and examined under microscopes, we do not expect this study to be repeated with humans any time soon.
So, are there human studies that have been done?
There are! Particularly promising was this 2020 study of people with Alzheimer’s disease, wherein supplementation with 1g of lion’s mane mushroom daily for 49 weeks significantly increased cognitive test scores compared with a placebo; you can read about it here:
Additionally, this 2019 study showed that taking 1.2g daily for eight weeks helped relieve depression, anxiety, and sleep disorders in overweight or obese patiences:
Are there other health benefits?
It seems so! Unfortunately, most of its other health claims are only supported by animal studies so far, aside from one small study funded by a supplement company for their supplement that contained mostly Agaricus blazei (a different mushroom) with 14% lion’s mane.
However, in animal studies, lion’s mane has also shown promise:
- For digestion
- Against inflammation
- For cardiovascular health
- For diabetes management
- Against cancer
- Against aging
Where can I get it?
We don’t sell it (or anything else, for that matter) but if you’d like to try it, here’s an example product for your convenience:
Share This Post
Related Posts
-
Wanna read more?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You’ve Got Questions? We’ve Got Answers!
Q: Tips for reading more and managing time for it?
A: We talked about this a little bit in yesterday’s edition, so you may have seen that, but aside from that:
- If you don’t already have one, consider getting a Kindle or similar e-reader. They’re very convenient, and also very light and ergonomic—no more wrist strain as can occur with physical books. No more eye-strain, either!
- Consider making reading a specific part of your daily routine. A chapter before bed can be a nice wind-down, for instance! What’s important is it’s a part of your day that’ll always, or at least almost always, allow you to do a little reading.
- If you drive, walk, run, or similar each day, a lot of people find that’s a great time to listen to an audiobook. Please be safe, though!
- If your lifestyle permits such, a “reading retreat” can be a wonderful vacation! Even if you only “retreat” to your bedroom, the point is that it’s a weekend (or more!) that you block off from all other commitments, and curl up with the book(s) of your choice.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Diet Tips for Crohn’s Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Doctors are great at saving lives like mine. I’m a two time survivor of colon cancer and have recently been diagnosed with Chron’s disease at 62. No one is the health system can or is prepared to tell me an appropriate diet to follow or what to avoid. Can you?❞
Congratulations on the survivorship!
As to Crohn’s, that’s indeed quite a pain, isn’t it? In some ways, a good diet for Crohn’s is the same as a good diet for most other people, with one major exception: fiber
…and unfortunately, that changes everything, in terms of a whole-foods majority plant-based diet.
What stays the same:
- You still ideally want to eat a lot of plants
- You definitely want to avoid meat and dairy in general
- Eating fish is still usually* fine, same with eggs
- Get plenty of water
What needs to change:
- Consider swapping grains for potatoes or pasta (at least: avoid grains)
- Peel vegetables that are peelable; discard the peel or use it to make stock
- Consider steaming fruit and veg for easier digestion
- Skip spicy foods (moderate spices, like ginger, turmeric, and black pepper, are usually fine in moderation)
Much of this latter list is opposite to the advice for people without Crohn’s Disease.
*A good practice, by the way, is to keep a food journal. There are apps that you can get for free, or you can do it the old-fashioned way on paper if prefer.
But the important part is: make a note not just of what you ate, but also of how you felt afterwards. That way, you can start to get a picture of patterns, and what’s working (or not) for you, and build up a more personalized set of guidelines than anyone else could give to you.
We hope the above pointers at least help you get going on the right foot, though!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Blue Zones Kitchen – by Dan Buettner
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Buettner’s other book, The Blue Zones: 9 Lessons For Living Longer From The People Who’ve Lived The Longest, and with this one, it’s now time to focus on the dietary aspect.
As the title and subtitle promises, we get 100 recipes, inspired by Blue Zone cuisines. The recipes themselves have been tweaked a little for maximum healthiness, eliminating some ingredients that do crop up in the Blue Zones but are exceptions to their higher average healthiness rather than the rule.
The recipes are arranged by geographic zone rather than by meal type, so it might take a full read-through before knowing where to find everything, but it makes it a very enjoyable “coffee-table book” to browse, as well as being practical in the kitchen. The ingredients are mostly easy to find globally, and most can be acquired at a large supermarket and/or health food store. In the case of substitutions, most are obvious, e.g. if you don’t have wild fennel where you are, use cultivated, for example.
In the category of criticism, it appears that Buettner is very unfamiliar with spices, and so has skipped them almost entirely. We at 10almonds could never skip them, and heartily recommend adding your own spices, for their health benefits and flavors. It may take a little experimentation to know what will work with what recipes, but if you’re accustomed to cooking with spices normally, it’s unlikely that you’ll err by going with your heart here.
Bottom line: we’d give this book a once-over for spice additions, but aside from that, it’s a fine book of cuisine-by-location cooking.
Click here to check out The Blue Zones Kitchen, and get cooking into your own three digits!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: