Cherries vs Grapes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cherries to grapes, we picked the cherries.
Why?
First, let’s mention: we are looking at sour cherries and Californian grapes. Even those will of course vary in quality, but the nutritional values here are quite reliable averages.
In terms of macros you might have guessed this one: cherries have nearly 2x the fiber and grapes have about 50% more carbs. So, while neither fruit is bad and they are both low glycemic index foods, cherry is the winner in this category.
When it comes to vitamins, cherries have more of vitamins A, B3, B5, B9, C, and choline, while grapes have more of vitamins B1, B2, B6, E, and K. That’s a 6:5 win for cherries, and the respective margins of difference bear that out too.
In the category of minerals, cherries have more calcium, copper, iron, magnesium, phosphorus, and zinc, while grapes have more manganese and potassium. An easy 6:2 win for cherries.
You might be wondering about polyphenols: both are very abundant in very many polyphenols; so much and so many, in fact, that we couldn’t possibly try to adjudicate between them without doing some complex statistical modeling (especially given how much this can vary from one sample to another, much more so than the micro-and macronutrient values discussed above), so we’ll call it a tie on these.
Adding up the section makes for a clear win for cherries, but of course, enjoy either or both!
Want to learn more?
You might like to read:
Cherries’ Very Healthy Wealth Of Benefits!
Resveratrol & Healthy Aging
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Problem With Active Listening
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The problem with active listening
Listening is an important skill to keep well-trained at any age. It’s important in romantic relationships, parent-child relationships, friendships, and more.
First, for any unfamiliar or hazy-of-memory: active listening is the practice of listening, actively. The “active” side of this comes in several parts:
- Asking helpful questions
- Giving feedback to indicate that the answer has been understood
- Prompting further information-giving
This can look like:
- A: How did you feel when that happened?
- B: My heart was racing and I felt panicked, it really shocked me
- A: It really shocked you?
- B: Yes, because it was so unexpected; I’d never imagined something like this happening
- A: You’d never expect something like that
- B: No, I mean, I had no reason to
And… As a superficial listening technique, it’s not terrible, and it has its place
But unfortunately, if it’s one’s only listening technique, one will very quickly start sounding like a Furby—that children’s toy from the 90s that allegedly randomly parroted fragments of things that had been said to it. In fact this was a trick of programming, but that’s beyond the scope of this article.
The point is: the above technique, if used indiscriminately and/or too often, starts to feel like talking to a very basic simulacrum.
Which is the opposite of feeling like being listened to!
A better way to listen
Start off similarly, but better.
Ask open questions, or otherwise invite sharing of information.
People can be resistant to stock phrases like “How did that make you feel?”, but this can be got around by simply changing it up, e.g.:
- “What was your reaction?” ← oblique but often elicits the same information
- “I’m not sure how I’d feel about that, in your shoes” ← not even a question, but shows active attention much better than the “mmhmm” noises of traditional active listening, and again prompts the same information
Express understanding… But better
People have been told “I understand” a lot, and often it’s code for “Stop talking”. So, avoid “I understand”. Instead, try:
- “I can understand that”
- “Understandable”
- “That makes sense”
Ask clarifying questions… Better
Sometimes, a clarifying question doesn’t have to have its own point, beyond prompting more sharing, and sometimes, an “open question” can be truly wide open, meaning that vaguer is better, such as:
- “Oh?”
- “How so?” ← this is the heavy artillery that can open up a lot
Know when to STFU
Something that good therapists (and also military interrogators) know: when to STFU
If someone is talking, don’t interrupt them. If you do, they might not start again, or might skip what they were going to say.
Interruption says “I think you’ve said all that needs to be said there”, or else, if the interruption was to ask one of the above questions, it says “you’re not doing a good enough job of talking”, and neither of those sentiments encourage people to share, nor do they make someone feel listened-to!
Instead, just listen. Passive listening has its place too! When there’s a break, then you can go to one of the above questions/prompts/expressions of understanding, as appropriate.
Judge not, lest they feel judged
Reserve judgement until the conversation is over, at the earliest. If asked for your judgement of some aspect, be as reassuring as you can. People feel listened-to when they don’t feel judged.
If they feel judged, conversely, they can often feel you didn’t listen properly, or else you’d be in agreement with them. So instead, just sit on it for as long as you can.
Note: that goes for positive judgements too! Sit on it. Expressing a positive judgement too soon can seem that you were simply eager to please, and can suggest insincerity.
If this seems simple, that’s because it is. But, try it, and see the difference.
Share This Post
-
The Best 4 Pool Exercises to Strengthen Your Core & Tone Up
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of people don’t love working on their core strength, but exercising in the pool can make it a lot more enjoyable, as well as minimizing risk of injury.
Dr Alyssa Kuhn, arthritis specialist, also advises “being in the water also helps to control for balance and can offload the joints so they aren’t as painful”:
The gentlest exercise
The specific exercises she recommends are:
Wood Chops
Stagger your feet, clasp your hands, and submerge them in the water. Now, move your hands diagonally from one side to the other. This engages your core and balance using water resistance. Perform 10–20 reps per side, exhaling on the hardest part.
Front Kick with Opposite Arm Press
Kick one leg forward while pushing the opposite arm out or overhead—higher kicks increase difficulty by requiring more balance. If balance isn’t sufficient for you yet, hold onto the pool wall if needed. Either way, engage the core to lift the leg. Do 20–30 reps alternating sides.
Wall Push-Ups
Place your hands on the pool wall, shoulder-width apart. Keep feet together and hips slightly tucked for core engagement. Next, move your chest toward the wall and push back while maintaining a straight body—avoid arching your back. Do 10–20 reps.
Arm Circles
Stand with your feet wider than shoulder-width. Clasp your hands, extend your arms, and submerge them in the water. Make large circular motions for resistance training. This can be done with straight or bent arms for different difficulty levels. Do 10–20 circles in each direction.
For more on each of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Osteoporosis & Exercises: Which To Do (And Which To Avoid)
Take care!
Share This Post
-
Do Hard Things – by Steve Magness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to say that we must push ourselves if we want to achieve worthwhile things—and it’s also easy to push ourselves into an early grave by overreaching. So, how to do the former, without doing the latter?
That’s what this book’s about. The author, speaking from a background in the science of sports psychology, applies his accumulated knowledge and understanding to the more general problems of life.
Most of us are, after all, not sportspeople or if we are, not serious ones. Those few who are, will get benefit from this book too! But it’s mostly aimed at the rest of us who are trying to work out whether/when we should scale up, scale back, change track, or double down:
- How much can we really achieve in our career?
- How about in retirement?
- Do we ever really get too old for athletic feats, or should we keep pressing on?
Magness brings philosophy and psychological science together, to help us sort our way through.
Nor is this just a pep talk—there’s readily applicable, practical, real-world advice here, things to enable us to do our (real!) best without getting overwhelmed.
The style is pop-science, very easy-reading, and clear and comprehensible throughout—without succumbing to undue padding either.
Bottom line: this is a very pleasant read, that promises to make life more meaningful and manageable at the same time. Highly recommendable!
Click here to check out Do Hard Things, and get the most out of life!
Share This Post
Related Posts
-
High-Protein Plant-Based Diet for Beginners – by Maya Howard with Ariel Warren
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Seasoned vegans (well-seasoned vegans?) will know that getting enough protein from a plant-based diet is really not the challenge that many think it is, but for those just embarking on cutting out the meat, it’s not useful to say “it’s easy!”; it’s useful to show how.
That’s what this book does. And not just by saying “these foods” and leaving people to wonder if they need to eat a pound of tofu each day to get their protein in. Instead, recipes. Enough for a 4-week meal plan, and the idea is that after a month of eating that way, it won’t be nearly so mysterious.
The recipes are very easy to execute, while still having plenty of flavor (which is what happens when one uses a lot of flavorsome main ingredients and then seasons them well too). The ingredients are not obscure, and you should be able to find everything easily in any medium-sized supermarket.
As for the well-roundedness of the diet, we’ll mention that the “with Ariel Warren” in the by-line means that while the book was principally authored by Maya Howard (who is, at time of writing, a nutritionist-in-training), she had input throughout from Ariel Warren (a Registered Dietician Nutritionist) to ensure she didn’t go off-piste anyway and it gets the professional stamp of approval.
Bottom line: if you’d like to cook plant based while still prioritizing protein and you’re not sure how to make that exciting and fun instead of a chore, then this book will show you how to please your taste buds and improve your body composition at the same time.
Click here to check out High-Protein Plant-Based Diet for Beginners, and dig in!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healthy Harissa Falafel Patties
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You can make these as regular falafel balls if you prefer, but patties are quicker and easier to cook, and are great for popping in a pitta.
You will need
For the falafels:
- 1 can chickpeas, drained, keep the chickpea water (aquafaba)
- 1 red onion, roughly chopped
- 2 tbsp chickpea flour (also called gram flour or garbanzo bean flour)
- 1 bunch parsley
- 1 tbsp harissa paste
- Extra virgin olive oil for frying
For the harissa sauce:
- ½ cup crème fraîche or plant-based equivalent (you can use our Plant-Based Healthy Cream Cheese recipe and add the juice of 1 lemon)*
- 1 tbsp harissa paste (or adjust this quantity per your heat preference)
*if doing this, rather than waste the zest of the lemon, you can add the zest to the falafels if you like, but it’s by no means necessary, just an option
For serving:
- Wholegrain pitta or other flatbread (you can use our Healthy Homemade Flatbreads recipe)
- Salad (your preference; we recommend some salad leaves, sliced tomato, sliced cucumber, maybe some sliced onion, that sort of thing)
Method
(we suggest you read everything at least once before doing anything)
1) Blend the chickpeas, 1 oz of the aquafaba, the onion, the parsley, and the harissa paste, until smooth. Then add in the chickpea flour until you get a thick batter. If you overdo it with the chickpea flour, add a little more of the aquafaba to equalize. Refrigerate the mixture for at least 30 minutes.
2) Heat some oil in a skillet, and spoon the falafel mixture into the pan to make the patties, cooking on both sides (you can use a spatula to gently turn them), and set them aside.
3) Mix the harissa sauce ingredients in a small bowl.
4) Assemble; best served warm, but enjoy it however you like!
Enjoy!
Want to learn more?
For those interested in more of what we have going on today:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Capsaicin For Weight Loss And Against Inflammation
- Hero Homemade Hummus ← another great option
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Sun Exposure Dilemma
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Sun Exposure Dilemma
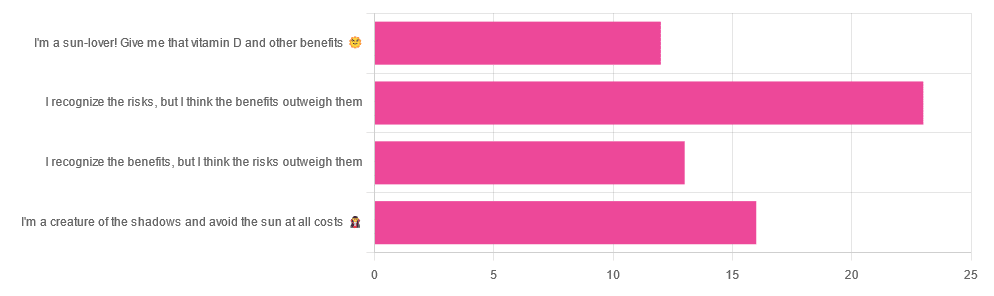
Yesterday, we asked you about your policy on sun exposure, and got the above-pictured, below-described, set of answers:
- A little over a third of respondents chose “I recognize the risks, but I think the benefits outweigh them”
- A quarter of respondents chose “I am a creature of the shadows and I avoid the sun at all costs”
- A little over a fifth of respondents chose “I recognize the benefits, but I think the risks outweigh them”
- A little under a fifth of respondents chose “I’m a sun-lover! Give me that vitamin D and other benefits!”
All in all, this is perhaps the most even spread of answers we’ve had for Friday mythbuster polls—though the sample size was smaller than it often is.
Of those who added comments, common themes were to mention your local climate, and the importance of sunscreen and/or taking vitamin D supplements.
One subscriber mentioned having lupus and living in Florida, which is a particularly unfortunate combination:
Lupus Foundation | Lupus & UV exposure: What you need to know
Another subscriber wrote:
❝Use a very good sunscreen with a high SPF all the time. Reapply after swimming or as needed! I also wear polarized sunglasses anytime I’m outside.❞
…which are important things to note too, and a lot of people forget!
See also: Who Screens The Sunscreens? (on fearing chemical dangers, vs the protection given)
But, onto today’s science for the topic at hand…
We need to get plenty of sun to get plenty of vitamin D: True or False?
True or False, depending on so many factors—to the point that many people get it wildly wrong in either direction.
Whether we are getting enough vitamin D depends on many circumstances, including:
- The climate (and depending on latitude, time of year) where we live
- Our genes, and especially (but not only) our skintone
- The clothes we wear (or don’t)
- Our diet (and not just “how much vitamin D do we consume”)
- Chronic diseases that affect vitamin D metabolism and/or requirements and/or sensitivity to the sun
For a rundown on these factors and more, check out:
Should I be getting my vitamin D levels checked?
Notably, on the topic of whether you should stay in the sun for longer to get more vitamin D…
❝The body can only produce a certain amount of vitamin D at the time, so staying in the sun any longer than needed (which could be just a few minutes, in a sunny climate) is not going to help increase your vitamin D levels, while it will increase your risk of skin cancer.❞
In contrast, she does also note:
❝During winter, catching enough sun can be difficult, especially if you spend your days confined indoors. Typically, the required exposure increases to two to three hours per week in winter. This is because sunlight exposure can only help produce vitamin D if the UVB rays reach us at the correct angle. So in winter we should regularly spend time outside in the middle of the day to get our dose of vitamin D.❞
See also: Vitamin D & Calcium: Too Much Of A Good Thing?
We can skip the sun and get our vitamin D from diet/supplements: True or False?
True! However, vitamin D is not the only health benefit of sun exposure.
Not only is sunlight-induced serotonin production important for many things ranging from mood to circadian rhythm (which in turn affects many other aspects of health), but also…
While too much sun can cause skin cancer, too little sun could cause other kinds of cancer:
Benefits of Sunlight: A Bright Spot for Human Health
Additionally, according to new research, the circadian rhythm benefits we mentioned above may also have an impact on type 2 diabetes:
Can catching some rays help you fight off type 2 diabetes?
Which way to jump?
A lot of it depends on who you are, ranging from the factors we mentioned earlier, to even such things as “having many moles” or “having blonde hair”.
This latter item, blonde hair, is a dual thing: it’s a matter of genetic factors that align with being prone to being more sensitive to the sun, as well as being a lesser physical barrier to the sun’s rays than dark hair (that can block some UV rays).
So for example, if two people have comparably gray hair now, but one of them used to have dark hair and the other blonde, there will still be a difference in how they suffer damage, or don’t—and yes, even if their skin is visually of the same approximate skintone.
You probably already know for yourself whether you are more likely to burn or tan in the sun, and the former group are less resistant to the sun’s damage… But the latter group are more likely to spend longer in the sun, and accumulate more damage that way.
If you’d like a very comprehensive downloadable, here are the guidelines issued by the UK’s National Institute for Health and Care Excellence:
NICE Guidelines | Sunlight exposure: risks and benefits
…and skip to “At risk groups”, if you don’t want to read the whole thing; “Skin type” is also an important subsection, which also uses your hair and eye color as indicators.
Writer’s note: genetics are complicated and not everyone will fall neatly into categories, which is why it’s important to know the individual factors.
For example, I am quite light-skinned with slightly graying dark hair and gray-blue eyes, and/but also have an obscure Sámi gene that means my skin makes vitamin D easily, while simultaneously being unusually resistant to burning (I just tan). Basically: built for the midnight sun of the Arctic circle.
And yet! My hobbies include not getting skin cancer, so I tend to still be quite mindful of UV levels in different weathers and times of day, and make choices (schedule, clothing, sunscreen or not) accordingly.
Bottom line:
That big self-perpetuating nuclear explosion in the sky is responsible for many things, good and bad for our health, so be aware of your own risk factors, especially for vitamin D deficiency, and skin cancer.
- If you have a predisposition to both, that’s unfortunate, but diet and supplementation at least can help with the vitamin D while getting modest amounts of sun at most.
- Remember that you can only make so much vitamin D at once, so sunbathing for health benefits need only take a few minutes
- Remember that sunlight is important for our circadian rhythm, which is important for many things.
- That’s governed by specific photoreceptor cells, though, so we don’t need our skin to be exposed for that; we just need to be able to see sunlight.
- If you’re going to be out in the sun, and not covered up, sunscreen is your friend, and yes, that goes for clear cold days under the winter sun too.
- Most phone weather apps these days have a UV index score as part of the data they give. Get used to checking it as often as you’d check for rain.
Stay safe, both ways around!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: