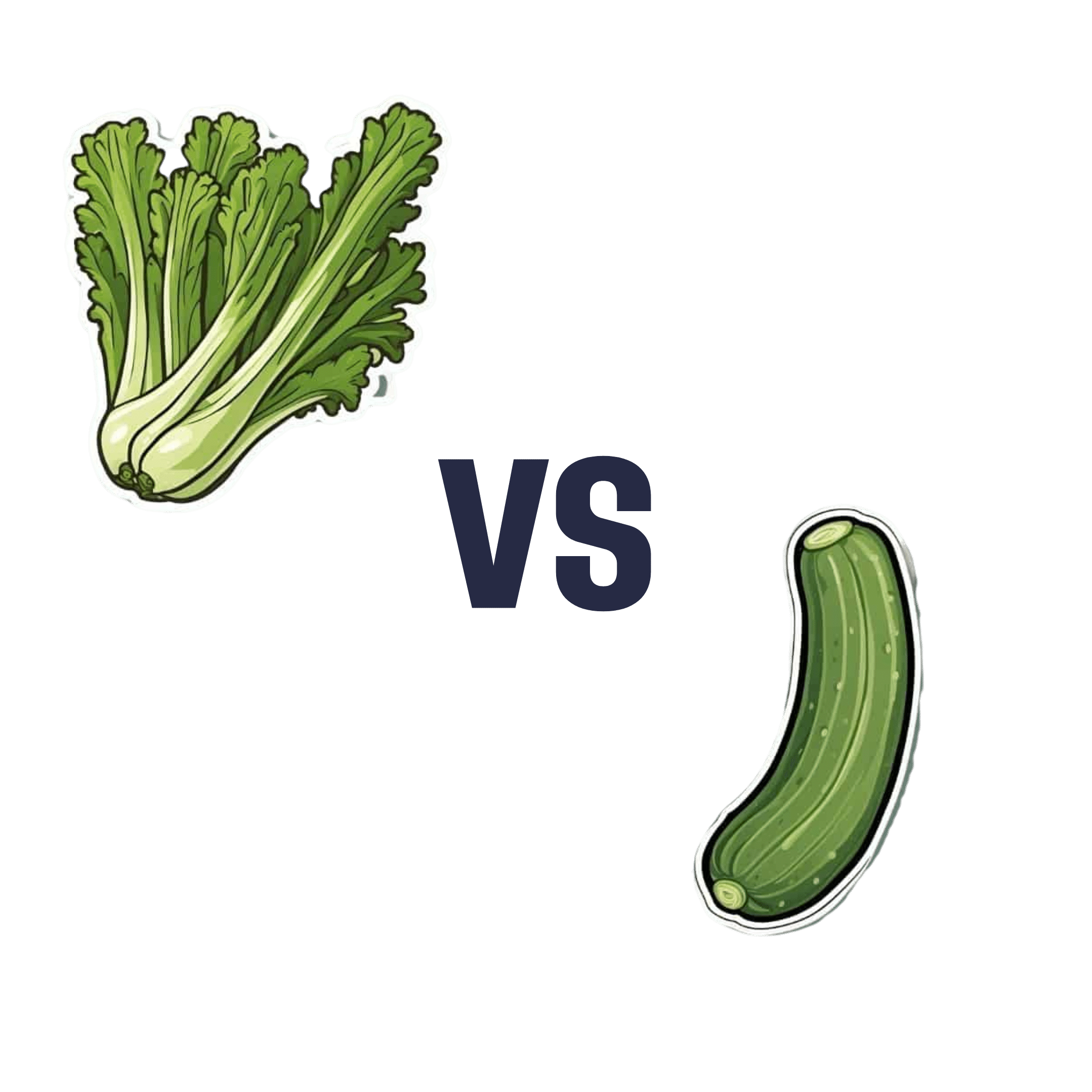
Celery vs Cucumber – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to cucumber, we picked the celery.
Why?
They are both great, of course! But celery came out on top:
Their macros are very comparable; they’re both 95% water with just enough other things to hold them together, and those other things are in approximately the same proportions in both celery and cucumber.
In the category of vitamins, however, celery has a lot more of vitamins A, B2, B3, B6, B9, E, and K, as well as slightly more vitamin C. Cucumber, meanwhile, only boasts slightly higher vitamin B1.
An easy win for celery on the vitamin front!
Minerals are closer, but celery still comes out on top with its notably higher calcium and potassium content. Cucumber has more iron and zinc, but the margin is smaller.
As a point in cucumber’s favor, it has been noted for its anti-inflammatory effect in ways that celery hasn’t, but we don’t think this is enough to say it wins over celery sweeping the vitamins category and coming out top for minerals too.
However! They are both great, so enjoy them both, of course.
Want to learn more?
You might like to read:
- Cucumber Extract Beats Glucosamine & Chondroitin… At 1/135th Of The Dose?!
- Some Surprising Truths About Hunger And Satiety ← both celery and cucumber are great for this
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Visceral Belly Fat & How To Lose It
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Visceral Belly Fat & How To Lose It
We’ve talked before about how waist circumference is a much more useful indicator of metabolic health than BMI.
So, let’s say you’ve a bit more around the middle than you’d like, but it stubbornly stays there. What’s going on underneath what you can see, why is it going on, and how can you get it to change?
What is visceral fat?
First, let’s talk about subcutaneous fat. That’s the fat directly under your skin. Women usually have more than men, and that’s perfectly healthy (up to a point); it’s supposed to be that way. We (women) will tend to accumulate this mostly in places such as our breasts, hips, and butt, and work outwards from there. Men will tend to put it on more to the belly and face.
Side-note: if you’re undergoing (untreated) menopause, the changes in your hormone levels will tend to result in more subcutaneous fat to the belly and face too. That’s normal, and/but normal is not always good, and treatment options are great (with hormone replacement therapy, HRT, topping the list).
Visceral fat (also called visceral adipose tissue), on the other hand, is the fat of the viscera—the internal organs of the abdomen.
So, this is fat that goes under your abdominal muscles—you can’t squeeze this (directly).
So what can we do?
Famously “you can’t do spot reduction” (lose fat from a particular part of your body by focusing exercises on that area), but that’s about subcutaneous fat. There are things you can do that will reduce your visceral fat in particular.
Some of these advices you may think “that’s just good advice for losing fat in general” and it is, yes. But these are things that have the biggest impact on visceral fat.
Cut alcohol use
This is the biggie. By numerous mechanisms, some of which we’ve talked about before, alcohol causes weight gain in general yes, but especially for visceral fat.
Get better sleep
You might think that hitting the gym is most important, but this one ranks higher. Yes, you can trim visceral fat without leaving your bed (and even without getting athletic in bed, for that matter). Not convinced?
- Here’s a study of 101 people looking at sleep quality and abdominal adiposity
- Oh, and here’s a meta-analysis with 56,000 people (finding the same thing), in case that one study didn’t convince you.
So, the verdict is clear: you snooze, you lose (visceral fat)!
Tweak your diet
You don’t have to do a complete overhaul (unless you want to), but a few changes can make a big difference, especially:
- Getting more fiber (this is the biggie when it comes to diet)
- Eating less sugar (not really a surprise, but relevant to mention)
- Eat whole foods (skip the highly processed stuff)
If you’d like to learn more and enjoy videos, here’s an informative one to get you going!
Click Here If The Embedded Video Doesn’t Load Automatically! Share This Post
-
What Different Kinds of Hair Loss/Thinning Say About Your Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Siobhan Deshauer shows us different kinds of hair loss, what causes them, and what can be done about them:
Many different causes
Here’s how to tell them apart:
- Alopecia areata is an autoimmune condition where the immune system mistakenly attacks hair follicles, causing hair loss that can occur at any age and affects about 1 in 50 people. It often presents as smooth patches of hair loss and can be treated with steroid injections. Severe cases may require high-dose prednisone, which can restore hair growth over time.
- Discoid lupus is an autoimmune disease that affects the skin, leading to inflammation, scarring, and permanent hair loss. Unlike alopecia areata, it causes visible damage to the scalp and hair follicles. This type of lupus typically does not involve internal organs, unlike systemic lupus.
- Telogen effluvium occurs when a major systemic shock, such as an infection, surgery, or significant stress, triggers many hair follicles to enter the resting phase simultaneously, resulting in delayed hair shedding. The condition is diagnosed with a “hair pull test” and is typically temporary, as the resting phase is followed by normal hair growth phases.
- Allergic reactions to products, such as hair dye containing PPD, can cause hair loss due to scalp irritation and inflammation. An allergic response may trigger hair follicles to enter a resting phase, leading to hair loss by the same mechanism as telogen effluvium. Treatment with steroids can calm the reaction, and hair usually regrows after recovery.
- Syphilis, a sexually transmitted infection, can present with varied symptoms, including hair loss in a distinct moth-eaten pattern. Hair loss due to syphilis is reversible and curable with penicillin treatment, with hair regrowth typically occurring a few months after treatment.
- Biotin deficiency is rare due to its production by gut bacteria and presence in foods such as nuts, seeds, and beans such as soybeans. Deficiency can result from excessive consumption of raw egg whites, which block absorption. Severe deficiency causes hair loss and skin issues but can be treated effectively with biotin supplements.
- Iron deficiency anemia can cause hair thinning along with symptoms like fatigue and breathlessness. It often results from inadequate dietary intake, but can also occur after heavy menstrual bleeding. Treatment with iron supplements, or blood transfusions in severe cases, can restore both hair and energy levels, leading to significant improvements.
- Trichotillomania is a psychological condition marked by an uncontrollable urge to pull out one’s hair, often associated with anxiety or depression. Hair patches may show different stages of regrowth. While it can be challenging to manage, the condition can be treated with appropriate psychological and medical support.
- Traction alopecia results from hairstyles that exert prolonged tension on the hair, causing it to thin or fall out. This type of hair loss can be prevented by reducing the strain on the hair. Loosening hairstyles and giving the scalp a break can help hair regrow over time.
- Hypothyroidism causes symptoms like fatigue, dry skin, and hair thinning due to insufficient thyroid hormone production—however, it can be managed with diet, and if necessary, thyroid medications.
- Zinc deficiency may also cause hair loss and a characteristic rash. Treatment with zinc supplements can significantly improve hair growth and other symptoms.
- Medications, such as chemotherapy drugs, Accutane, and anti-seizure medications like valproic acid, are known to cause hair loss as a side effect. This type of hair loss is often reversible once the medication is stopped.
- Male pattern hair loss, or androgenic alopecia, is influenced by testosterone and genetic risk factors—which, contrary to popular belief, can come from either or both sides of the family. Early onset, especially before age 40, is linked to an increased risk of heart disease. However, effective treatments are available, and early intervention is beneficial.
- Female pattern hair loss is basically the same thing as male pattern hair loss (indeed, it is literally still androgenic alopecia), just a) almost always much less severe and b) with a gender-appropriate name. It affects up to 40% of women by age 50 and is characterized by thinning hair at the top of the head. It’s related to hormonal imbalances involving testosterone, such as those seen in PCOS and menopause, amongst other less common causes. Early treatment can be effective, and research is ongoing to develop more targeted therapies.
Dr. Siobhan Deshauer advises, if you’re experiencing hair loss, to monitor other symptoms too if applicable, take photos for tracking, and consult a doctor early for diagnosis and potential treatment.
For more on all of this plus visual illustrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
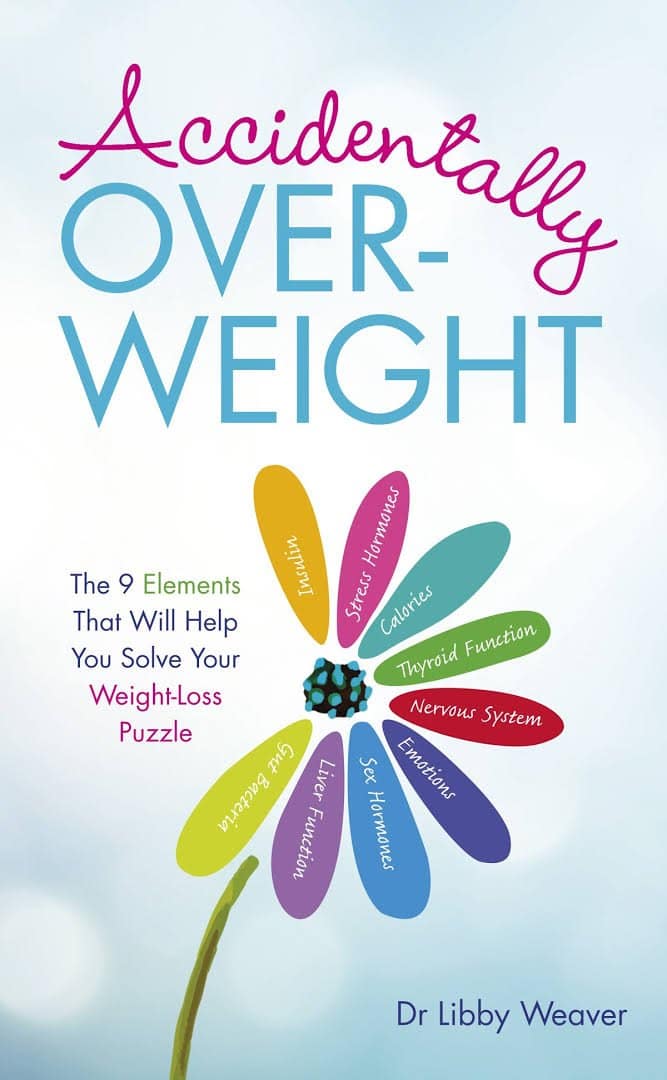
Accidentally Overweight – by Dr. Libby Weaver
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book’s main premise is that for most people who become overweight especially in midlife or later, if there wasn’t an obvious lifestyle change to precipitate this (e.g. started living on fast food for some reason), then in most cases, what’s needed is not drastic action, so much as some metabolic tweaks to correct things that have gone off-piste a little in our physiology.
The book covers nine factors that make an impact, and how each can be managed. They are:
- Insulin
- Stress hormones
- Calories
- Thyroid function
- Nervous system
- Emotions
- Sex hormones
- Liver function
- Gut bacteria
Some will be obvious, but as Dr. Weaver explains, are relative trivial compared to the others; “calories” in one such example of this “yes, it’s a factor, but very overrated” category.
Others are things that most people don’t think too much about, like liver function. And yet, it is indeed very much critical, and a major player in metabolism and adiposity.
The style is on the very light end of pop-science, but she does bring her professional knowledge to bear on topic (her doctorate is a PhD in biochemistry, so a lot of explanations come from that angle).
Bottom line: if you’ve found yourself “accidentally overweight”, and would like to tip the scales back in the other direction without doing anything extreme, then this book provides the tweaks that no amount of cardio or restrictive dieting will.
Click here to check out Accidentally Overweight, and re-adjust it back the other way!
Share This Post
Related Posts
-
Wanna read more?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You’ve Got Questions? We’ve Got Answers!
Q: Tips for reading more and managing time for it?
A: We talked about this a little bit in yesterday’s edition, so you may have seen that, but aside from that:
- If you don’t already have one, consider getting a Kindle or similar e-reader. They’re very convenient, and also very light and ergonomic—no more wrist strain as can occur with physical books. No more eye-strain, either!
- Consider making reading a specific part of your daily routine. A chapter before bed can be a nice wind-down, for instance! What’s important is it’s a part of your day that’ll always, or at least almost always, allow you to do a little reading.
- If you drive, walk, run, or similar each day, a lot of people find that’s a great time to listen to an audiobook. Please be safe, though!
- If your lifestyle permits such, a “reading retreat” can be a wonderful vacation! Even if you only “retreat” to your bedroom, the point is that it’s a weekend (or more!) that you block off from all other commitments, and curl up with the book(s) of your choice.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
ADHD… As An Adult?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ADHD—not just for kids!
Consider the following:
- If a kid has consistent problems paying attention, it’s easy and common to say “Aha, ADHD!”
- If a young adult has consistent problems paying attention, it’s easy and common to say “Aha, a disinterested ne’er-do-well!”
- If an older adult has consistent problems paying attention, it’s easy and common to say “Aha, a senior moment!”
Yet, if we recognize that ADHD is fundamentally a brain difference in children (and we do; there are physiological characteristics that we can test), and we can recognize that as people get older our brains typically have less neuroplasticity (ability to change) than when we are younger rather than less, then… Surely, there are just as many adults with ADHD as kids!
After all, that rather goes with the linear nature of time and the progressive nature of getting older.
So why do kids get diagnoses so much more often than adults?
Parents—and schools—can find children’s ADHD challenging, and it’s their problem, so they look for an explanation, and ADHD isn’t too difficult to find as a diagnosis.
Meanwhile, adults with ADHD have usually developed coping mechanisms, have learned to mask and/or compensate for their symptoms, and we expect adults to manage their own problems, so nobody’s rushing to find an explanation on their behalf.
Additionally, the stigma of neurodivergence—especially something popularly associated with children—isn’t something that many adults will want for themselves.
But, if you have an ADHD brain, then recognizing that (even if just privately to yourself) can open the door to much better management of your symptoms… and your life.
So what does ADHD look like in adults?
ADHD involves a spread of symptoms, and not everyone will have them all, or have them in the same magnitude. However, very commonly most noticeable traits include:
- Lack of focus (ease of distraction)
- Conversely: high focus (on the wrong things)
- To illustrate: someone with ADHD might set out to quickly tidy the sock drawer, and end up Marie Kondo-ing their entire wardrobe… when they were supposed to doing something else
- Conversely: high focus (on the wrong things)
- Poor time management (especially: tendency to procrastinate)
- Forgetfulness (of various kinds—for example, forgetting information, and forgetting to do things)
Want To Take A Quick Test? Click Here ← this one is reputable, and free. No sign in required; the test is right there.
Wait, where’s the hyperactivity in this Attention Deficit Hyperactivity Disorder?
It’s often not there. ADHD is simply badly-named. This stems from how a lot of mental health issues are considered by society in terms of how much they affect (and are observable by) other people. Since ADHD was originally noticed in children (in fact being originally called “Hyperkinetic Reaction of Childhood”), it ended up being something like:
“Oh, your brain has an inconvenient relationship with dopamine and you are driven to try to correct that by shifting attention from boring things to stimulating things? You might have trouble-sitting-still disorder”
Hmm, this sounds like me (or my loved one); what to do now at the age of __?
Some things to consider:
- If you don’t want medication (there are pros and cons, beyond the scope of today’s article), you might consider an official diagnosis not worth pursuing. That’s fine if so, because…
- More important than whether or not you meet certain diagnostic criteria, is whether or not the strategies recommended for it might help you.
- Whether or not you talk to other people about it is entirely up to you. Maybe it’s a stigma you’d rather avoid… Or maybe it’ll help those around you to better understand and support you.
- Either way, you might want to learn more about ADHD in adults. Today’s article was about recognizing it—we’ll write more about managing it another time!
In the meantime… We recommended a great book about this a couple of weeks ago; you might want to check it out:
Click here to see our review of “The Silent Struggle: Taking Charge of ADHD in Adults”!
Note: the review is at the bottom of that page. You’ll need to scroll past the video (which is also about ADHD) without getting distracted by it and forgetting you were there to see about the book. So:
- Click the above link
- Scroll straight to the review!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
On This Bright Day – by Dr. Susan Thompson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is principally aimed at those who have struggled with emotional/comfort eating, over-eating, and/or compulsive eating of some kind.
However, its advices go for the “little compulsions” too, the many small unhealthy choices that add up. Thus, this book has value for most if not all of us.
The format is: each day has a little quotation, followed by a short discussion of that, which is then underlined by an affirmation for the day.
The main thrust of the book is to promote mindful eating, and it does this well with daily reminders that are helpful without being preachy.
Bottom line: if you enjoy “daily reader” type books and would like a daily reminder to practice mindful eating, then this book is for you!
Click here to check out On This Bright Day, and enjoy your food mindfully, every day!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: