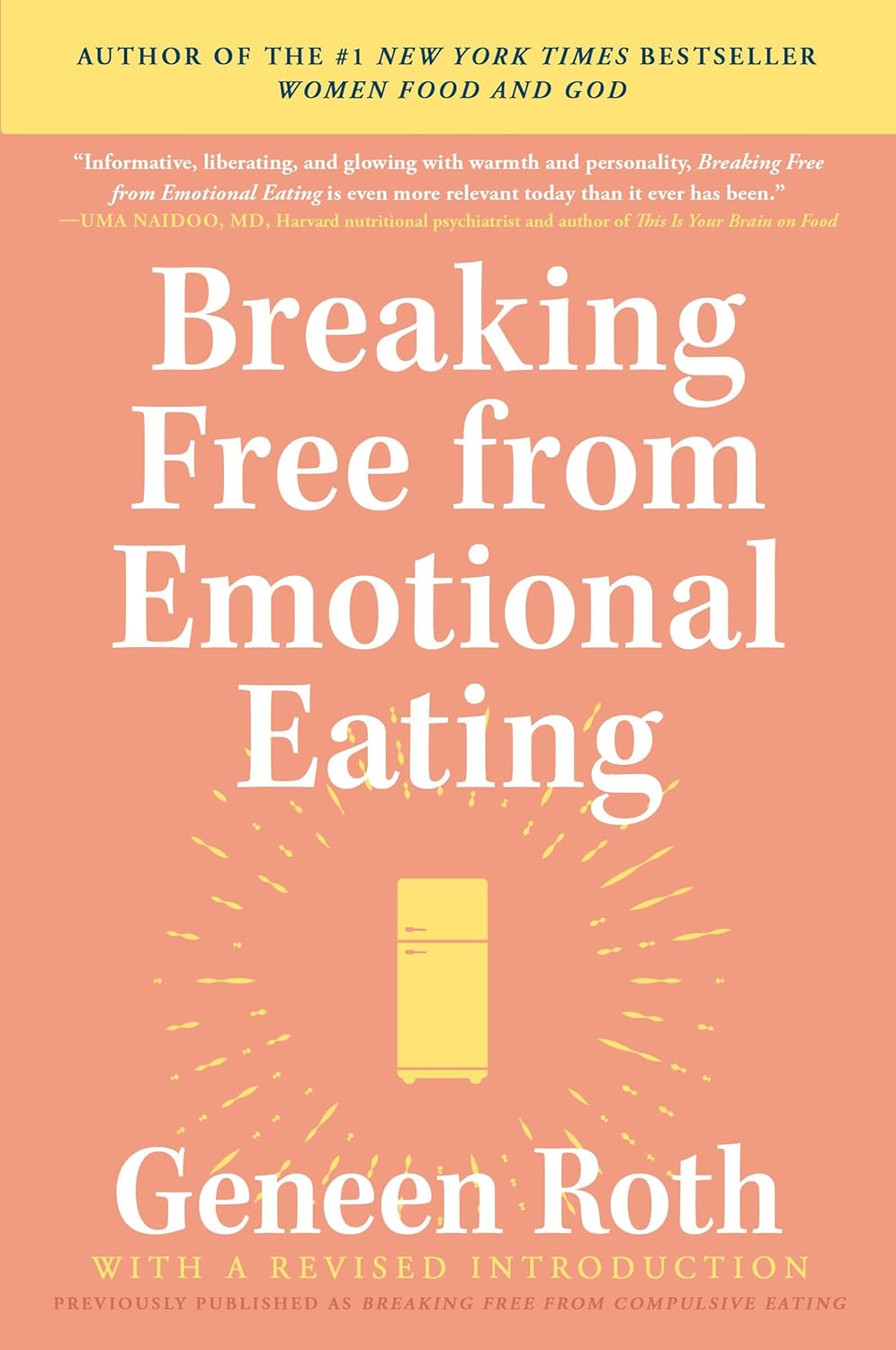
Breaking Free from Emotional Eating – Geneen Roth
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The isn’t a book about restrictive dieting, or even willpower. Rather, it’s about making the unconscious conscious, and changing your relationship with food from being one of compulsion, to one of choice, wherein you also get the choice of saying “no”.
Roth takes us through the various ways in which life seems to conspire to take consciousness away from eating, from obvious distractions such as TV, to less obvious ones, like “it doesn’t count if you’re not sitting down”. She also tackles other psychological aspects, such as those people get from parents—which can be a big factor for many.
Importantly, she teaches us that when it comes to “have your cake and eat it”, you can also, in fact, have your cake and not eat it. That’s an option too. Its mere presence in our house is not the boss of us. However, overcoming the “this then that” automatic process that goes from having to eating, is something that Roth gives quite some attention to, offering a number of reframes to make it a lot easier.
The style is friendly, conversational, pop-science, and the format dates it a little—this is very much a book formatted the way pop-science books were formatted 20–50 years ago (the book itself is from 2003, for what it’s worth). However, a lack of modern format doesn’t take away from its very valuable insights, and if anything, the older format rather promotes reading a book from cover to cover, which can be beneficial.
Bottom line: if emotional or compulsive eating is something that you’ve found tricky to overcome, then this book can help make it a lot easier.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chromium Picolinate For Blood Sugar Control & Weight Loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, a quick disambiguation:
- chromium found in food, trivalent chromium of various kinds, is safe (in the quantities usually consumed) and is sometimes considered an essential mineral, sometimes considered unnecessary but beneficial. It’s hard to know for sure, since it’s in a lot of foods (naturally, like many trace elements)
- chromium found in pollution, hexavalent chromium (so: twice as many cationic bonds, if this writer’s chemistry serves her correctly) is poisonous.
We’re going to be writing about the food kind, which is also possible to take as a supplement.
In this case, supplementing vs getting from food is quite a big difference, by the way, since (unlike for a lot of things, which are often the other way around) the bioavailability of chromium from food is very low (around 2.5%), whereas chromium picolinate, one of the most commonly-used supplement forms, boasts higher bioavailability.
Does it work for blood sugars?
Yes, it does! At least, it does in the case of people with type 2 diabetes. Rather than bombard you with many individual studies, here’s a systematic review and meta-analysis of 22 criteria-meeting randomized clinical trials that found:
❝The available evidence suggests favourable effects of chromium supplementation on glycaemic control in patients with diabetes.
Chromium monosupplement may additionally improve triglycerides and HDL-C levels.❞
Type 1 diabetes does not have anything like the same weight of evidence, and indeed,
we couldn’t find a single human study. It was beneficial for mice with artificially-induced T1D, thoughwait no, we have an update! We found literally a single human study:Chromium picolinate supplementation for diabetes mellitus
Literally, as in: it’s a case study of one person, and the results were a modest reduction in Hb A1c levels after 3 months of 600μg daily; the researchers concluded that ❝chromium picolinate continues to fall squarely within the scope of “alternative medicine,” with both unproven benefits and unknown risks❞.
As for people without diabetes, it may reduce the risk of diabetes:
Risk of Type 2 Diabetes Is Lower in US Adults Taking Chromium-Containing Supplements
However! This was an observational study, and correlation ≠ causation.
Furthermore, they said:
❝Over one-half the adult US population consumes nutritional supplements, and over one-quarter consumes supplemental chromium. The odds of having T2D were lower in those who, in the previous 30 d, had consumed supplements containing chromium❞
That “over one-quarter consumes supplemental chromium” brought our attention to the fact that this is not talking about specifically chromium “monosupplements” (definitely not quarter of the adult population take those), but rather, “multivitamin and mineral” supplements that also contain a tiny amount (often under 50μg) of chromium.
In other words, this ruins the data and honestly the benefit could have been from anything in the “multivitamin and mineral” supplement, or indeed, could just be “the kind of person who takes supplements is the kind of person who lives a lifestyle that is less conducive to becoming diabetic”.
Does it work for weight loss?
We’re running out of space here, so we’ll be brief:
No.
There are many papers that have concluded this, but here are two:
Chromium picolinate supplementation for overweight or obese adults
and
Is it safe?
Science’s current best answer is “we don’t know; it hasn’t been tested enough; we haven’t even established the tolerable upper limit, which is usually step 1 of establishing safety”.
Nor is there an estimated average requirement (if indeed there even is a requirement, which question is also not as yet answered conclusively by science), and science falls back to “here’s an average of what people consume in their diet, so that’s probably safe, we guess”.
(that average was reckoned as 25μg/day for young women and 25μg/day for young men, by the way; older ages not as yet reckoned)
You can read about this sorry state of affairs here.
Want to try some?
Notwithstanding the above lack of data for safety, it does have benefits for blood sugars, so if that’s a gamble you’re willing to make, then here’s an example product on Amazon.
Note: the dosage per capsule there (800μg) is half of the low end of the dose that was implicated in the serious kidney condition caused in this case study (1200–2400μg), so if you are going to try it, we strongly recommend not taking more than one per day.
Take care!
Share This Post
-
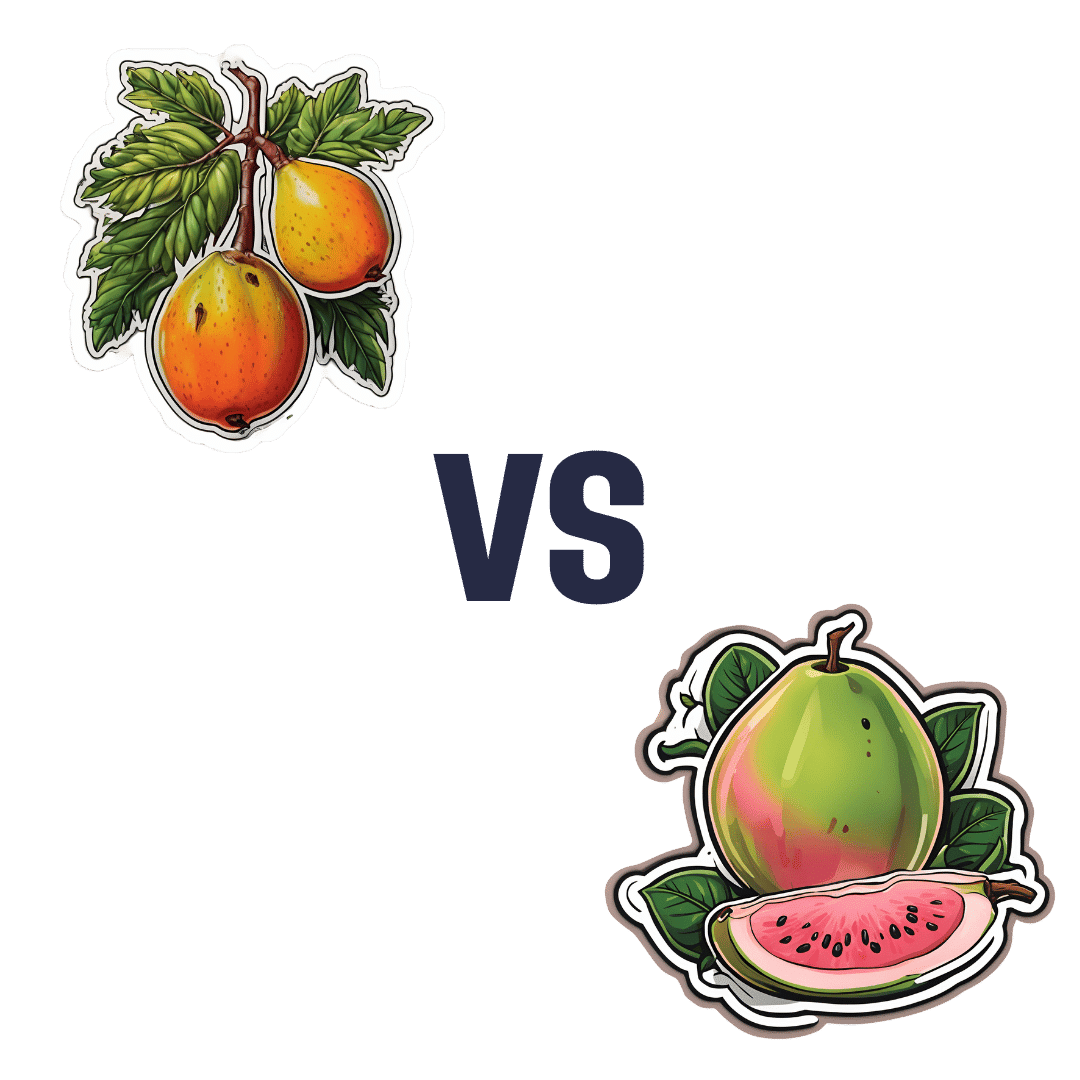
Mango vs Guava – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mango to guava, we picked the guava.
Why?
Looking at macros first, these two fruits are about equal on carbs (nominally mango has more, but it’s by a truly tiny margin), while guava has more than 3x the protein and more than 3x the fiber. A clear win for guava.
In terms of vitamins, mango has more of vitamins A, E, and K, while guava has more of vitamins B1, B2, B3, B5, B7, B9, and C. Another win for guava.
In the category of minerals, mango is not higher in any minerals, while guava is higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc.
In short, enjoy both; both are healthy. But if you’re choosing one, there’s a clear winner here, and it’s guava.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Share This Post
-
Seriously Useful Communication Skills!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Are Communication Skills, Really?
Superficially, communication is “conveying an idea to someone else”. But then again…
Superficially, painting is “covering some kind of surface in paint”, and yet, for some reason, the ceiling you painted at home is not regarded as equally “good painting skills” as Michaelangelo’s, with regard to the ceiling of the Sistine Chapel.
All kinds of “Dark Psychology” enthusiasts on YouTube, authors of “Office Machiavelli” handbooks, etc, tell us that good communication skills are really a matter of persuasive speaking (or writing). And let’s not even get started on “pick-up artist” guides. Bleugh.
Not to get too philosophical, but here at 10almonds, we think that having good communication skills means being able to communicate ideas simply and clearly, and in a way that will benefit as many people as possible.
The implications of this for education are obvious, but what of other situations?
Conflict Resolution
Whether at work or at home or amongst friends or out in public, conflict will happen at some point. Even the most well-intentioned and conscientious partners, family, friends, colleagues, will eventually tread on our toes—or we, on theirs. Often because of misunderstandings, so much precious time will be lost needlessly. It’s good for neither schedule nor soul.
So, how to fix those situations?
I’m OK; You’re OK
In the category of “bestselling books that should have been an article at most”, a top-tier candidate is Thomas Harris’s “I’m OK; You’re OK”.
The (very good) premise of this (rather padded) book is that when seeking to resolve a conflict or potential conflict, we should look for a win-win:
- I’m not OK; you’re not OK ❌
- For example: “Yes, I screwed up and did this bad thing, but you too do bad things all the time”
- I’m OK; you’re not OK ❌
- For example: “It is not I who screwed up; this is actually all your fault”
- I’m not OK; you’re OK ❌
- For example: “I screwed up and am utterly beyond redemption; you should immediately divorce/disown/dismiss/defenestrate me”
- I’m OK; you’re OK ✅
- For example: “I did do this thing which turned out to be incorrect; in my defence it was because you said xyz, but I can understand why you said that, because…” and generally finding a win-win outcome.
So far, so simple.
“I”-Messages
In a conflict, it’s easy to get caught up in “you did this, you did that”, often rushing to assumptions about intent or meaning. And, the closer we are to the person in question, the more emotionally charged, and the more likely we are to do this as a knee-jerk response.
“How could you treat me this way?!” if we are talking to our spouse in a heated moment, perhaps, or “How can you treat a customer this way?!” if it’s a worker at Home Depot.
But the reality is that almost certainly neither our spouse nor the worker wanted to upset us.
Going on the attack will merely put them on the defensive, and they may even launch their own counterattack. It’s not good for anyone.
Instead, what really happened? Express it starting with the word “I”, rather than immediately putting it on the other person. Often our emotions require a little interrogation before they’ll tell us the truth, but it may be something like:
“I expected x, so when you did/said y instead, I was confused and hurt/frustrated/angry/etc”
Bonus: if your partner also understands this kind of communication situation, so much the better! Dark psychology be damned, everything is best when everyone knows the playbook and everyone is seeking the best outcome for all sides.
The Most Powerful “I”-Message Of All
Statements that start with “I” will, unless you are rules-lawyering in bad faith, tend to be less aggressive and thus prompt less defensiveness. An important tool for the toolbox, is:
“I need…”
Softly spoken, firmly if necessary, but gentle. If you do not express your needs, how can you expect anyone to fulfil them? Be that person a partner or a retail worker or anyone else. Probably they want to end the conflict too, so throw them a life-ring and they will (if they can, and are at least halfway sensible) grab it.
- “I need an apology”
- “I need a moment to cool down”
- “I need a refund”
- “I need some reassurance about…” (and detail)
Help the other person to help you!
Everything’s best when it’s you (plural) vs the problem, rather than you (plural) vs each other.
Apology Checklist
Does anyone else remember being forced to write an insincere letter of apology as a child, and the literary disaster that probably followed? As adults, we (hopefully) apologize when and if we mean it, and we want our apology to convey that.
What follows will seem very formal, but honestly, we recommend it in personal life as much as professional. It’s a ten-step apology, and you will forget these steps, so we recommend to copy and paste them into a Notes app or something, because this is of immeasurable value.
It’s good not just for when you want to apologize, but also, for when it’s you who needs an apology and needs to feel it’s sincere. Give your partner (if applicable) a copy of the checklist too!
- Statement of apology—say “I’m sorry”
- Name the offense—say what you did wrong
- Take responsibility for the offense—understand your part in the problem
- Attempt to explain the offense (not to excuse it)—how did it happen and why
- Convey emotions; show remorse
- Address the emotions/damage to the other person—show that you understand or even ask them how it affected them
- Admit fault—understand that you got it wrong and like other human beings you make mistakes
- Promise to be better—let them realize you’re trying to change
- Tell them how you will try to do it different next time and finally
- Request acceptance of the apology
Note: just because you request acceptance of the apology doesn’t mean they must give it. Maybe they won’t, or maybe they need time first. If they’re playing from this same playbook, they might say “I need some time to process this first” or such.
Want to really superpower your relationship? Read this together with your partner:
Hold Me Tight: Seven Conversations for a Lifetime of Love, and, as a bonus:
The Hold Me Tight Workbook: A Couple’s Guide for a Lifetime of Love
Share This Post
- I’m not OK; you’re not OK ❌
Related Posts
-
Is it OK if my child eats lots of fruit but no vegetables?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Does it seem like most vegetables you serve your children end up left on the plate, or worse, strewn across the floor? But mention dessert, and your fruit skewers are polished off in an instant.
Or maybe the carrot and cucumber sticks keep coming home in your child’s lunchbox untouched, yet the orange slices are nowhere to be seen.
If you’re facing these struggles with your child, you’re not alone. Many children prefer fruit to vegetables.
So if your child eats lots of fruit but minimal or no vegetables, is that OK? And how can you get them to eat more veggies?
Children have an innate preference for fruit
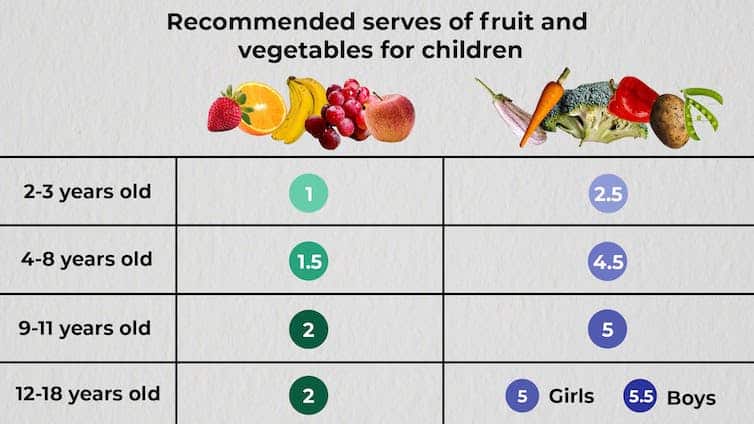
The Australian Dietary Guidelines’ recommended daily intakes for vegetables and fruit depend on a child’s age.
Fruit and vegetable serving sizes by age. The Conversation.
National Health and Medical Research Council, CC BY-SAConsumption among Australian children falls well below recommendations. Around 62.6% of children aged over two meet the recommended daily fruit intake, but only 9% meet the recommended vegetable intake.
This is not surprising given children have a natural preference for fruit. At least in part, this is due to its sweetness and texture, whether crispy, crunchy or juicy. The texture of fruit has been linked to a positive sensory experience among children.
Vegetables, on the other hand, are more of an acquired taste, and certain types, such as cruciferous vegetables, can be perceived by children as bitter.
The reason children often prefer fruit over vegetables could also be related to the parents’ preferences. Some research has even suggested we develop food preferences before birth based on what our mother consumes during pregnancy.
Balance is key
So, a preference for fruit is common. But is it OK if your child eats lots of fruit but little to no vegetables? This is a question we, as dietitians, get asked regularly.
You might be thinking, at least my child is eating fruit. They could be eating no veggies and no fruit. This is true. But while it’s great your child loves fruit, vegetables are just as important as part of a balanced eating pattern.
Vegetables provide us with energy, essential vitamins and minerals, as well as water and fibre, which help keep our bowels regular. They also support a strong immune system.
If your child is only eating fruit, they are missing some essential nutrients. But the same is true if they are eating only veggies.
Fruit likewise provides the body with a variety of essential vitamins and minerals, as well as phytochemicals, which can help reduce inflammation.
Evidence shows healthy consumption of fruit and vegetables protects against chronic diseases including high blood pressure, heart disease and stroke.
Consumed together, fruit and vegetables in a variety of colours provide different nutrients we need, some of which we can’t get from other foods. We should encourage kids to eat a “rainbow” of fruit and vegetables each day to support their growth and development.
What if my child eats too much fruit?
If your child is eating slightly more fruit than what’s recommended each day, it’s not usually a problem.
Fruit contains natural sugar which is good for you. But too much of a good thing, even if it’s natural, can create problems. Fruit also contains virtually no fat and very little to no protein, both essential for a growing child.
When overindulging in fruit starts to displace other food groups such as vegetables, dairy products and meat, that’s when things can get tricky.
6 tips to get your kids to love vegetables
1. Get them involved
Take your child with you when you go shopping. Let them choose new vegetables. See if you can find vegetables even you haven’t tried, so you’re both having a new experience. Then ask them to help you with preparing or cooking the vegetables using a recipe you have chosen together. This will expose your child to veggies in a positive way and encourage them to eat more.
2. Sensory learning
Try to expose your child to vegetables rather than hiding them. Kids are more likely to eat veggies when they see, smell and feel them. This is called sensory learning.
3. Have fun with food
Use colourful vegetables of different sizes and textures. Make them fun by creating scenes or faces on your child’s plate. Add edible flowers or mint for decoration. You can even serve this with a side of veggie-based dip such as hummus or guacamole for some bonus healthy fats.
4. Teach them to grow their own
Teach your child how to grow their own vegetables. Evidence shows kids are more inclined to try the food they have helped and watched grow. You don’t need to have a big backyard to do this. A windowsill with a pot plant is a perfect start.
5. Lead by example
Your child learns from you, and your eating habits will influence theirs. Ensure they see you eating and enjoying veggies, whether in meals or as snacks.
6. Practise persistence
If your child refuses a particular vegetable once, don’t give up. It can take many attempts to encourage children to try a new food.
Yasmine Probst, Associate Professor, School of Medical, Indigenous and Health Sciences, University of Wollongong; Olivia Wills, Accredited Practising Dietitian, PhD candidate, University of Wollongong, and Shoroog Allogmanny, Accredited Practising Dietitian, PhD candidate, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Gut-Healthy Tacos
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Full of prebiotics and probiotics, healthy fats, colorful salad boasting vitamins and minerals aplenty, and of course satisfying protein too, these tacos are also boasting generous flavors to keep you coming back for more…
You will need
- 24 sardines—canned is fine (if vegetarian/vegan, substitute tempeh and season generously; marinade if you have time)
- 12 small wholewheat tortillas
- 1 14oz/400g can black beans, drained
- 1 ripe avocado, stoned and cut into small chunks
- 1 red onion, thinly sliced
- 1 little gem lettuce, shredded
- 12 cherry tomatoes, halved
- 1 bulb garlic, crushed
- 1 lemon, sliced
- 4 tbsp plain unsweetened yogurt (your choice what kind, but something with a live culture is best)
- 3oz pickled jalapeños, roughly chopped
- 1oz cilantro (or substitute parsley if you have the cilantro-tastes-like-soap gene), finely chopped
- 1 tbsp extra virgin olive oil
- 2 tsp black pepper
- 1 tsp smoked paprika
- Juice of 1 lime
- Optional: Tabasco sauce, or similar hot sauce
Method
(we suggest you read everything at least once before doing anything)
1) Preheat your oven to a low temperature; 200℉ or just under 100℃ is fine
2) Place the lemon slices on top of the sardines on top of foil on a baking tray; you want the foil to be twice as much as you’d expect to need, because now you’re going to fold it over and make a sort of sealed envelope. You could use a dish with a lid yes, but this way is better because there’s going to be less air inside. Upturn the edges of the envelope slightly so that juices won’t run out, and make sure the foil is imperfectly sealed so a little steam can escape but not much at a time. This will ensure it doesn’t dry out, while also ensuring your house doesn’t smell of fish. Put all this into the oven on a middle shelf.
3) Mix the lime juice with the onion in a bowl, and add the avocado and tomatoes, mixing gently. Add half the cilantro, and set aside.
4) Put the black beans in a sieve and pour boiling water over them to refresh and slightly warm them. Tip them into a bowl and add the olive oil, black pepper, and paprika. Mix thoroughly with a fork, and no need to be gentle this time; in fact, deliberately break the beans a little in this case.
5) Mix the yogurt, jalapeños, garlic, and remaining cilantro in a small bowl.
6) Get the warmed sardines from the oven; discard the lemon slices.
7) Assemble! We recommend the order: tortilla, lettuce, fish (2 per taco), black bean mixture, salad mixture, garlic jalapeño yogurt mixture. You can also add a splash of the hot sauce per your preference, or if catering for more people, let people add their own.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- We Are Such Stuff As Fish Are Made Of
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Making Friends With Your Gut (You Can Thank Us Later)
- Our Top 5 Spices: How Much Is Enough For Benefits?
- Enjoy Pungent Polyphenols For Your Heart & Brain
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
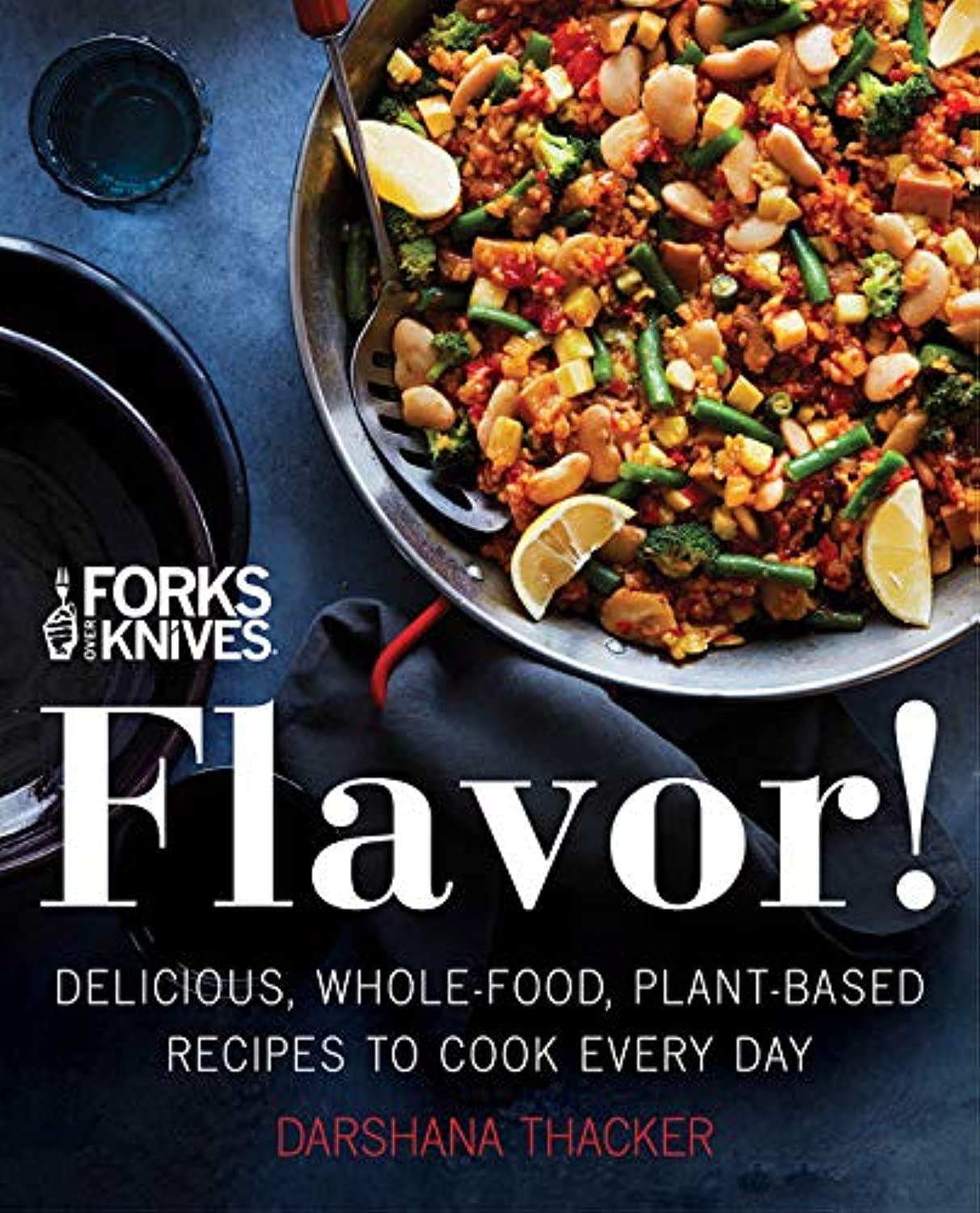
Forks Over Knives: Flavor! – by Darshana Thacker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s important to not have to choose too much between health and flavor, because the outcome will never be a good one, either for your health or your happiness. And what’s bad for your happiness will ultimately not work out and thus will be bad for your general health, so, the question becomes: how to get both?
This book handles that nicely, delivering plant-based dishes that are also incidentally oil-free, and also either gluten-free or else there’s an obvious easy substitution to make it such. The flavor here comes from the ingredients as a whole, including the main ingredients as well as seasonings.
On the downside, occasionally those ingredients may be a little obscure if you don’t live in, say, San Francisco, and the ingredients weren’t necessarily chosen for cooking on a budget, either.
However, in most cases for most people it will, at worse, inspire you to try using an ingredient you don’t usually use—so that’s a good result.
The recipes are very clear and easy to follow, although not all are illustrated, and the “ready in…” times are about as accurate as they are for any cookbook, that is to say, it’s the time in which it conceivably can be done if (like the author, a head chef) you have a team of sous-chefs who have done a bunch of prep for you (e.g. sweet potato does not normally come in ½” dice; it comes in sweet potatoes) and laid everything out in little bowls mise-en-place style, and also you know the procedure well enough to not have to stop, hesitate, check anything, wash anything, wait for water to boil or anything else to heat up, or so forth. In other words, if you’re on your own in your home kitchen with normal domestic appliances, it’s going to take a little longer than for a professional in a professional kitchen with professional help.
But don’t let that detract from the honestly very good recipes.
Bottom line: if you’d like to level-up your plant-based cooking, this will definitely make your dishes that bit better!
Click here to check out Forks Over Knives: Flavor!, and dig in!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: