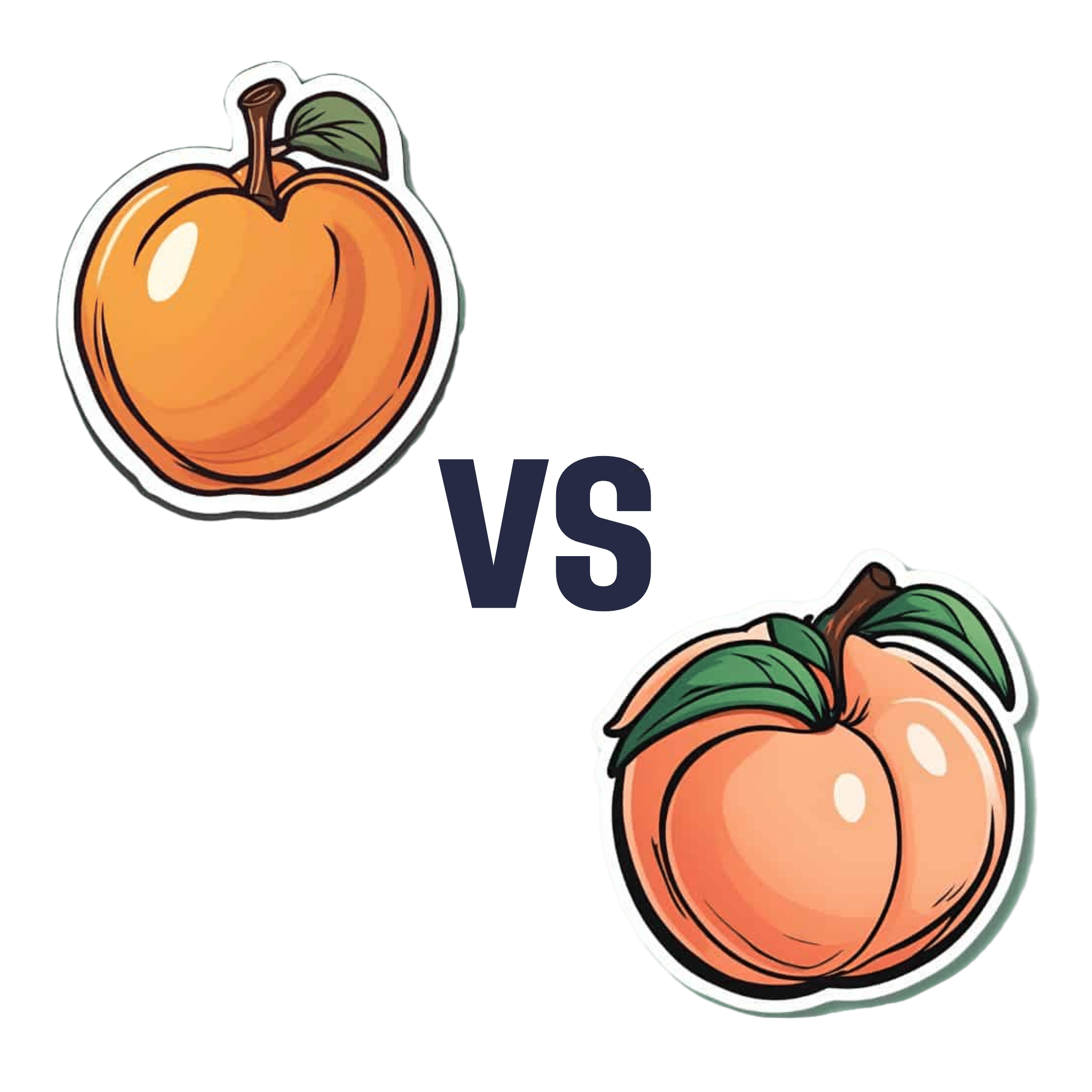
Apricots vs Peaches – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apricots to peaches, we picked the apricots.
Why?
Both are great! But there’s a clear winner:
In terms of macros, apricots have more fiber and, which is less important because the numbers are small, more protein. Apricots do also have more carbs, and/but carbs from whole fruit are not a problem for most people (especially because of the fiber), unless undertaking a very carb-controlled diet.
When it comes to vitamins, apricots sweep with more of vitamins A, B1, B2, B5, B6, B9, C, E, & K. Peaches meanwhile boast more vitamin B3, and that only marginally, as well as more choline.
In the category of minerals, apricots sweep again with more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. Peaches are not higher in any minerals.
Finally, if we consider polyphenols, apricots sweep yet again. The flavonols that peaches have, apricots have more of, and apricots have a long list of flavonols that peaches don’t.
Outside of flavonols, there is one (1) phenolic acid that peaches have more of (it’s 3-Caffeoylquinic acid), and it’s only slightly more, and it’s mostly in the skin which isn’t included if you buy your fruit ready-chopped. So in those cases, apricots would have the higher 3-Caffeoylquinic acid content anyway.
All in all, with their higher content of fiber, vitamins, minerals, and polyphenols, apricots easily win the day.
Enjoy both, though! Diversity is healthy!
Want to learn more?
You might like to read:
- Dried Apricots vs Dried Prunes – Which is Healthier?
- Which Sugars Are Healthier, And Which Are Just The Same? ← we know we link this one a lot, but we think it’s important for everyone to know how fruit is good and juice isn’t (and why, less that seem bizarrely arbitrary)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
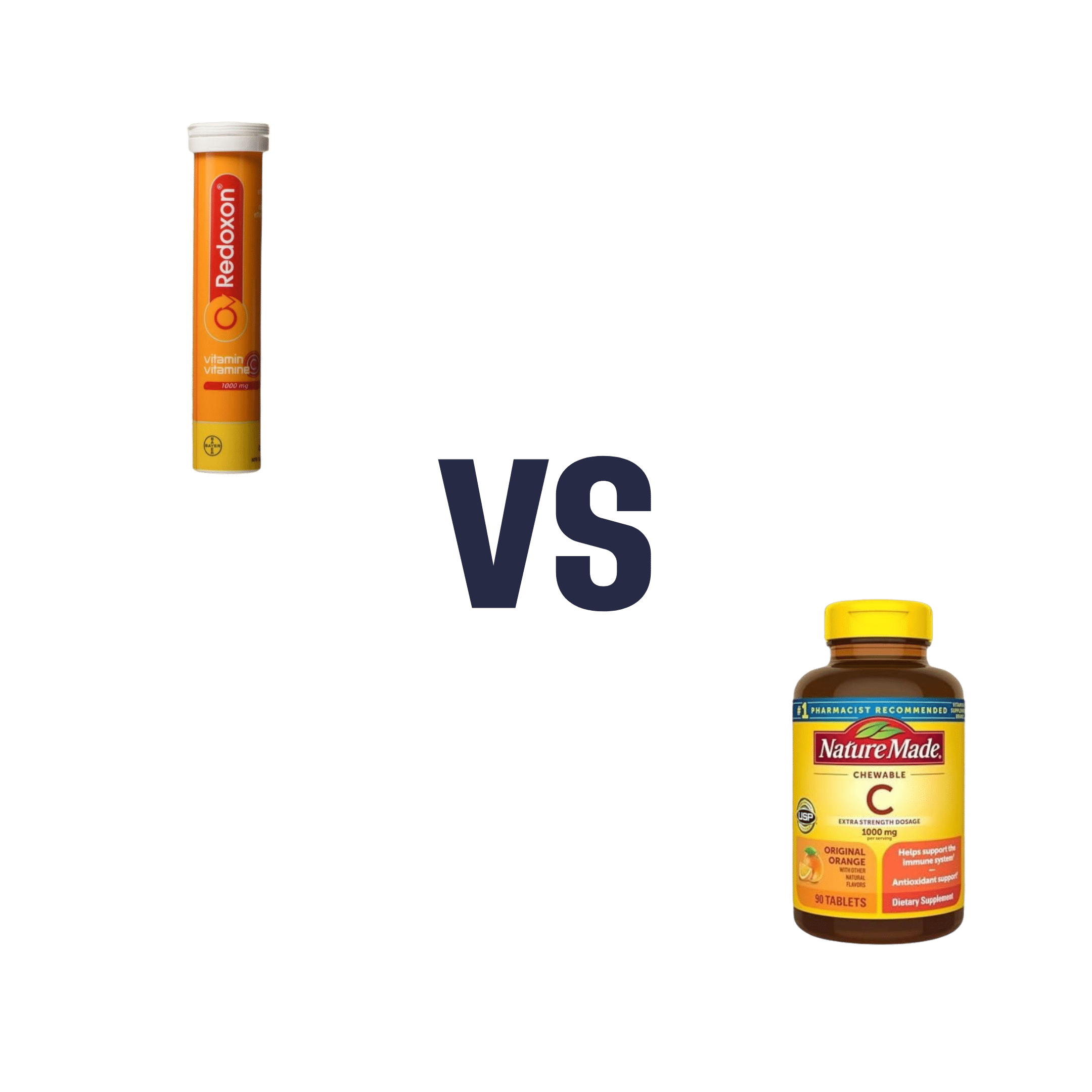
Vitamin C (Drinkable) vs Vitamin C (Chewable) – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing vitamin C (drinkable) to vitamin C (chewable), we picked the drinkable.
Why?
First let’s look at what’s more or less the same in each:
- The usable vitamin C content is comparable
- The bioavailability is comparable
- The additives to hold it together are comparable
So what’s the difference?
With the drinkable, you also drink a glass of water
If you’d like to read more about how to get the most out of the vitamins you take, you can do so here:
Are You Wasting Your Vitamins? Maybe, But You Don’t Have To
If you’d like to get some of the drinkable vitamin C, here’s an example product on Amazon
Enjoy!
Share This Post
-
Tourette’s Syndrome Treatment Options
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Is there anything special that might help someone with Tourette’s syndrome?❞
There are of course a lot of different manifestations of Tourette’s syndrome, and some people’s tics may be far more problematic to themselves and/or others, while some may be quite mild and just something to work around.
It’s an interesting topic for sure, so we’ll perhaps do a main feature (probably also covering the related-and-sometimes-overlapping OCD umbrella rather than making it hyperspecific to Tourette’s), but meanwhile, you might consider some of these options:
Share This Post
-
But First, Inner Peace – by Case Kenny
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Thinking positively and vividly imagining a Ferrari parked in your driveway will not, in fact, cause it to manifest there.
You know what that method does work for, though? Feelings.
This book is essentially a guided thought-and-feeling modelling system that, consisting of 60 chapters to be taken one-per-day, aims to rewire your mind for inner peace.
This is not, however, just a matter of “imagine peacefulness”, or nice-sounding platitudes. Rather, at the end of each chapter there is an exercise and journaling prompts; effectively, work to do along the way.
Weighing in at 438 pages, this is a sizeable book, but part of that is because of the space to write answers to journaling prompts. Still, it’s not exactly a pamphlet, either—there is serious and extensive content here too.
Like any daily reader, you can zip through it all at once if you like, but a benefit to doing the chapter-a-day approach is that it sets a habit of mindful reflection, and gives you a chance to implement each thing, one per day, building up new habits in that regard, too. In contrast, reading it all in one sitting wouldn’t give that.
Bottom line: without inner peace, we don’t have much. Treat yourself—you deserve it.
Click here to check out But First, Inner Peace, and enjoy inner peace!
Share This Post
Related Posts
-
Your Brain on Art – by Susan Magsamen & Ivy Ross
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The notion of art therapy is popularly considered a little wishy-washy. As it turns out, however, there are thousands of studies showing its effectiveness.
Nor is this just a matter of self-expression. As authors Magsamen and Ross explore, different kinds of engagement with art can convey different benefits.
That’s one of the greatest strengths of this book: “this form of engagement with art will give these benefits, according to these studies”
With benefits ranging from reducing stress and anxiety, to overcoming psychological trauma or physical pain, there’s a lot to be said for art!
And because the book covers many kinds of art, if you can’t imagine yourself taking paintbrush to canvas, that’s fine too. We learn of the very specific cognitive benefits of coloring in mandalas (yes, really), of sculpting something terrible in clay, or even just of repainting the kitchen, and more. Each thing has its set of benefits.
The book’s main goal is to encourage the reader to cultivate what the authors call an aesthetic mindset, which involves four key attributes:
- a high level of curiosity
- a love of playful, open-ended exploration
- a keen sensory awareness
- a drive to engage in creative activities
And, that latter? It’s as a maker and/or a beholder. We learn about what we can gain just by engaging with art that someone else made, too.
Bottom line: come for the evidence-based cognitive benefits; stay for the childlike wonder of the universe. If you already love art, or have thought it’s just “not for you”, then this book is for you.
Click here to check out Your Brain On Art, and open up whole new worlds of experience!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Your friend has been diagnosed with cancer. Here are 6 things you can do to support them
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Across the world, one in five people are diagnosed with cancer during their lifetime. By age 85, almost one in two Australians will be diagnosed with cancer.
When it happens to someone you care about, it can be hard to know what to say or how to help them. But providing the right support to a friend can make all the difference as they face the emotional and physical challenges of a new diagnosis and treatment.
Here are six ways to offer meaningful support to a friend who has been diagnosed with cancer.
1. Recognise and respond to emotions
When facing a cancer diagnosis and treatment, it’s normal to experience a range of emotions including fear, anger, grief and sadness. Your friend’s moods may fluctuate. It is also common for feelings to change over time, for example your friend’s anxiety may decrease, but they may feel more depressed.
Spending time together can mean a lot to someone who is feeling isolated during cancer treatment. Chokniti-Studio/Shutterstock Some friends may want to share details while others will prefer privacy. Always ask permission to raise sensitive topics (such as changes in physical appearance or their thoughts regarding fears and anxiety) and don’t make assumptions. It’s OK to tell them you feel awkward, as this acknowledges the challenging situation they are facing.
When they feel comfortable to talk, follow their lead. Your support and willingness to listen without judgement can provide great comfort. You don’t have to have the answers. Simply acknowledging what has been said, providing your full attention and being present for them will be a great help.
2. Understand their diagnosis and treatment
Understanding your friend’s diagnosis and what they’ll go through when being treated may be helpful.
Being informed can reduce your own worry. It may also help you to listen better and reduce the amount of explaining your friend has to do, especially when they’re tired or overwhelmed.
Explore reputable sources such as the Cancer Council website for accurate information, so you can have meaningful conversations. But keep in mind your friend has a trusted medical team to offer personalised and accurate advice.
3. Check in regularly
Cancer treatment can be isolating, so regular check-ins, texts, calls or visits can help your friend feel less alone.
Having a normal conversation and sharing a joke can be very welcome. But everyone copes with cancer differently. Be patient and flexible in your support – some days will be harder for them than others.
Remembering key dates – such as the next round of chemotherapy – can help your friend feel supported. Celebrating milestones, including the end of treatment or anniversary dates, may boost morale and remind your friend of positive moments in their cancer journey.
Always ask if it’s a good time to visit, as your friend’s immune system may be compromised by their cancer or treatments such as chemotherapy or radiotherapy. If you’re feeling unwell, it’s best to postpone visits – but they may still appreciate a call or text.
4. Offer practical support
Sometimes the best way to show your care is through practical support. There may be different ways to offer help, and what your friend needs might change at the beginning, during and after treatment.
For example, you could offer to pick up prescriptions, drive them to appointments so they have transport and company to debrief, or wait with them at appointments.
Meals will always be welcome. However it’s important to remember cancer and its treatments may affect taste, smell and appetite, as well as your friend’s ability to eat enough or absorb nutrients. You may want to check first if there are particular foods they like. Good nutrition can help boost their strength while dealing with the side effects of treatment.
There may also be family responsibilities you can help with, for example, babysitting kids, grocery shopping or taking care of pets.
There may be practical ways you can help, such as dropping off meals. David Trinks/Unsplash 5. Explore supports together
Studies have shown mindfulness practices can be an effective way for people to manage anxiety associated with a cancer diagnosis and its treatment.
If this is something your friend is interested in, it may be enjoyable to explore classes (either online or in-person) together.
You may also be able to help your friend connect with organisations that provide emotional and practical help, such as the Cancer Council’s support line, which offers free, confidential information and support for anyone affected by cancer, including family, friends and carers.
Peer support groups can also reduce your friend’s feelings of isolation and foster shared understanding and empathy with people who’ve gone through a similar experience. GPs can help with referrals to support programs.
6. Stick with them
Be committed. Many people feel isolated after their treatment. This may be because regular appointments have reduced or stopped – which can feel like losing a safety net – or because their relationships with others have changed.
Your friend may also experience emotions such as worry, lack of confidence and uncertainty as they adjust to a new way of living after their treatment has ended. This will be an important time to support your friend.
But don’t forget: looking after yourself is important too. Making sure you eat well, sleep, exercise and have emotional support will help steady you through what may be a challenging time for you, as well as the friend you love.
Our research team is developing new programs and resources to support carers of people who live with cancer. While it can be a challenging experience, it can also be immensely rewarding, and your small acts of kindness can make a big difference.
Stephanie Cowdery, Research Fellow, Carer Hub: A Centre of Excellence in Cancer Carer Research, Translation and Impact, Deakin University; Anna Ugalde, Associate Professor & Victorian Cancer Agency Fellow, Deakin University; Trish Livingston, Distinguished Professor & Director of Special Projects, Faculty of Health, Deakin University, and Victoria White, Professor of Pyscho-Oncology, School of Psychology, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From Lupus To Arthritis: New Developments
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week’s health news round-up highlights some things that are getting better, and some things that are getting worse, and how to be on the right side of both:
New hope for lupus sufferers
Lupus is currently treated mostly with lifelong medications to suppress the immune system, which is not only inconvenient, but also can leave people more open to infectious diseases. The latest development uses CAR T-cell technology (as has been used in cancer treatment for a while) to genetically modify cells to enable the body’s own immune system to behave properly:
Read in full: Exciting new lupus treatment could end need for lifelong medication
Related: How to Prevent (Or Reduce The Severity Of) Inflammatory Diseases
It’s in the hips
There are a lot of different kinds of hip replacements, and those with either delta ceramic or oxidised zirconium head with a highly cross-linked polyethylene liner/cup have the lowest risk of need for revision in the 15 years after surgery. This is important, because obviously, once it’s in there, you want it to be able to stay in there and not have to be touched again any time soon:
Read in full: Study identifies hip implant materials with the lowest risk of needing revision
Related: Nobody Likes Surgery, But Here’s How To Make It Much Less Bad
Sooner is better than later
Often, people won’t know about an unwanted pregnancy in the first six weeks, but for those who are able to catch it early, Very Early Medical Abortion (VEMA) offers a safe an effective way of doing so, with success rate being linked to earliness of intervention:
Read in full: Very early medication abortion is effective and safe, study finds
Related: What Might A Second Trump Presidency Look Like for Health Care?
Increased infectious disease risks from cattle farms
Many serious-to-humans infectious diseases enter the human population via the animal food chain, and in this case, bird flu becoming more rampant amongst cows is starting to pose a clear threat to humans, so this is definitely something to be aware of:
Read in full: Bird flu infects 1 in 14 dairy workers exposed; CDC urges better protections
Related: With Only Gloves To Protect Them, Farmworkers Say They Tend Sick Cows Amid Bird Flu
Herald of woe
Gut health affects most of the rest of health, and there are a lot of links between gut and bone health. In this case, an association has been found between certain changes in the gut microbiome, and subsequent onset of rheumatoid arthritis:
Read in full: Changes in gut microbiome could signal onset of rheumatoid arthritis
Related: Stop Sabotaging Your Gut
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: