Anxiety Attack vs Panic Attack: Do You Know The Difference?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The terms are sometimes used incorrectly, but have quite different meanings. Dr. Julie Smith, psychologist, explains in this short video:
Important distinctions
Anxiety attacks are not clinically recognized terms and lack a clear definition, often used to describe a build-up of anxiety before anticipated stressful events (e.g. social gatherings, medical appointments, etc, though of course what it is will vary from person to person—not everyone finds the same things stressful, or has the same kinds of anticipations around things).
Panic attacks, in contrast, are sudden surges of intense fear or discomfort that peak within minutes. They are characterized by symptoms including at least 4 of:
- palpitations
- sweating
- shortness of breath
- chest pain
- dizziness
- fear of losing control or dying
There’s a misconception that panic attacks never have identifiable triggers while anxiety attacks always do.
In reality, both can occur with or without a clear cause. Panic attacks can arise from various conditions, including trauma, OCD, or phobias, and don’t necessarily mean you have a panic disorder. They can also occur as a drug response, without any known underlying psychological condition.
You may also notice that that list of symptoms has quite a bit of overlap with the symptoms of a heart attack, which a) does not help people to calm down b) can, on the flipside, cause a heart attack to be misdiagnosed as a panic attack.
In terms of management:
- In the moment: breathing exercises, like extending your exhalation (a common example is the “7-11” method, inhaling for 7 seconds and exhaling for 11 seconds), can calm the body and reduce panic symptoms.
- More generally: to prevent panic attacks from becoming more frequent, avoid avoiding safe environments that triggered an attack, like supermarkets or social gatherings. Gradual exposure helps reduce anxiety over time, while avoidance can worsen it.
If panic attacks persist, Dr. Smith advises to seek help from a doctor or psychologist to understand their root causes and develop effective coping strategies.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Should I get a weighted vest to boost my fitness? And how heavy should it be?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Exercise training while wearing a weighted vest is undergoing somewhat of a renaissance. Social media posts and trainers are promoting them as a potential strategy for improving fitness and health.
Exercising with additional weight attached to the body is nothing new. This idea has been used with soldiers for many centuries if not millennia – think long hikes with a heavy pack.
The modern weighted vest comes in a range of designs that are more comfortable and can be adjusted in terms of the weight added. But could one be helpful for you?
ZR10/Shutterstock What the research says
One of the earliest research studies, reported in 1993, followed 36 older people wearing weighted vests during a weekly exercise class and at home over a 20-week period. Wear was associated with improvements in bone health, pain and physical function.
Since then, dozens of papers have evaluated the exercise effects of wearing a weighted vest, reporting a range of benefits.
Not surprisingly, exercise with a weighted vest increases physiological stress – or how hard the body has to work – as shown by increased oxygen uptake, heart rate, carbohydrate utilisation and energy expenditure.
Adding weight equal to 10% of body weight is effective. But it doesn’t appear the body works significantly harder when wearing 5% extra weight compared to body weight alone.
Does more load mean greater injury risk?
A small 2021 study suggested additional weights don’t alter the biomechanics of walking or running. These are important considerations for lower-limb injury risk.
The safety considerations of exercising with weighted vests have also been reported in a biomechanical study of treadmill running with added weight of 1% to 10% of body weight.
While physiological demand (indicated by heart rate) was higher with additional weight and the muscular forces greater, running motion was not negatively affected.
To date no research studies have reported increased injuries due to wearing weighted vests for recreational exercise. However a 2018 clinical study on weight loss in people with obesity found back pain in 25% of those wearing such vests. Whether this can be translated to recreational use in people who don’t have obesity is difficult to say. As always, if pain or discomfort is experienced then you should reduce the weight or stop vest training.
Better for weight loss or bone health?
While wearing a weighted vest increases the energy expenditure of aerobic and resistance exercise, research to show it leads to greater fat loss or retaining muscle mass is somewhat inconclusive.
One older study investigated treadmill walking for 30 minutes, three times a week in postmenopausal women with osteoporosis. The researchers found greater fat loss and muscle gain in the participants who wore a weighted vest (at 4–8% body weight). But subsequent research in obese older adults could not show greater fat loss in participants who wore weighted vests for an average of 6.7 hours per day.
There has been considerable interest in the use of weighted vests to improve bone health in older people. One 2003 study reported significant improvements in bone density in a group of older women over 32 weeks of weighted vest walking and strength training compared to a sedentary control group.
But a 2012 study found no difference in bone metabolism between groups of postmenopausal women with osteoporosis walking on a treadmill with or without a weighted vest.
Making progress
As with any exercise, there is a risk of injury if it is not done correctly. But the risk of weighted vest training appears low and can be managed with appropriate exercise progression and technique.
If you are new to training, then the priority should be to simply start exercising and not complicate it with wearing a weighted vest. The use of body weight alone will be sufficient to get you on the path to considerable gains in fitness.
Once you have a good foundation of strength, aerobic fitness and resilience for muscles, joints and bones, using a weighted vest could provide greater loading intensity as well as variation.
It is important to start with a lighter weight (such as 5% bodyweight) and build to no more than 10% body weight for ground impact exercises such as running, jogging or walking.
For resistance training such as squats, push-ups or chin-ups, progression can be achieved by increasing loads and adjusting the number of repetitions for each set to around 10 to 15. So, heavier loads but fewer repetitions, then building up to increase the load over time.
While weighted vests can be used for resistance training, it is probably easier and more convenient to use barbells, dumbbells, kettle bells or weighted bags.
The benefits of added weight can also be achieved by adding repetition or duration. Geert Pieters/Unsplash The bottom line
Weighted vest training is just one tool in an absolute plethora of equipment, techniques and systems. Yes, walking or jogging with around 10% extra body weight increases energy expenditure and intensity. But training for a little bit longer or at a higher intensity can achieve similar results.
There may be benefits for bone health in wearing a weighted vest during ground-based exercise such as walking or jogging. But similar or greater stimulus to bone growth can be achieved by resistance training or even the introduction of impact training such as hopping, skipping or bounding.
Exercising with a weighted vest likely won’t increase your injury risk. But it must be approached intelligently considering fitness level, existing and previous injuries, and appropriate progression for intensity and repetition.
Rob Newton, Professor of Exercise Medicine, Edith Cowan University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
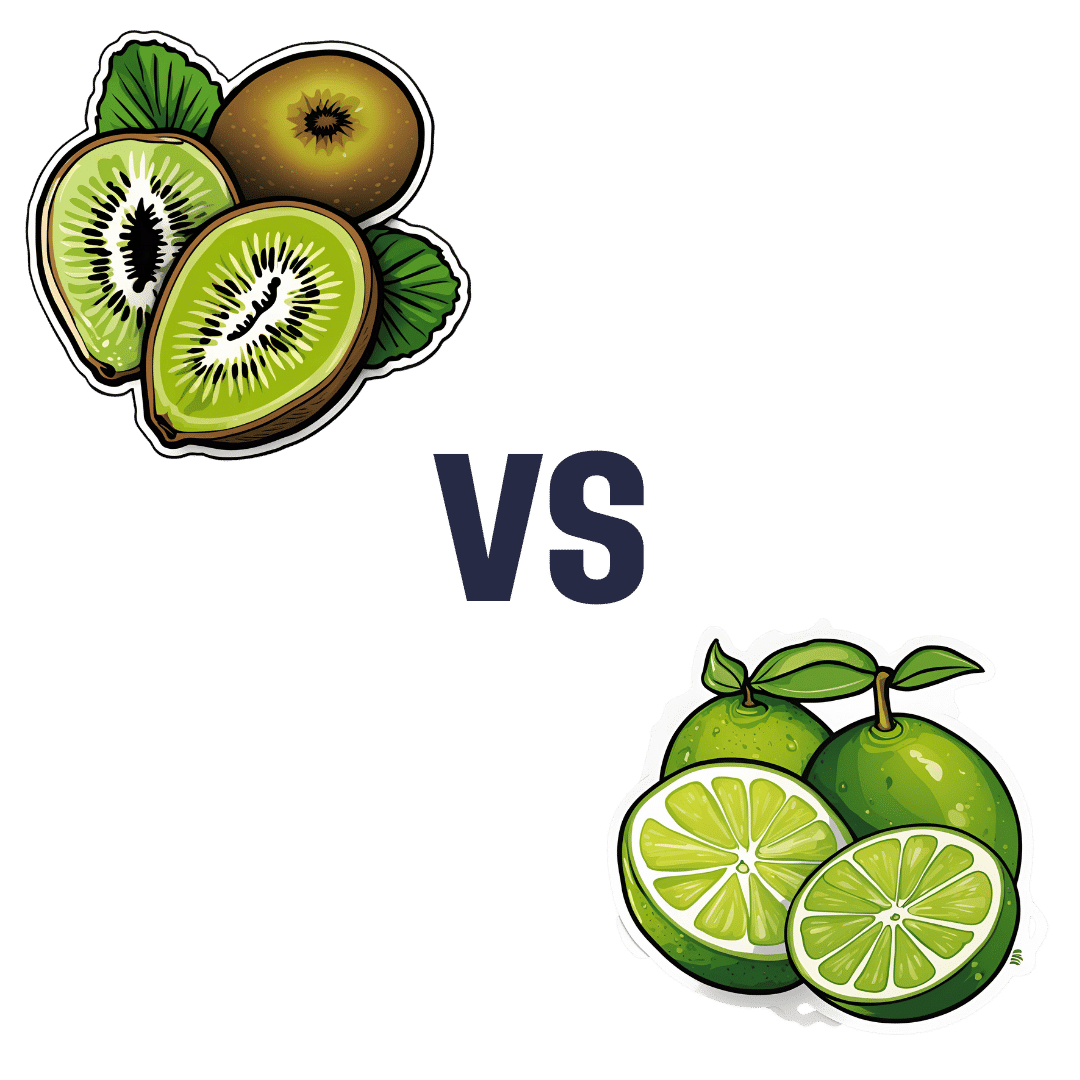
Kiwi vs Lime – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi to lime, we picked the kiwi.
Why?
Looking at the macros first, kiwi has more protein, more carbs, and more fiber. As with most fruits, the fiber is the number we’re most interested in for health purposes; in this case, kiwi is just slightly ahead of lime on all three of those.
In terms of vitamins, kiwi has more of vitamins A, B2, B3, B6, B9, C, E, K, and choline, while lime has a tiny bit more vitamin B5. As in, the vitamin that’s in pretty much anything and is practically impossible to be deficient in unless you are literally starving to death. You may be thinking: aren’t limes a famously good source of vitamin C? And yes, yes they are. But kiwis have >3x more. In other big differences, kiwis also have >6x more vitamin E and >67 times more vitamin K.
When it comes to minerals, kiwi has more calcium, copper, magnesium, manganese, phosphorus, potassium, and zinc, while lime has more iron and selenium. Another easy win for kiwis.
In short: enjoy both; both are good. But kiwis are the more nutritionally dense option by almost every way of measuring it.
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← kiwi is top of the list; it promotes cancer cell death while sparing healthy cells
Take care!
Share This Post
-
Young Mind Young Body – by Sue Ziang
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a very “healthy mind in a healthy body” book, consistent with the author’s status as a holistic health coach. Sometimes that produces a bit of a catch-22 regarding where to start, but for Ziang, the clear answer is to start with the mind, and specifically, one’s perception of one’s own age.
She advocates for building a young mind in a young body, and yes, that’s mind-building much like body-building. This does not mean any kind of wilful self-delusion, but rather, choosing the things that we do get to choose along the way.
The bridge between mind and body, for Ziang, is meditation—which is reasonable, as it’s very much mind-stuff and also very much neurological and has a very real-world impact on the body’s broader health, even simply by such mechanisms as changing breathing, heart rate, neurotransmitter levels, endocrine functions, and the like.
When it comes to the more physical aspects of health, her dietary advice is completely in line with what we write here at 10almonds. Hydrate well, eat more plants, especially beans and greens and whole grains, get good fats in, enjoy spices, practice mindful eating, skip the refined carbohydrates, be mindful of bio-individuality (e.g. one’s own personal dietary quirks that stem from physiology; some of us react differently to this kind of food or that for genetic reasons, and that’s not something to be overlooked).
In the category of exercise, she’s simply about moving more, which while not comprehensive, is not bad advice either.
Bottom line: if you’re looking for an “in” to holistic health and wondering where to start, this book is a fine and very readable option.
Click here to check out “Young Mind Young Body”, and transform yours!
Share This Post
Related Posts
-
What Flexible Dieting Really Means
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Flexibility Is The Dish Of The Day
This is Alan Aragon. Notwithstanding not being a “Dr. Alan Aragon”, he’s a research scientist with dozens of peer-reviewed nutrition science papers to his name, as well as being a personal trainer and fitness educator. Most importantly, he’s an ardent champion of making people’s pursuit of health and fitness more evidence-based.
We’ll be sharing some insights from a book of his that we haven’t reviewed yet, but we will link it at the bottom of today’s article in any case.
What does he want us to know?
First, get out of the 80s and into the 90s
In the world of popular dieting, the 80s were all about calorie-counting and low-fat diets. They did not particularly help.
In the 90s, it was discovered that not only was low-fat not the way to go, but also, regardless of the diet in question, rigid dieting leads to “disinhibition”, that is to say, there comes a point (usually not far into a diet) whereby one breaks the diet, at which point, the floodgates open and the dieter binges unhealthily.
Aragon would like to bring our attention to a number of studies that found this in various ways over the course of the 90s measuring various different metrics including rigid vs flexible dieting’s impacts on BMI, weight gain, weight loss, lean muscle mass changes, binge-eating, anxiety, depression, and so forth), but we only have so much room here, so here’s a 1999 study that’s pretty much the culmination of those:
Flexible vs. Rigid Dieting Strategies: Relationship with Adverse Behavioral Outcomes
So in short: trying to be very puritan about any aspect of dieting will not only not work, it will backfire.
Next, get out of the 90s into the 00s
…which is not only fun if you read “00s” out loud as “naughties”, but also actually appropriate in this case, because it is indeed important to be comfortable being a little bit naughty:
In 2000, Dr. Marika Tiggemann found that dichotomous perceptions of food (e.g. good/bad, clean/dirty, etc) were implicated as a dysfunctional cognitive style, and predicted not only eating disorders and mood disorders, but also adverse physical health outcomes:
Dieting and Cognitive Style: The Role of Current and Past Dieting Behaviour and Cognitions
This was rendered clearer, in terms of physical health outcomes, by Dr. Susan Byrne & Dr. Emma Dove, in 2009:
❝Weight loss was negatively associated with pre-treatment depression and frequency of treatment attendance, but not with dichotomous thinking. Females who regard their weight as unacceptably high and who think dichotomously may experience high levels of depression irrespective of their actual weight, while depression may be proportionate to the degree of obesity among those who do not think dichotomously❞
Aragon’s advice based on all this: while yes, some foods are better than others, it’s more useful to see foods as being part of a spectrum, rather than being absolutist or “black and white” about it.
Next: hit those perfect 10s… Imperfectly
The next decade expanded on this research, as science is wont to do, and for this one, Aragon shines a spotlight on Dr. Alice Berg’s 2018 study with obese women averaging 69 years of age, in which…
In other words (and in fact, to borrow Dr. Berg’s words from that paper),
❝encouraging a flexible approach to eating behavior and discouraging rigid adherence to a diet may lead to better intentional weight loss for overweight and obese older women❞
You may be wondering: what did this add to the studies from the 90s?
And the key here is: rather than being observational, this was interventional. In other words, rather than simply observing what happened to people who thought one way or another, this study took people who had a rigid, dichotomous approach to food, and gave them a 6-month behavioral intervention (in other words, support encouraging them to be more flexible and open in their approach to food), and found that this indeed improved matters for them.
Which means, it’s not a matter of fate or predisposition, as it could have been back in the 90s, per “some people are just like that; who’s to say which factor causes which”. Instead, now we know that this is an approach that can be adopted, and it can be expected to work.
Beyond weight loss
Now, so far we’ve talked mostly about weight loss, and only touched on other health outcomes. This is because:
- weight loss a very common goal for many
- it’s easy to measure so there’s a lot of science for it
Incidentally, if it’s a goal of yours, here’s what 10almonds had to say about that, along with two follow-up articles for other related goals:
Spoiler: we agree with Aragon, and recommend a relaxed and flexible approach to all three of these things
Aragon’s evidence-based approach to nutrition has found that this holds true for other aspects of healthy eating, too. For example…
To count or not to count?
It’s hard to do evidence-based anything without counting, and so Aragon talks a lot about this. Indeed, he does a lot of counting in scientific papers of his own, such as:
and
The effect of protein timing on muscle strength and hypertrophy: a meta-analysis
…as well as non-protein-related but diet-related topics such as:
But! For the at-home health enthusiast, Aragon recommends that the answer to the question “to count or not to count?” is “both”:
- Start off by indeed counting and tracking everything that is important to you (per whatever your current personal health intervention is, so it might be about calories, or grams of protein, or grams of carbs, or a certain fat balance, or something else entirely)
- Switch to a more relaxed counting approach once you get used to the above. By now you probably know the macros for a lot of your common meals, snacks, etc, and can tally them in your head without worrying about weighing portions and knowing the exact figures.
- Alternatively, count moderately standardized portions of relevant foods, such as “three servings of beans or legumes per day” or “no more than one portion of refined carbohydrates per day”
- Eventually, let habit take the wheel. Assuming you have established good dietary habits, this will now do you just fine.
This latter is the point whereby the advice (that Aragon also champions) of “allow yourself an unhealthy indulgence of 10–20% of your daily food”, as a budget of “discretionary calories”, eventually becomes redundant—because chances are, you’re no longer craving that donut, and at a certain point, eating foods far outside the range of healthiness you usually eat is not even something that you would feel inclined to do if offered.
But until that kicks in, allow yourself that budget of whatever unhealthy thing you enjoy, and (this next part is important…) do enjoy it.
Because it is no good whatsoever eating that cream-filled chocolate croissant and then feeling guilty about it; that’s the dichotomous thinking we had back in the 80s. Decide in advance you’re going to eat and enjoy it, then eat and enjoy it, then look back on it with a sense of “that was enjoyable” and move on.
The flipside of this is that the importance of allowing oneself a “little treat” is that doing so actively helps ensure that the “little treat” remains “little”. Without giving oneself permission, then suddenly, “well, since I broke my diet, I might as well throw the whole thing out the window and try again on Monday”.
On enjoying food fully, by the way:
Mindful Eating: How To Get More Nutrition Out Of The Same Food
Want to know more from Alan Aragon?
Today we’ve been working heavily from this book of his; we haven’t reviewed it yet, but we do recommend checking it out:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Vary Breakfast for Digestion?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Would appreciate your thoughts on how best to promote good digestion. For years, my breakfast has consisted of flaxseeds, sunflower seeds, and almonds – all well ground up – eaten with a generous amount of kefir. This works a treat as far as my digestion is concerned. But I sometimes wonder whether it would be better for my health if I varied or supplemented this breakfast. How might I do this without jeopardising my good digestion?❞
Sounds like you’re already doing great! Those ingredients are all very nutrient-dense, and grinding them up improves digestion greatly, to the point that you’re getting nutrients your body couldn’t get at otherwise. And the kefir, of course, is a top-tier probiotic.
Also, you’re getting plenty of protein and healthy fats in with your carbs, which results in the smoothest blood sugar curve.
As for variety…
Variety is good in diet, but variety within a theme. Our gut microbiota change according to what we eat, so sudden changes in diet are often met with heavy resistance from our gut.
- For example, people who take up a 100% plant-based diet overnight often spend the next day in the bathroom, and wonder what happened.
- Conversely, a long-time vegan who (whether by accident or design) consumes meat or dairy will likely find themself quickly feeling very unwell, because their gut microbiota have no idea what to do with this.
So, variety yes, but within a theme, and make any changes gradual for the easiest transition.
All in all, the only obvious suggestion for improvement is to consider adding some berries. These can be fresh, dried, or frozen, and will confer many health benefits (most notably a lot of antioxidant activity).
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Health Tips for Males Too
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Articles are very informative and helpful. Maybe it’s me but things seem to lean more toward females. That being said don’t forget us males❞
Rest assured, we could never forget you! We try to make as much as possible of our content applicable to as many as possible of our readers, but of course not everything can be relevant for everyone.
This is, presumably, in response to our recent feature on menopausal health, because previous to that, our next-most-recent main feature that centred women’s health was a month ago—that was about breast cancer, and did have a section on breast cancer in men too. You might also enjoy the book we reviewed recently about prostate health, or our regular sponsor offering testosterone therapy. Please feel free to check out our articles on saw palmetto against male pattern baldness and BPH, as well as mental health issues that disproportionally affect men.
And of course, if you have specific questions/requests about men’s health (or any other health topic) we’re only ever an email away (or use the handy feedback widget, as you did to make this request)!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: