An RSV vaccine has been approved for people over 60. But what about young children?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Therapeutic Goods Administration (TGA) has approved a vaccine against respiratory syncytial virus (RSV) in Australia for the first time. The shot, called Arexvy and manufactured by GSK, will be available by prescription to adults over 60.
RSV is a contagious respiratory virus which causes an illness similar to influenza, most notably in babies and older adults.
So while it will be good to have an RSV vaccine available for older people, where is protection up to for the youngest children?
A bit about RSV
RSV was discovered in chimpanzees with respiratory illness in 1956, and was soon found to be a common cause of illness in humans.
There are two key groups of people we would like to protect from RSV: babies (up to about one year old) and people older than 60.
Babies tend to fill up hospitals during the RSV season in late spring and winter in large numbers, but severe infection requiring admission to intensive care is less common.
In babies and younger children, RSV generally causes a wheezing asthma-like illness (bronchiolitis), but can also cause pneumonia and croup.
Although there are far fewer hospital admissions among older people, they can develop severe disease and die from an infection.

Prostock-studio/Shutterstock
RSV vaccines for older people
For older adults, there are actually several RSV vaccines in the pipeline. The recent Australian TGA approval of Arexvy is likely to be the first of several, with other vaccines from Pfizer and Moderna currently in development.
The GSK and Pfizer RSV vaccines are similar. They both contain a small component of the virus, called the pre-fusion protein, that the immune system can recognise.
Both vaccines have been shown to reduce illness from RSV by more than 80% in the first season after vaccination.
In older adults, side effects following Arexvy appear to be similar to other vaccines, with a sore arm and generalised aches and fatigue frequently reported.
Unlike influenza vaccines which are given each year, it is anticipated the RSV vaccine would be a one-off dose, at least at this stage.
Protecting young children from RSV
Younger babies don’t tend to respond well to some vaccines due to their immature immune system. To prevent other diseases, this can be overcome by giving multiple vaccine doses over time. But the highest risk group for RSV are those in the first few months of life.
To protect this youngest age group from the virus, there are two potential strategies available instead of vaccinating the child directly.
The first is to give a vaccine to the mother and rely on the protective antibodies passing to the infant through the placenta. This is similar to how we protect babies by vaccinating pregnant women against influenza and pertussis (whooping cough).
The second is to give antibodies directly to the baby as an injection. With both these strategies, the protection provided is only temporary as antibodies wane over time, but this is sufficient to protect infants through their highest risk period.

Image Point Fr/Shutterstock
Abrysvo, the Pfizer RSV vaccine, has been trialled in pregnant women. In clinical trials, this vaccine has been shown to reduce illness in infants for up to six months. It has been approved in pregnant women in the United States, but is not yet approved in Australia.
An antibody product called palivizumab has been available for many years, but is only partially effective and extremely expensive, so has only been given to a small number of children at very high risk.
A newer antibody product, nirsevimab, has been shown to be effective in reducing infections and hospitalisations in infants. It was approved by the TGA in November, but it isn’t yet clear how this would be accessed in Australia.
What now?
RSV, like influenza, is a major cause of respiratory illness, and the development of effective vaccines represents a major advance.
While the approval of the first vaccine for older people is an important step, many details are yet to be made available, including the cost and the timing of availability. GSK has indicated its vaccine should be available soon. While the vaccine will initially only be available on private prescription (with the costs paid by the consumer), GSK has applied for it to be made free under the National Immunisation Program.
In the near future, we expect to hear further news about the other vaccines and antibodies to protect those at higher risk from RSV disease, including young children.
Allen Cheng, Professor of Infectious Diseases, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Science Of Sounds
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We Think You Might Like The Sound Of This…
We’ve written before about the benefits of mindfulness meditation, and how to do it.
We also reviewed a great book on a related topic:
This is Your Brain On Music – by Dr. Daniel Levitin
(yes, that’s the same neuroscientist that we featured as an expert talking about The Five Keys of Aging Healthily)
But what happens when we combine the two?
Mantra meditation & music
Most scientific studies that have been undertaken with regard to meditation tend to focus on mindfulness meditation. It’s easy, effective, and (which makes a difference when it comes to publication bias) is a very safe bet when it comes to funding.
However, today we’re going to look at mantra meditation, which has a lot in common, neurologically speaking, with music. Indeed, when the two were compared separately in a randomized control trial:
❝Daily mantra meditation or classical music listening may be beneficial for cognitive outcomes and quality of life of breast cancer survivors with cancer-related cognitive impairment.
The cognitive benefits appear to be sustained beyond the initial intervention period.❞
One possible reason for some of the similar benefits is the vagus nerve—whether intoning a mantra, or humming along to music, the vibrations can stimulate the vagus nerve, which in turn activates the parasympathetic nervous system, resulting in body-wide relaxation:
The Vagus Nerve (And How You Can Make Use Of It)
How effective is mantra meditation?
According to a large recent narrative review, it depends on your goal:
❝Based on the studies in the four important areas presented, there is no doubt of a strong connection between mantra meditation and human health.
Strong evidence has been found that practicing mantra meditation is effective in relieving stress and in coping with hypertension.
For the other two areas: anxiety and immunity, the evidence is inconclusive or not strong enough to firmly support the claim that the mantra meditation can be used to reduce anxiety or to improve immunity. ❞
Read in full: Scientific Evidence of Health Benefits by Practicing Mantra Meditation: Narrative Review
this is a very interesting read if you do have the time!
How do I practice mantra meditation?
The definition is broad, but the critical criteria are:
- You meditate…
- …using a mantra
Lest that seem flippant: those really are the two key points!
Meditation comes in various forms, and mantra meditation is a form of focussed meditation. While some focussed meditation forms may use a candle or some other focal point, in mantra meditation, the mantra itself provides the focus.
You may be wondering: what should the mantra be?
Classic and well-tested mantras include such simple things as the monosyllabic Sanskrit “Om” or “Ham”. We’re a health science newsletter, so we’ll leave esoteric meanings to other publications as they are beyond our scope, but we will say that these result, most naturally, in the humming sound that we mentioned earlier stimulates the vagus nerve.
But that’s not the only way. Practitioners of religions that have repetitive prayer systems (e.g. anything that uses prayer beads, for example) also provide the basis of focused meditation, using a mantra (in this case, usually a very short oft-repeated prayer phrase).
How long is needed for benefits?
Most studies into mantra meditation have used timed sessions of 15–30 minutes, with 20 minutes being a commonly-used session length, once per day. However…
- Vagus nerve benefits should appear a lot more quickly than that (under 5 minutes) in the case of mantras that cause that vibration we mentioned.
- Repetitive spoken prayers (or similar repeated short phrases, for the irreligious) will generally effect relaxation in whatever period of time it takes for your brain to be fully focused on what you are doing now, instead of what you were thinking about before. If using counting beads, then you probably already know what number works for you.
(again, as a health science publication, we cannot comment on any otherworldly benefits, but the worldly benefits seem reason enough to consider these practices for their potential therapeutic effects)
10almonds tip: for any meditative practice that you want to take approximately a given period of time, we recommend investing in a nice sand timer like this one, as this will not result in a jarring alarm going off!
Like to jazz things up a little?
Enjoy: Meditation That You’ll Actually Enjoy ← Meditation games!
Prefer to keep things to the basics?
Enjoy: No Frills, Evidence-Based Mindfulness ← The simplest scientific approach
Take care!
Share This Post
-
Ayurveda’s Contributions To Science
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ayurveda’s Contributions To Science (Without Being Itself Rooted in Scientific Method)
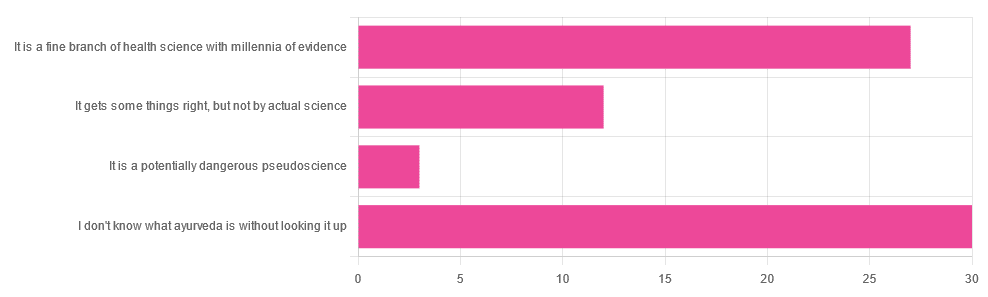
Yesterday, we asked you for your opinions on ayurveda, and got the above-depicted, below-described, set of responses. Of those who responded…
- A little over 41% said “I don’t know what ayurveda is without looking it up”
- A little over 37% said “It is a fine branch of health science with millennia of evidence”
- A little over 16% said “It gets some things right, but not by actual science”
- A little over 4% said “It is a potentially dangerous pseudoscience”
So, what does the science say?
Ayurveda is scientific: True or False?
False, simply. Let’s just rip the band-aid off in this case. That doesn’t mean it’s necessarily without merit, though!
Let’s put it this way:
- If you drink coffee to feel more awake because scientific method has discerned that caffeine has vasoconstrictive and adenosine-blocking effects while also promoting dopaminergic activity, then your consumption of coffee is evidence-based and scientific. Great!
- If you drink coffee to feel more awake because somebody told you that that somebody told them that it energizes you by balancing the elements fire (the heat of the coffee), air (the little bubbles on top), earth (the coffee grinds), water (the water), and ether (steam), then that is neither evidence-based nor scientific, but it will still work exactly the same.
Ayurveda is a little like that. It’s an ancient traditional Indian medicine, based on a combination of anecdotal evidence and supposition.
- The anecdotal evidence from ayurveda has often resulted in herbal remedies that, in modern scientific trials, have been found to have merit.
- Ayurvedic meditative practices also have a large overlap with modern mindfulness practices, and have also been found to have merit
- Ayurveda also promotes the practice of yoga, which is indeed a very healthful activity
- The supposition from ayurveda is based largely in those five elements we mentioned above, as well as a “balancing of humors” comparable to medieval European medicine, and from a scientific perspective, is simply a hypothesis with no evidence to support it.
Note: while ayurveda is commonly described as a science by its practitioners in the modern age, it did not originally claim to be scientific, but rather, wisdom handed down directly by the god Dhanvantari.
Ayurveda gets some things right: True or False?
True! Indeed, we covered some before in 10almonds; you may remember:
Bacopa Monnieri: A Well-Evidenced Cognitive Enhancer
(Bacopa monnieri is also known by its name in ayurveda, brahmi)
There are many other herbs that have made their way from ayurveda into modern science, but the above is a stand-out example. Others include:
- Ashwagandha: The Root of All Even-Mindedness?
- Boswellia serrata (Frankincense) Against Pain and Depression/Anxiety
Yoga and meditation are also great, and not only that, but great by science, for example:
- NCCIH | Yoga for Health: Clinical Guidelines, Scientific Literature, Info for Patients
- The Neuroscience of Mindfulness: How Mindfulness Alters the Brain and Facilitates Emotion Regulation
Ayurveda is a potentially dangerous pseudoscience: True or False?
Also True! We covered why it’s a pseudoscience above, but that doesn’t make it potentially dangerous, per se (you’ll remember our coffee example).
What does, however, make it potentially dangerous (dose-dependent) is its use of heavy metals such as lead, mercury, and arsenic:
Heavy Metal Content of Ayurvedic Herbal Medicine Products
Some final thoughts…
Want to learn more about the sometimes beneficial, sometimes uneasy relationship between ayurveda and modern science?
A lot of scholarly articles trying to bridge (or further separate) the two were very biased one way or the other.
Instead, here’s one that’s reasonably optimistic with regard to ayurveda’s potential for good, while being realistic about how it currently stands:
Development of Ayurveda—Tradition to trend
Take care!
Share This Post
-
F*ck You Chaos – by Dominika Choroszko
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all read decluttering books. Some may even have decluttering books cluttering bookshelves. This one’s a little different, though:
Dominika Choroszko looks at assessing, decluttering, and subsequently organizing:
- Your home
- Your mind
- Your finances
In other words
- she starts off like Marie Kondo, and…
- phases through doing the jobs of Queer Eye’s “Fab Five”, before…
- sitting us down with some CBT worksheets, and…
- finally going through finances à la Martin Lewis.
By the time we’ve read the book, it’s as though Mary Poppins has breezed through our house, head, and bank account, leaving everything “practically perfect in every way”.
Of course, it’s on us to actually do the work, but as many of us struggle with “how” and the ever-dreaded “but where to begin”, Choroszko’s whirlwind impetus and precision guidance (many very direct practical steps to take) really grease the wheels of progress.
In short, this could be the book that kickstarts your next big “getting everything into better order” drive, with a clear step-by-step this-then-this-then-this linear process.
Share This Post
Related Posts
-
The Daily Stoic – by Ryan Holiday & Stephen Hanselman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s this, a philosophy book in a health and productivity newsletter? Well, look at it this way: Aristotle basically wrote the “How To Win Friends And Influence People” of his day, and Plato before him wrote a book about management.
In this (chiefly modern!) book, we see what the later Stoic philosophers had to say about getting the most out of life—which is also what we’re about, here at 10almonds!
We tend to use the word “stoic” in modern English to refer to a person who is resolute in the face of hardship. The traditional meaning does encompass that, but also means a lot more: a whole, rounded, philosophy of life.
Philosophy in general is not an easy thing into which to “dip one’s toe”. No matter where we try to start, it seems, it turns out there were a thousand other things we needed to read first!
This book really gets around that. The format is:
- There’s a theme for each month
- Each month has one lesson per day
- Each daily lesson starts with some words from a renowned stoic philosopher, and then provides commentary on such
- The commentary provides a jumping-off point and serves as a prompt to actually, genuinely, reflect and apply the ideas.
Unlike a lot of “a year of…” day-by-day books, this is not light reading, by the way, and you are getting a weighty tome for your money.
But, the page-length daily lessons are indeed digestible—which, again, is what we like at 10almonds!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Lower Your Blood Pressure (Cardiologists Explain)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today we enjoy the benefit of input from Dr. Zalzal, Dr. Weeing, and Dr. Hefferman!
If the thought of being in an operating room with three cardiologists in scrubs doesn’t raise your blood pressure too much, the doctors in question have a lot to offer for bringing those numbers down and keeping them down! They recommend…
150 mins of Exercise
This isn’t exactly controversial, but: move your body!
See also: Exercise Less; Move More
Reduce salt
Most people eating the Standard American Diet (SAD) are getting far too much—mostly because it’s in so many processed foods already.
See also: How Too Much Salt May Lead To Organ Failure
Eating habits
There’s a lot more to eating healthily for the heart than just reducing salt, and over all, the Mediterranean diet comes out scoring highest:
- What Is The Mediterranean Diet Anyway? ← a primer for the uncertain
- Four Ways To Upgrade The Mediterranean ← includes a heart-specialized version!
Reduce alcohol
According to the WHO, the only healthy amount of alcohol is zero. According to these cardiologists: at the very least cut down. However much or little you’re drinking right now, less is better.
See also: How To Reduce Or Quit Alcohol
Maintain healthy weight
While the doctors agree that BMI isn’t a great method of measuring metabolic health, it is clear that carrying excessive weight isn’t good for the heart.
See also: Lose Weight (Healthily!)
No smoking
This one’s pretty straight forward: just don’t.
See also: Addiction Myths That Are Hard To Quit
Reduce stress
Chronic stress has a big impact on chronic health in general and that includes its effect on blood pressure. So, improving one improves the other.
See also: Lower Your Cortisol! (Here’s Why & How)
Good sleep
Quality matters as much as quantity, and that goes for its effect on your blood pressure too, so take the time to invest in your good health!
See also: The 6 Dimensions Of Sleep (And Why They Matter)
Click Here If The Embedded Video Doesn’t Load Automatically!
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Intuitive Eating – by Evelyn Tribole and Elyse Resch
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be given to wonder: if this is about intuitive eating, and an anti-diet approach, why a whole book?
There’s a clue in the other part of the title: “4th Edition”.
The reason there’s a 4th edition (and before it, a 3rd and 2nd edition) is because this book is very much full of science, and science begets more science, and the evidence just keeps on rolling in.
While neither author is a doctor, each has a sizeable portion of the alphabet after their name (more than a lot of doctors), and this is an incredibly well-evidenced book.
The basic premise from many studies is that restrictive dieting does not work well long-term for most people, and instead, better is to make use of our bodies’ own interoceptive feedback.
You see, intuitive eating is not “eat randomly”. We do not call a person “intuitive” because they speak or act randomly, do we? Same with diet.
Instead, the authors give us ten guiding principles (yes, still following the science) to allow us a consistent “finger on the pulse” of what our body has to say about what we have been eating, and what we should be eating.
Bottom line: if you want to be a lot more in tune with your body and thus better able to nourish it the way it needs, this book is literally on the syllabus for many nutritional science classes, and will stand you in very good stead!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: