Alzheimer’s Risk Reduction Methods
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Q: I am now in the “aging” population. A great concern for me is Alzheimers. My father had it and I am so worried. What is the latest research on prevention?
Very important stuff! We wrote about this not long back:
- See: How To Reduce Your Alzheimer’s Risk
- See also: Brain Food? The Eyes Have It!
(one good thing to note is that while Alzheimer’s has a genetic component, it doesn’t appear to be hereditary per se. Still, good to be on top of these things, and it’s never too early to start with preventive measures!)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Are You?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Answering The Most Difficult Question: How Are You?
Today’s feature is aimed at helping mainly two kinds of people:
- “I have so many emotions that I don’t always know what to do with them”
- “What is an emotion, really? I think I felt one some time ago”
So, if either those describe you and/or a loved one, read on…
Alexithymia
Alexi who? Alexithymia is an umbrella term for various kinds of problems with feeling emotions.
That could be “problems feeling emotions” as in “I am unable to feel emotions” or “problems feeling emotions” as in “feeling these emotions is a problem for me”.
It is most commonly used to refer to “having difficulty identifying and expressing emotions”.
There are a lot of very poor quality pop-science articles out there about it, but here’s a decent one with good examples and minimal sensationalist pathologization:
Alexithymia Might Be the Reason It’s Hard to Label Your Emotions
A somatic start
Because a good level of self-awareness is critical for healthy emotional regulation, let’s start there. We’ll write this in the first person, but you can use it to help a loved one too, just switching to second person:
Simplest level first:
Are my most basic needs met right now? Is this room a good temperature? Am I comfortable dressed the way I am? Am I in good physical health? Am I well-rested? Have I been fed and watered recently? Does my body feel clean? Have I taken any meds I should be taking?
Note: If the answer is “no”, then maybe there’s something you can do to fix that first. If the answer is “no” and also you can’t fix the thing for some reason, then that’s unfortunate, but just recognize it anyway for now. It doesn’t mean the thing in question is necessarily responsible for how you feel, but it’s good to check off this list as a matter of good practice.
Bonus question: it’s cliché, but if applicable… What time of the month is it? Because while hormonal mood swings won’t create moods out of nothing, they sure aren’t irrelevant either and should be listened to too.
Bodyscanning next
What do you feel in each part of your body? Are you clenching your jaw? Are your shoulders tense? Do you have a knot in your stomach? What are your hands doing? How’s your posture? What’s your breathing like? How about your heart? What are your eyes doing?
Your observations at this point should be neutral, by the way. Not “my posture is terrible”, but “my posture is stooped”, etc. Much like in mindfulness meditation, this is a time for observing, not for judging.
Narrowing it down
Now, like a good scientist, you have assembled data. But what does the data mean for your emotions? You may have to conduct some experiments to find out.
Thought experiments: what calls to you? What do you feel like doing? Do you feel like curling up in a ball? Breaking something? Taking a bath? Crying?
Maybe what calls to you, or what you feel like doing, isn’t something that’s possible for you to do. This is often the case with anxiety, for example, and perhaps also guilt. But whatever calls to you, notice it, reflect on it, and if it’s something that your conscious mind considers reasonable and safe for you to do, you can even try doing it.
Your body is trying to help you here, by the way! It will try (and usually succeed) to give you a little dopamine spike when you anticipate doing the thing it wants you to do. Warning: it won’t always be right about what’s best for you, so do still make your own decisions about whether it is a good idea to safely do it.
Practical experiments: whether you have a theory or just a hypothesis (if you have neither make up a hypothesis; that is also what scientists do), you can also test it:
If in the previous step you identified something you’d like to do and are able to safely do it, now is the time to try it. If not…
- Find something that is likely to (safely) tip you into emotional expression, ideally, in a cathartic way. But, whatever you can get is good.
- Music is great for this. What songs (or even non-lyrical musical works) make you sad, happy, angry, energized? Try them.
- Literature and film can be good too, albeit they take more time. Grab that tear-jerker or angsty rage-fest, and see if it feels right.
- Other media, again, can be completely unrelated to the situation at hand, but if it evokes the same emotion, it’ll help you figure out “yes, this is it”.
- It could be a love letter or a tax letter, it could be an outrage-provoking news piece or some nostalgic thing you own.
Ride it out, wherever it takes you (safely)
Feelings feel better felt. It doesn’t always seem that way! But, really, they are.
Emotions, just like physical sensations, are messengers. And when a feeling/sensation is troublesome, one of the best ways to get past it is to first fully listen to it and respond accordingly.
- If your body tells you something, then it’s good to acknowledge that and give it some reassurance by taking some action to appease it.
- If your emotions are telling you something, then it’s good to acknowledge that and similarly take some action to appease it.
There is a reason people feel better after “having a good cry”, or “pounding it out” against a punchbag. Even stress can be dealt with by physically deliberately tensing up and then relaxing that tension, so the body thinks that you had a fight and won and can relax now.
And when someone is in a certain (not happy) mood and takes (sometimes baffling!) actions to stay in that mood rather than “snap out of it”, it’s probably because there’s more feeling to be done before the body feels heard. Hence the “ride it out if you safely can” idea.
How much feeling is too much?
While this is in large part a subjective matter, clinically speaking the key question is generally: is it adversely affecting daily life to the point of being a problem?
For example, if you have to spend half an hour every day actively managing a certain emotion, that’s probably indicative of something unusual, but “unusual” is not inherently pathological. If you’re managing it safely and in a way that doesn’t negatively affect the rest of your life, then that is generally considered fine, unless you feel otherwise about it.
If you do think “I would like to not think/feel this anymore”, then there are tools at your disposal too:
- How To Manage Chronic Stress
- How To Set Anxiety Aside
- How To Stop Revisiting Those Memories
- How To Stay Alive (When You Really Don’t Want To)
Take care!
Share This Post
-
Chipotle Chili Wild Rice
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a very gut-healthy recipe that’s also tasty and filling, and packed with polyphenols too. What’s not to love?
You will need
- 1 cup cooked wild rice (we suggest cooking it with 1 tbsp chia seeds added)
- 7 oz cooked sweetcorn (can be from a tin or from frozen or cook it yourself)
- 4 oz charred jarred red peppers (these actually benefit from being from a jar—you can use fresh or frozen if necessary, but only jarred will give you the extra gut-healthy benefits from fermentation)
- 1 avocado, pitted, peeled, and cut into small chunks
- ½ red onion, thinly sliced
- 6–8 sun-dried tomatoes, chopped
- 2 tbsp extra virgin olive oil
- 2 tsp chipotle chili paste (adjust per your heat preferences)
- 1 tsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
- Juice of 1 lime
Method
(we suggest you read everything at least once before doing anything)
1) Mix the cooked rice, red onion, sweetcorn, red peppers, avocado pieces, and sun-dried tomato, in a bowl. We recommend to do it gently, or you will end up with guacamole in there.
2) Mix the olive oil, lime juice, chipotle chili paste, black pepper, and MSG/salt, in another bowl. If perchance you have a conveniently small whisk, now is the time to use it. Failing that, a fork will suffice.
3) Add the contents of the second bowl to the first, tossing gently but thoroughly to combine well, and serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Brown Rice vs Wild Rice – Which is Healthier?
- Making Friends With Your Gut (You Can Thank Us Later)
- Capsaicin For Weight Loss And Against Inflammation
Take care!
Share This Post
-
What Do The Different Kinds Of Fiber Do? 30 Foods That Rank Highest
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve talked before about how important fiber is:
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
And even how it’s arguably the most important dietary factor when it comes to avoiding heart disease:
What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure ← Spoiler: it’s fiber
And yes, that’s even when considered alongside other (also laudable) dietary interventions such as lowering intake of sodium, various kinds of saturated fat, and red meat.
So, what should we know about fiber, aside from “aim to get nearer 40g/day instead of the US average 16g/day”?
Soluble vs Insoluble
The first main way that dietary fibers can be categorized is soluble vs insoluble. Part of the difference is obvious, but bear with us, because there’s more to know about each:
- Soluble fiber dissolves (what a surprise) in water and, which part is important, forms a gel. This slows down things going through your intestines, which is important for proper digestion and absorption of nutrients (as well as avoiding diarrhea). Yes, you heard right: getting enough of the right kind of fiber helps you avoid diarrhea.
- Insoluble fiber does not dissolve (how shocking) in water and thus mostly passes through undigested by us (some will actually be digested by gut microbes who subsist on this, and in return for us feeding them daily, they make useful chemicals for us). This kind of fiber is also critical for healthy bowel movements, because without it, constipation can ensue.
Both kinds of fiber improve just about every metric related to blood, including improving triglycerides and improving insulin sensitivity and blood glucose levels. Thus, they help guard against various kinds of cardiovascular disease, diabetes, and metabolic disease in general. Do note that because whatever’s good for your heart/blood is good for your brain (which requires a healthy heart and bloodstream to nourish it and take away waste), likely this also has a knock-on effect against cognitive decline, but we don’t have hard science for that claim so we’re going to leave that last item as a “likely”.
However, one thing’s for sure: if you want a healthy gut, heart, and brain, you need a good balance of soluble and insoluble fibers.
10 of the best for soluble fiber
Food Soluble Fiber Type(s) Soluble Fiber (g per serving) Insoluble Fiber Type(s) Insoluble Fiber (g per serving) Total Fiber (g per serving) Kidney beans (1 cup cooked) Pectin, Resistant Starch 1.5–2 Hemicellulose, Cellulose 6 8 Lentils (1 cup cooked) Pectin, Resistant Starch 1.5–2 Cellulose 6 7.5 Barley (1 cup cooked) Beta-glucan 3–4 Hemicellulose 2 6 Brussels sprouts (1 cup cooked) Pectin 1–1.5 Cellulose, Hemicellulose 2 3.5 Oats (1 cup cooked) Beta-glucan 2–3 Cellulose 1 3 Apples (1 medium) Pectin 1–2 Cellulose, Hemicellulose 2 3 Carrots (1 cup raw) Pectin 1–1.5 Cellulose, Hemicellulose 2 3 Citrus fruits (orange, 1 medium) Pectin 1–1.5 Cellulose 1 2.5 Flaxseeds (2 tbsp) Mucilage, Lignin 1–1.5 Cellulose 1 2.5 Psyllium husk (1 tbsp) Mucilage 3–4 Trace amounts 0 3–4 10 of the best for insoluble fiber
Food Soluble Fiber Type(s) Soluble Fiber (g per serving) Insoluble Fiber Type(s) Insoluble Fiber (g per serving) Total Fiber (g per serving) Wheat bran (1 cup) Trace amounts 0 Cellulose, Lignin 6–8 6–8 Black beans (1 cup cooked) Pectin, Resistant Starch 1.5 Cellulose 6 7.5 Brown rice (1 cup cooked) Trace amounts 0.5 Hemicellulose, Lignin 2–3 2.5–3.5 Popcorn (3 cups popped) Trace amounts 0.5 Hemicellulose 3 3.5 Broccoli (1 cup cooked) Pectin 1 Cellulose, Hemicellulose 4 5 Green beans (1 cup cooked) Trace amounts 0.5 Cellulose, Hemicellulose 3 3.5 Sweet potatoes (1 cup cooked) Pectin 1–1.5 Cellulose 3 4.5 Whole wheat bread (1 slice) Trace amounts 0.5 Cellulose, Hemicellulose 1 1.5 Pears (1 medium) Pectin 1 Cellulose, Hemicellulose 4 5 Almonds (1 oz) Trace amounts 0.5 Cellulose, Hemicellulose 2 2.5 10 of the best for a balance of both
Food Soluble Fiber Type(s) Soluble Fiber (g per serving) Insoluble Fiber Type(s) Insoluble Fiber (g per serving) Total Fiber (g per serving) Raspberries (1 cup) Pectin 1 Cellulose 5 6 Edamame (1 cup cooked) Pectin 1 Cellulose 5 6 Chia seeds (2 tbsp) Mucilage, Pectin 2–3 Lignin, Cellulose 3 5.5 Artichokes (1 medium) Inulin 1 Cellulose, Hemicellulose 5 6 Avocado (1 medium) Pectin ~2 Cellulose 4 6 Black beans (1 cup cooked) Pectin, Resistant Starch 1.5 Cellulose 6 7.5 Quinoa (1 cup cooked) Pectin, Saponins 1 Cellulose, Hemicellulose 3 4 Spinach (1 cup cooked) Pectin 0.5 Cellulose, Lignin 3 3.5 Prunes (1/2 cup) Pectin, Sorbitol 2 Cellulose 4 6 Figs (3 medium) Pectin 1 Cellulose 2 3 You’ll notice that the above “balance” is not equal; that’s ok; we need greater quantities of insoluble than soluble anyway, so it is as well that nature provides such.
This is the same kind of balance when we talk about “balanced hormones” (does not mean all hormones are in equal amounts; means they are in the right proportions) or “balanced microbiome” (does not mean that pathogens and friendly bacteria are in equal numbers), etc.
Some notes on the above:
About those fiber types, some of the most important soluble ones to aim for are:
- Beta-glucan: found in oats and barley, it supports heart health.
- Pectin: found in fruits like apples, citrus, and pears, it helps with cholesterol control.
- Inulin: a type of prebiotic fiber found in artichokes.
- Lignin: found in seeds and wheat bran, it has antioxidant properties.
- Resistant starch: found in beans and lentils, it acts as a prebiotic for gut health.
See also: When Is A Fiber Not A Fiber? The Food Additive You Do Want
One fiber to rule them all
Well, not entirely (we still need the others) but there is a best all-rounder:
The Best Kind Of Fiber For Overall Health?
Enjoy!
Share This Post
Related Posts
-
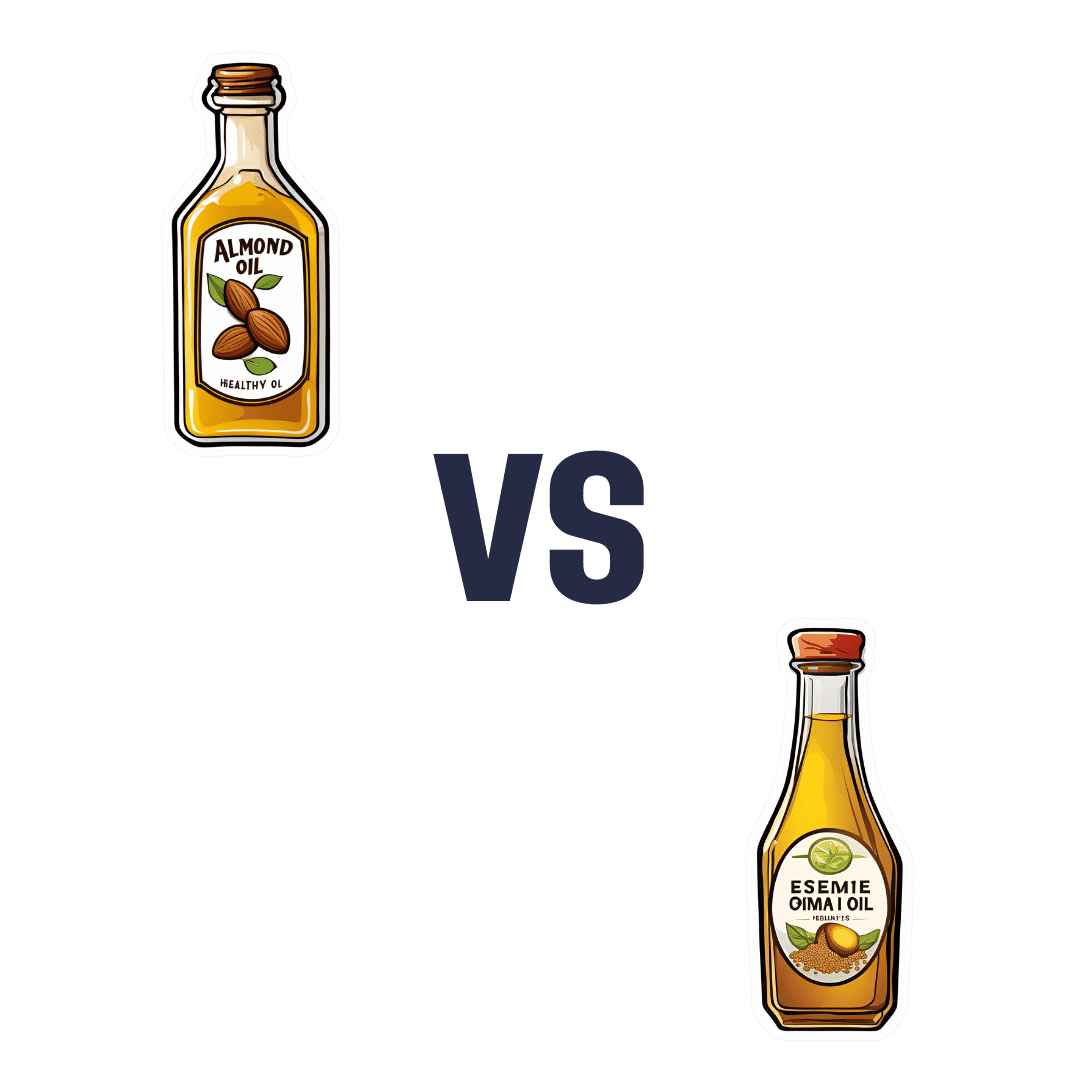
Sesame Oil vs Almond Oil – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sesame oil to almond oil, we picked the almond.
Why?
We were curious about this one! Were you, or were you confident? You see, almonds tend to blow away all the other nuts with their nutritional density, but they’re far from the oiliest of nuts, and their greatest strengths include their big dose of protein and fiber (which don’t make it into the oil), vitamins (most of which don’t make it into the oil) and minerals (which don’t make it into the oil). So, a lot will come down to the fat profile!
On which note, looking at the macros first, it’s 100% fat in both cases, but sesame oil has more saturated fat and polyunsaturated fat, while almond oil has more monounsaturated fat. Since the mono- and poly-unsaturated fats are both healthy and each oil has more of one or the other, the deciding factor here is which has the least saturated fat—and that’s the almond oil, which has close to half the saturated fat of sesame oil. As an aside, neither of them are a source of omega-3 fatty acids.
In terms of vitamins, there’s not a lot to say here, but “not a lot” is not nothing: sesame oil has nearly 2x the vitamin K, while almond oil has 28x the vitamin E*, and 2x the choline. So, another win for almond oil.
*which is worth noting, not least of all because seeds are more widely associated with vitamin E in popular culture, but it’s the almond oil that provide much more here. Not to get too distracted into looking at the values of the actual seeds and nuts, almonds themselves do have over 102x the vitamin E compared to sesame seeds.
Now, back to the oils:
In the category of minerals, there actually is nothing to say here, except you can’t get more than the barest trace of any mineral from either of these two oils. So it’s a tie on this one.
Adding up the categories makes for a clear win for almond oil!
Want to learn more?
You might like to read:
Avocado Oil vs Olive Oil – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is TikTok right? Can adding a teaspoon of cinnamon to your coffee help you burn fat?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cinnamon has been long used around the world in both sweet and savoury dishes and drinks.
But a new TikTok trend claims adding a teaspoon of cinnamon to your daily coffee (and some cocoa to make it more palatable) for one week can help you burn fat. Is there any truth to this?
Evannovostro/Shutterstock Not all cinnamon is the same
There are two types of cinnamon, both of which come from grinding the bark of the cinnamomum tree and may include several naturally occurring active ingredients.
Cassia cinnamon is the most common type available in grocery stores. It has a bitter taste and contains higher levels of one of the active ingredient cinnamaldehyde, a compound that gives cinnamon its flavour and odour. About 95% of cassia cinnamon is cinnamaldehyde.
The other is Ceylon cinnamon, which tastes sweeter. It contains about 50-60% cinnamaldehyde.
Does cinnamon burn fat? What does the research say?
A review of 35 studies examined whether consuming cinnamon could affect waist circumference, which is linked to increased body fat levels. It found cinnamon doses below 1.5 grams per day (around half a teaspoon) decreased waist circumference by 1.68cm. However, consuming more than 1.5g/day did not have a significant effect.
A meta-analysis of 21 clinical trials with 1,480 total participants found cinnamon also reduced body mass index (BMI) by 0.40kg/m² and body weight by 0.92kg. But it did not change the participants’ composition of fat or lean mass.
Another umbrella review, which included all the meta-analyses, found a small effect of cinnamon on weight loss. Participants lost an average of 0.67kg and reduced their BMI by 0.45kg/m².
The effect appears small. Radu Sebastian/Shutterstock So overall, the weight loss we see from these high-quality studies is very small, ranging anywhere from two to six months and mostly with no change in body composition.
The studies included people with different diseases, and most were from the Middle East and/or the Indian subcontinent. So we can’t be certain we would see this effect in people with other health profiles and in other countries. They were also conducted over different lengths of time from two to six months.
The supplements were different, depending on the study. Some had the active ingredient extracted from cinnamon, others used cinnamon powder. Doses varied from 0.36g to 10g per day.
They also used the two different types of cinnamon – but none of the studies used cinnamon from the grocery store.
How could cinnamon result in small amounts of weight loss?
There are several possible mechanisms.
It appears to allow blood glucose (sugar) to enter the body’s cells more quickly. This lowers blood glucose levels and can make insulin work more effectively.
It also seems to improve the way we break down fat when we need it for energy.
Finally, it may make us feel fuller for longer by slowing down how quickly the food is released from our stomach into the small intestine.
What are the risks?
Cinnamon is generally regarded as safe when used as a spice in cooking and food.
However, in recent months the United States and Australia have issued health alerts about the level of lead and other heavy metals in some cinnamon preparations.
Lead enters as a contaminant during growth (from the environment) and in harvesting. In some cases, it has been suggested there may have been intentional contamination.
Some people can have side effects from cinnamon, including gastrointestinal pain and allergic reactions.
One of the active ingredients, coumarin, can be toxic for some people’s livers. This has prompted the European Food Authority to set a limit of 0.1mg/kg of body weight.
Cassia cinnamon contains up to 1% of coumarin, and the Ceylon variety contains much less, 0.004%. So for people weighing above 60kg, 2 teaspoons (6g) of cassia cinnamon would bring them over the safe limit.
What about the coffee and cocoa?
Many people may think coffee can also help us lose weight. However there isn’t good evidence to support this yet.
An observational study found drinking one cup of regular coffee was linked to a reduction in weight that is gained over four years, but by a very small amount: an average of 0.12kg.
Good-quality cocoa and dark chocolate have also been shown to reduce weight. But again, the weight loss was small (between 0.2 and 0.4kg) and only after consuming it for four to eight weeks.
So what does this all mean?
Using cinnamon may have a very small effect on weight, but it’s unlikely to deliver meaningful weight loss without other lifestyle adjustments.
We also need to remember these trials used products that differ from the cinnamon we buy in the shops. How we store and how long we keep cinnamon might also impact or degrade the active ingredients.
And consuming more isn’t going to provide additional benefit. In fact, it could increase your risk of side effects.
So if you enjoy the taste of cinnamon in your coffee, continue to add it, but given its strong taste, you’re likely to only want to add a little.
And no matter how much we’d like this to be true, we certainly won’t gain any fat-loss benefits by consuming cinnamon on doughnuts or in buns, due to their high kilojoule count.
If you want to lose weight, there are evidence-backed approaches that won’t spoil your morning coffee.
Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cucumber vs Lychee – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cucumber to lychee, we picked the lychee.
Why?
In terms of macros, the lychee has more carbs and more fiber, but both are low glycemic index foods. Functionally a tie, though we could consider it a nominal win for cucumber.
In the category of vitamins, cucumber has more of vitamins A, B1, B5, and K, while lychee has more of vitamins B2, B3, B6, B9, C, E, and choline. In particular, cucumber has a lot more vitamin K and lychee has a lot more vitamin C. Nevertheless, in terms of overall vitamin coverage, lychee is the clear winner here.
Looking at minerals, cucumber has more calcium, magnesium, manganese, and zinc, while lychee has more copper (especially rich in this), iron, phosphorus, potassium, and selenium. Another clear win for lychee.
Both have an abundance of anti-inflammatory polyphenols, but we could find no strong argument for one being better than the other in this category, just different.
In short, both are fine options, but the more nutritionally dense is the lychee, so that’s our choice!
Want to learn more?
You might like to read:
Cucumber Extract Beats Glucosamine & Chondroitin… At 1/135th Of The Dose?!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: