Alzheimer’s: The Bad News And The Good
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Devi’s Spectrum of Hope
This is Dr. Gayatri Devi. She’s a neurologist, board-certified in neurology, pain medicine, psychiatry, brain injury medicine, and behavioral neurology.
She’s also a Clinical Professor of Neurology, and Director of Long Island Alzheimer’s Disease Center, Fellow of the American Academy of Neurology, and we could continue all day with her qualifications, awards and achievements but then we’d run out of space. Suffice it to say, she knows her stuff.
Especially when it comes to the optimal treatment of stroke, cognitive loss, and pain.
In her own words:
❝Helping folks live their best lives—by diagnosing and managing complex neurologic disorders—that’s my job. Few things are more fulfilling! For nearly thirty years, my focus has been on brain health, concussions, Alzheimer’s and other dementias, menopause related memory loss, and pain.❞
Alzheimer’s is more common than you might think
According to Dr. Devi,
❝97% of patients with mild Alzheimer’s disease don’t even get diagnosed in their internist offices, and half of patients with moderate Alzheimer’s don’t get diagnosed.
What that means is that the percentage of people that we think about when we think about Alzheimer’s—the people in the nursing home—that’s a very, very small fraction of the entirety of the people who have the condition❞
As for what she would consider the real figures, she puts it nearer 1 in 10 adults aged 65 and older.
Source: Neurologist dispels myths about Alzheimer’s disease
Her most critical advice? Reallocate your worry.
A lot of people understandably worry about a genetic predisposition to Alzheimer’s, especially if an older relative died that way.
See also: Alzheimer’s, Genes, & You
However, Dr. Devi points out that under 5% of Alzheimer’s cases are from genetics, and the majority of Alzheimer’s cases can be prevented be lifestyle interventions.
See also: Reduce Your Alzheimer’s Risk
Lastly, she wants us to skip the stigma
Outside of her clinical practice and academic work, this is one of the biggest things she works on, reducing the stigma attached to Alzheimer’s both publicly and professionally:
Alzheimer’s Disease in Physicians: Assessing Professional Competence and Tempering Stigma
Want more from Dr. Devi?
You might enjoy this interview:
Click Here If The Embedded Video Doesn’t Load Automatically!
And here’s her book:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Bird Flu Is Bad for Poultry and Dairy Cows. It’s Not a Dire Threat for Most of Us — Yet.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Headlines are flying after the Department of Agriculture confirmed that the H5N1 bird flu virus has infected dairy cows around the country. Tests have detected the virus among cattle in nine states, mainly in Texas and New Mexico, and most recently in Colorado, said Nirav Shah, principal deputy director at the Centers for Disease Control and Prevention, at a May 1 event held by the Council on Foreign Relations.
A menagerie of other animals have been infected by H5N1, and at least one person in Texas. But what scientists fear most is if the virus were to spread efficiently from person to person. That hasn’t happened and might not. Shah said the CDC considers the H5N1 outbreak “a low risk to the general public at this time.”
Viruses evolve and outbreaks can shift quickly. “As with any major outbreak, this is moving at the speed of a bullet train,” Shah said. “What we’ll be talking about is a snapshot of that fast-moving train.” What he means is that what’s known about the H5N1 bird flu today will undoubtedly change.
With that in mind, KFF Health News explains what you need to know now.
Q: Who gets the bird flu?
Mainly birds. Over the past few years, however, the H5N1 bird flu virus has increasingly jumped from birds into mammals around the world. The growing list of more than 50 species includes seals, goats, skunks, cats, and wild bush dogs at a zoo in the United Kingdom. At least 24,000 sea lions died in outbreaks of H5N1 bird flu in South America last year.
What makes the current outbreak in cattle unusual is that it’s spreading rapidly from cow to cow, whereas the other cases — except for the sea lion infections — appear limited. Researchers know this because genetic sequences of the H5N1 viruses drawn from cattle this year were nearly identical to one another.
The cattle outbreak is also concerning because the country has been caught off guard. Researchers examining the virus’s genomes suggest it originally spilled over from birds into cows late last year in Texas, and has since spread among many more cows than have been tested. “Our analyses show this has been circulating in cows for four months or so, under our noses,” said Michael Worobey, an evolutionary biologist at the University of Arizona in Tucson.
Q: Is this the start of the next pandemic?
Not yet. But it’s a thought worth considering because a bird flu pandemic would be a nightmare. More than half of people infected by older strains of H5N1 bird flu viruses from 2003 to 2016 died. Even if death rates turn out to be less severe for the H5N1 strain currently circulating in cattle, repercussions could involve loads of sick people and hospitals too overwhelmed to handle other medical emergencies.
Although at least one person has been infected with H5N1 this year, the virus can’t lead to a pandemic in its current state. To achieve that horrible status, a pathogen needs to sicken many people on multiple continents. And to do that, the H5N1 virus would need to infect a ton of people. That won’t happen through occasional spillovers of the virus from farm animals into people. Rather, the virus must acquire mutations for it to spread from person to person, like the seasonal flu, as a respiratory infection transmitted largely through the air as people cough, sneeze, and breathe. As we learned in the depths of covid-19, airborne viruses are hard to stop.
That hasn’t happened yet. However, H5N1 viruses now have plenty of chances to evolve as they replicate within thousands of cows. Like all viruses, they mutate as they replicate, and mutations that improve the virus’s survival are passed to the next generation. And because cows are mammals, the viruses could be getting better at thriving within cells that are closer to ours than birds’.
The evolution of a pandemic-ready bird flu virus could be aided by a sort of superpower possessed by many viruses. Namely, they sometimes swap their genes with other strains in a process called reassortment. In a study published in 2009, Worobey and other researchers traced the origin of the H1N1 “swine flu” pandemic to events in which different viruses causing the swine flu, bird flu, and human flu mixed and matched their genes within pigs that they were simultaneously infecting. Pigs need not be involved this time around, Worobey warned.
Q: Will a pandemic start if a person drinks virus-contaminated milk?
Not yet. Cow’s milk, as well as powdered milk and infant formula, sold in stores is considered safe because the law requires all milk sold commercially to be pasteurized. That process of heating milk at high temperatures kills bacteria, viruses, and other teeny organisms. Tests have identified fragments of H5N1 viruses in milk from grocery stores but confirm that the virus bits are dead and, therefore, harmless.
Unpasteurized “raw” milk, however, has been shown to contain living H5N1 viruses, which is why the FDA and other health authorities strongly advise people not to drink it. Doing so could cause a person to become seriously ill or worse. But even then, a pandemic is unlikely to be sparked because the virus — in its current form — does not spread efficiently from person to person, as the seasonal flu does.
Q: What should be done?
A lot! Because of a lack of surveillance, the U.S. Department of Agriculture and other agencies have allowed the H5N1 bird flu to spread under the radar in cattle. To get a handle on the situation, the USDA recently ordered all lactating dairy cattle to be tested before farmers move them to other states, and the outcomes of the tests to be reported.
But just as restricting covid tests to international travelers in early 2020 allowed the coronavirus to spread undetected, testing only cows that move across state lines would miss plenty of cases.
Such limited testing won’t reveal how the virus is spreading among cattle — information desperately needed so farmers can stop it. A leading hypothesis is that viruses are being transferred from one cow to the next through the machines used to milk them.
To boost testing, Fred Gingrich, executive director of a nonprofit organization for farm veterinarians, the American Association of Bovine Practitioners, said the government should offer funds to cattle farmers who report cases so that they have an incentive to test. Barring that, he said, reporting just adds reputational damage atop financial loss.
“These outbreaks have a significant economic impact,” Gingrich said. “Farmers lose about 20% of their milk production in an outbreak because animals quit eating, produce less milk, and some of that milk is abnormal and then can’t be sold.”
The government has made the H5N1 tests free for farmers, Gingrich added, but they haven’t budgeted money for veterinarians who must sample the cows, transport samples, and file paperwork. “Tests are the least expensive part,” he said.
If testing on farms remains elusive, evolutionary virologists can still learn a lot by analyzing genomic sequences from H5N1 viruses sampled from cattle. The differences between sequences tell a story about where and when the current outbreak began, the path it travels, and whether the viruses are acquiring mutations that pose a threat to people. Yet this vital research has been hampered by the USDA’s slow and incomplete posting of genetic data, Worobey said.
The government should also help poultry farmers prevent H5N1 outbreaks since those kill many birds and pose a constant threat of spillover, said Maurice Pitesky, an avian disease specialist at the University of California-Davis.
Waterfowl like ducks and geese are the usual sources of outbreaks on poultry farms, and researchers can detect their proximity using remote sensing and other technologies. By zeroing in on zones of potential spillover, farmers can target their attention. That can mean routine surveillance to detect early signs of infections in poultry, using water cannons to shoo away migrating flocks, relocating farm animals, or temporarily ushering them into barns. “We should be spending on prevention,” Pitesky said.
Q: OK it’s not a pandemic, but what could happen to people who get this year’s H5N1 bird flu?
No one really knows. Only one person in Texas has been diagnosed with the disease this year, in April. This person worked closely with dairy cows, and had a mild case with an eye infection. The CDC found out about them because of its surveillance process. Clinics are supposed to alert state health departments when they diagnose farmworkers with the flu, using tests that detect influenza viruses, broadly. State health departments then confirm the test, and if it’s positive, they send a person’s sample to a CDC laboratory, where it is checked for the H5N1 virus, specifically. “Thus far we have received 23,” Shah said. “All but one of those was negative.”
State health department officials are also monitoring around 150 people, he said, who have spent time around cattle. They’re checking in with these farmworkers via phone calls, text messages, or in-person visits to see if they develop symptoms. And if that happens, they’ll be tested.
Another way to assess farmworkers would be to check their blood for antibodies against the H5N1 bird flu virus; a positive result would indicate they might have been unknowingly infected. But Shah said health officials are not yet doing this work.
“The fact that we’re four months in and haven’t done this isn’t a good sign,” Worobey said. “I’m not super worried about a pandemic at the moment, but we should start acting like we don’t want it to happen.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
What Is Earwax & Should You Get Rid Of It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Earwax (cerumen) forms in the outer ear canal when dead skin cells mix with oily sweat (a specialty of the apocrine glands) and sebum, a fatty substance mostly associated with facial oiliness. But, does it have a purpose, or is it just a waste product?
Nature is (mostly) best in this case
Earwax plays an important role in ear health, acting as a natural lubricant that prevents dryness and itchiness, trapping debris and microbes, and forming a protective barrier for the ear canal. It even contains proteins that help fight bacterial infections.
As for removal: the body has a natural mechanism for removing excess earwax: as skin cells grow, they migrate outward, carrying earwax with them.
In contrast, manual removal of earwax can do more harm than good. Using swabs or other items often pushes wax deeper, risks damaging the ear canal, and disrupts its protective barrier, potentially leading to infection.
Ear candling, which claims to extract earwax, not only does not work (its main premise has been actively disproven and clinical evidence shows unequivocally that it doesn’t work by any mysterious method either; it just plain doesn’t work), but also can cause injuries and will tend to leave more harmful debris behind than was there originally.
For those prone to earwax buildup, over-the-counter eardrops can help soften wax for natural removal, and medical professionals have safe methods to clear blockages if necessary.
To maintain ear health, it’s best to clean only the outer ear with a damp cloth, limit the use of earplugs or earbuds, and generally leave earwax alone unless it causes discomfort or hearing issues.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Ear Candling: Is It Safe & Does It Work? ← the answer is “no and no”, but the science may interest you
Take care!
Share This Post
-
When Carbs, Proteins, & Fats Switch Metabolic Roles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Strange Things Happening In The Islets Of Langerhans
It is generally known and widely accepted that carbs have the biggest effect on blood sugar levels (and thus insulin response), fats less so, and protein least of all.
And yet, there was a groundbreaking study published yesterday which found:
❝Glucose is the well-known driver of insulin, but we were surprised to see such high variability, with some individuals showing a strong response to proteins, and others to fats, which had never been characterized before.
Insulin plays a major role in human health, in everything from diabetes, where it is too low*, to obesity, weight gain and even some forms of cancer, where it is too high.
These findings lay the groundwork for personalized nutrition that could transform how we treat and manage a range of conditions.❞
*saying ”too low” here is potentially misleading without clarification; yes, Type 1 Diabetics will have too little [endogenous] insulin (because the pancreas is at war with itself and thus isn’t producing useful quantities of insulin, if any). Type 2, however, is more a case of acquired insulin insensitivity, because of having too much at once too often, thus the body stops listening to it, “boy who cried wolf”-style, and the pancreas also starts to get fatigued from producing so much insulin that’s often getting ignored, and does eventually produce less and less while needing more and more insulin to get the same response, so it can be legitimately said “there’s not enough”, but that’s more of a subjective outcome than an objective cause.
Back to the study itself, though…
What they found, and how they found it
Researchers took pancreatic islets from 140 heterogenous donors (varied in age and sex; ostensibly mostly non-diabetic donors, but they acknowledge type 2 diabetes could potentially have gone undiagnosed in some donors*) and tested cell cultures from each with various carbs, proteins, and fats.
They found the expected results in most of the cases, but around 9% responded more strongly to the fats than the carbs (even more strongly than to glucose specifically), and even more surprisingly 8% responded more strongly to the proteins.
*there were also some known type 2 diabetics amongst the donors; as expected, those had a poor insulin response to glucose, but their insulin response to proteins and fats were largely unaffected.
What this means
While this is, in essence, a pilot study (the researchers called for larger and more varied studies, as well as in vivo human studies), the implications so far are important:
It appears that, for a minority of people, a lot of (generally considered very good) antidiabetic advice may not be working in the way previously understood. They’re going to (for example) put fat on their carbs to reduce the blood sugar spike, which will technically still work, but the insulin response is going to be briefly spiked anyway, because of the fats, which very insulin response is what will lower the blood sugars.
In practical terms, there’s not a lot we can do about this at home just yet—even continuous glucose monitors won’t tell us precisely, because they’re monitoring glucose, not the insulin response. We could probably measure everything and do some math and work out what our insulin response has been like based on the pace of change in blood sugar levels (which won’t decrease without insulin to allow such), but even that is at best grounds for a hypothesis for now.
Hopefully, more publicly-available tests will be developed soon, enabling us all to know our “insulin response type” per the proteome predictors discovered in this study, rather than having to just blindly bet on it being “normal”.
Ironically, this very response may have hidden itself for a while—if taking fats raised insulin response without raising blood sugar levels, then if blood sugar levels are the only thing being measured, all we’ll see is “took fats at dinner; blood sugars returned to normal more quickly than when taking carbs without fats”.
You can read the study in full here:
Proteomic predictors of individualized nutrient-specific insulin secretion in health and disease
Want to know more about blood sugar management?
You might like to catch up on:
- 10 Ways To Balance Your Blood Sugars
- Track Your Blood Sugars For Better Personalized Health
- How To Turn Back The Clock On Insulin Resistance
Take care!
Share This Post
Related Posts
-
5 Ways To Beat Cancer (And Other Diseases)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Systematic Approach To Healthy Eating
This is Dr. William Li. He’s a physician, cancer researcher, and educator. He also founded the Angiogenesis Foundation back in 1994.
We recently reviewed one of his books, “Eat To Beat Disease”.
He has another book that we haven’t reviewed at time of writing, “Eat To Beat Your Diet“, which you might like to check out.
What does he want us to know?
He wants us to know how to eat to beat cancer and other diseases, by means of five specific angles:
Angiogenesis
This is about replacing blood vessels, which of course happens all the time, but it becomes a problem when it is feeding a cancer in the process.
Here, based on Dr. Li’s work, is what can be done about it:
A List of Anti-Angiogenic Foods for a Cancer-Fighting Diet
Regeneration
Generally speaking, we want to replace healthy cells early, because if we wait until they get damaged, then that damage will be copied forwards. As well as intermittent fasting, there are other things we can do to promote this—even, Dr. Li’s research shows, for stem cells:
Doctor’s Tip: Regeneration (stem cells)—one of your body’s five defense systems
Microbiome health
Healthy gut, healthy rest of the body. We’ve written about this before:
Making Friends With Your Gut (You Can Thank Us Later)
DNA protection
DNA gets unravelled and damaged with age, the telomere caps get shorter, and mistakes get copied forward. So there more we can protect our DNA, the longer we can live healthily. There are many ways to do this, but Dr. Li was one of the first to bring to light the DNA-protecting benefits of kiwi fruit:
Immunity
Paradoxically, what’s good for your immune system (making it stronger) also helps to protect against autoimmune diseases (for most people, for the most part).
In short: it’s good to have an immune system that’s powerful not just in its counterattacks, but also in its discerning nature. There are dietary and other lifestyle approaches to both, and they’re mostly the same things:
Beyond Supplements: The Real Immune-Boosters!
and thus see also:
Want to know more?
You might enjoy his blog or podcast, and here’s his TED talk:
Want to watch it, but not right now? Bookmark it for later
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Planning Festivities Your Body Won’t Regret
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Festive Dilemma
For many, Christmas is approaching. Other holidays abound too, and even for the non-observant, it’d be hard to escape seasonal jollities entirely.
So, what’s the plan?
- Eat, drink, and be merry, and have New Year’s Resolutions for the first few days of January before collapsing in a heap?
- Approach the Yuletide with Spartan abstemiousness and miss all the fun while simultaneously annoying your relatives?
Let’s try to find a third approach instead…
What’s festive and healthy?
We’re doing this article this week, because many people will be shopping already, making plans, and so forth. So here are some things to bear in mind:
Make your own mindful choices
Coca-Cola company really did a number on Christmas, but it doesn’t mean their product is truly integral to the season. Same goes for many other things that flood the stores around this time of year. So much sugary confectionary! But remember, they’re not the boss of you. If you wouldn’t buy it ordinarily, why are you buying it now? Do you actually even want it?
If you really do, then you do you, but mindful choices will invariably be healthier than “because there were three additional aisles of confectionary now so I stopped and looked and picked some things”.
Pick your battles
If you’re having a big family gathering, likely there will be occasions with few healthy options available. But you can decide what’s most important for you to avoid, perhaps picking a theme, e.g:
- No alcohol this year, or
- No processed sugary foods, or
- Eat/drink whatever, but practice intermittent fasting
Some resources:
Fight inflammation
This is a big one so it deserves its own category. In the season of sugar and alcohol and fatty meat, inflammation can be a big problem to come around and bite us in the behind. We’ve written on this previously:
Positive dieting
In other words, less of a focus on what to exclude, and more of a focus on what to include in your diet. Fruity drinks and sweets are common at this time of year, but you know what’s also fruity? Fruit!
And it can be festive, too! Berries are great, and those tiny orange-like fruits that may be called clementines or tangerines or satsumas or, as Aldi would have it, “easy peelers”. Apple and cinnamon are also a great combination that both bring sweetness without needing added sugar.
And as for mains? Make your salads that bit fancier, get plenty of greens with your main, have hearty soups and strews with lentils and beams!
See also: Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Your gut will thank us later!
Get moving!
That doesn’t mean you have to beat the New Year rush to the gym (unless you want to!). But it could mean, for example, more time in your walking shoes (or dancing shoes! With a nod to today’s sponsor) and less time in the armchair.
See also: The doctor who wants us to exercise less; move more
Lastly…
Remember it’s supposed to be fun! And being healthy can be a lot more fun than suffering because of unfortunate choices that we come to regret.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Longans vs Lychees – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
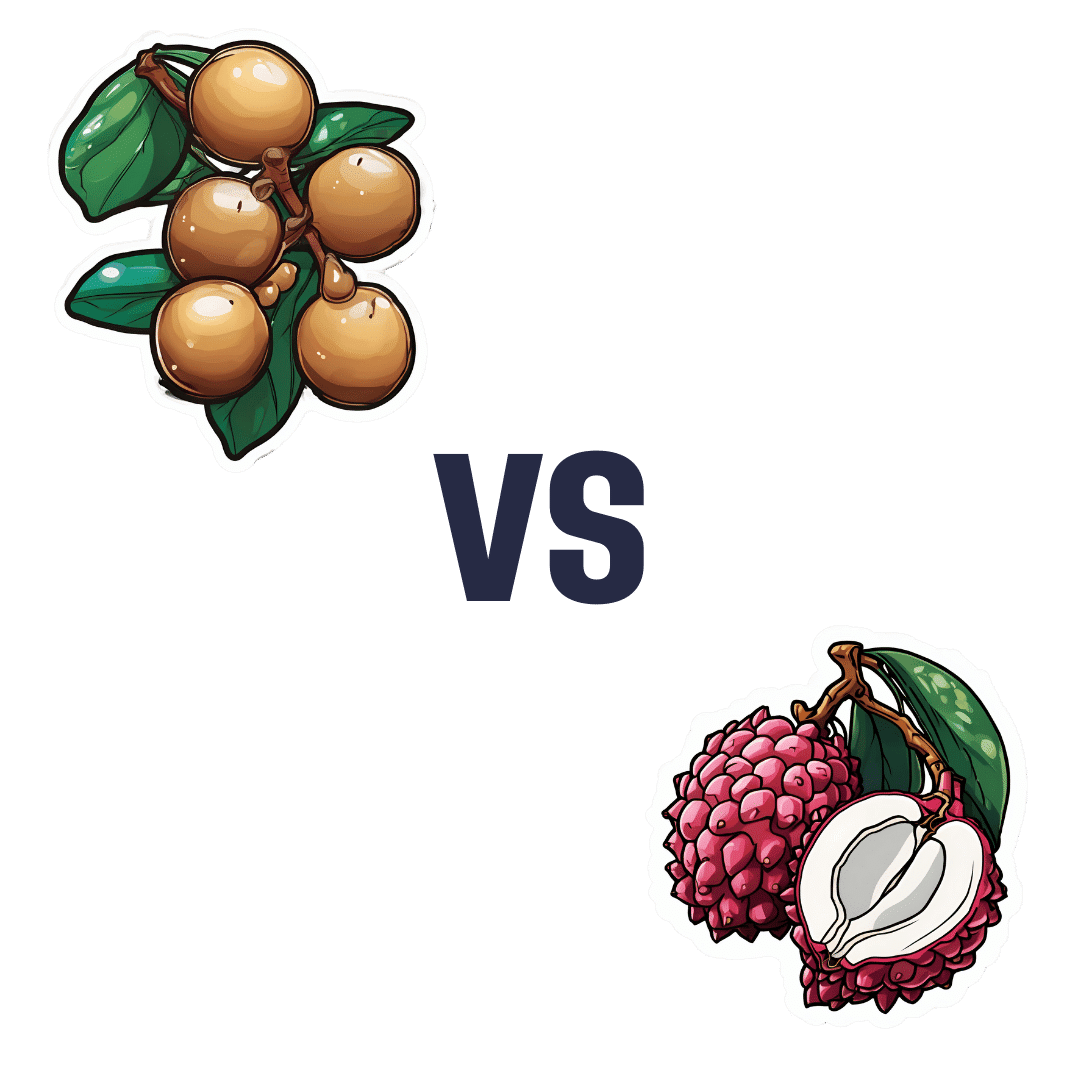
When comparing longans to lychees, we picked the lychees.
Why?
These two fruits are more closely related than they look from the outside, both being members of the soapberry family. However, there are some differences:
In terms of macros, longans have more protein while lychees have more carbs, and they are equal on fiber, giving longans the lower glycemic index. They’re both good, but longans nominally take the win on this one.
When it comes to vitamins, longans have more of vitamins B1, B2, and C, while lychees have more of vitamins B3, B6, B9, E, K, and choline, making for a respectable win for lychees in this category.
In the category of minerals, longans have more copper and potassium, while lychees have more calcium, iron, manganese phosphorus, and zinc. Thus, a win for lychees here too.
It’s worth looking at polyphenols too—lychees have around 10x more, which is notable.
Adding up the categories makes for an overall win for lychees, but by all means enjoy either or both! Diversity is good.
Want to learn more?
You might like to read:
Replacing Sugar: Top 10 Anti-Inflammatory Sweet Foods ← longans and lychees both make the list
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: