Ear Candling: Is It Safe & Does It Work?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Does This Practice Really Hold A Candle To Evidence-Based Medicine?
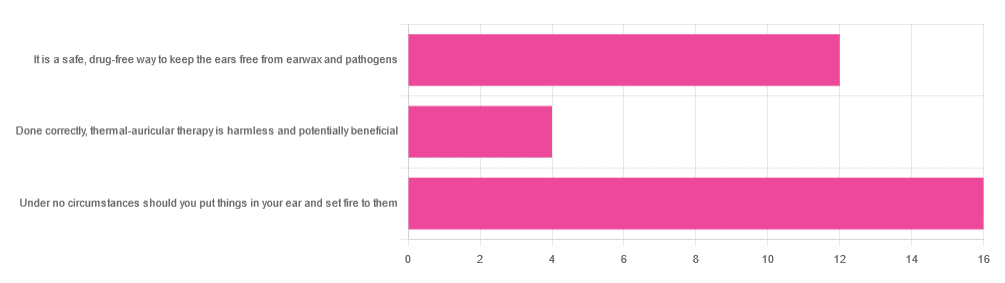
In Tuesday’s newsletter, we asked you your opinion of ear candling, and got the above-depicted, below-described set of responses:
- Exactly 50% said “Under no circumstances should you put things in your ear and set fire to them”
- About 38% said “It is a safe, drug-free way to keep the ears free from earwax and pathogens”
- About 13% said “Done correctly, thermal-auricular therapy is harmless and potentially beneficial”
This means that if we add the two positive-to-candling answers together, it’s a perfect 50:50 split between “do it” and “don’t do it”.
(Yes, 38%+13%=51%, but that’s because we round to the nearest integer in these reports, and more precisely it was 37.5% and 12.5%)
So, with the vote split, what does the science say?
First, a quick bit of background: nobody seems keen to admit to having invented this. One of the major manufacturers of ear candles refers to them as “Hopi” candles, which the actual Hopi tribe has spent a long time asking them not to do, as it is not and never has been used by the Hopi people. Other proposed origins offered by advocates of ear candling include Traditional Chinese Medicine (not used), Ancient Egypt (no evidence of such whatsoever), and Atlantis:
Quackwatch | Why Ear Candling Is Not A Good Idea
It is a safe, drug-free way to keep the ears free from earwax and pathogens: True or False?
False! In a lot of cases of alternative therapy claims, there’s an absence of evidence that doesn’t necessarily disprove the treatment. In this case, however, it’s not even an open matter; its claims have been actively disproven by experimentation:
- It doesn’t remove earwax; on the contrary, experimentation “showed no removal of cerumen from the external auditory canal. Candle wax was actually deposited in some“
- It doesn’t remove pathogens, and the proposed mechanism of action for removing pathogens, that of the “chimney effect”: the idea that the burning candle creates a vacuum that draws wax out of the ear along with debris and bacteria, simply does not work; on the contrary, “Tympanometric measurements in an ear canal model demonstrated that ear candles do not produce negative pressure”.
- It isn’t safe; on the contrary, “Ear candles have no benefit in the management of cerumen and may result in serious injury”
In a medium-sized survey (n=122), the following injuries were reported:
- 13 x burns
- 7 x occlusion of the ear canal
- 6 x temporary hearing loss
- 3 x otitis externa (this also called “swimmer’s ear”, and is an inflammation of the ear, accompanied by pain and swelling)
- 1 x tympanic membrane perforation
Indeed, authors of one paper concluded:
❝Ear candling appears to be popular and is heavily advertised with claims that could seem scientific to lay people. However, its claimed mechanism of action has not been verified, no positive clinical effect has been reliably recorded, and it is associated with considerable risk.
No evidence suggests that ear candling is an effective treatment for any condition. On this basis, we believe it can do more harm than good and we recommend that GPs discourage its use❞
Source: Canadian Family Physician | Ear Candling
Under no circumstances should you put things in your ear and set fire to them: True or False?
True! It’s generally considered good advice to not put objects in general in your ears.
Inserting flaming objects is a definite no-no. Please leave that for the Cirque du Soleil.
You may be thinking, “but I have done this and suffered no ill effects”, which seems reasonable, but is an example of survivorship bias in action—it doesn’t make the thing in question any safer, it just means you were one of the one of the ones who got away unscathed.
If you’re wondering what to do instead… Ear oils can help with the removal of earwax (if you don’t want to go get it sucked out at a clinic—the industry standard is to use a suction device, which actually does what ear candles claim to do). For information on safely getting rid of earwax, see our previous article:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Salt Sugar Fat – by Michael Moss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You are probably already aware that food giants put unhealthy ingredients in processed food. So what does this book offer of value?
Sometimes, better understanding leads to better movation. In this case, while a common (reasonable) view has been:
“The food giants fill their food with salt, sugar, and fat, because it makes that food irresistibly delicious”
…but that doesn’t exactly put us off the food, does it? It just makes it a guilty pleasure. Ah yes, the irresistible McDouble Dopamineburger. The time-honored tradition of Pizza Night; a happy glow; a special treat.
What Pulitzer-winning author Michael Moss brings to us is different.
He examines not just how they hooked us, but why. And the answer is not merely the obvious “profit and greed”, but also “survival, under capitalism”. That without regulation forcing companies to keep salt/sugar/fat levels down, companies that have tried to do so voluntarily have quickly had to u-turn to regain any hope of competitiveness.
He also looks at how the salt/sugar/fat components are needed to mask the foul taste of the substandard ingredients they use to maintain lower costs… Processed food, without the heavy doses of salt/sugar/fat, is not anywhere close to what you might make at home. Industry will cut costs where it can.
Bottom line: if you need a push to kick the processed food habit, this is the book that will do it.
Click here to check out Salt Sugar Fat, and reclaim your health!
Share This Post
-
The Drug & Supplement Combo That Reverses Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So far, its effects have been dramatic (in a good way) in mice; human trials are now underway.
How does it work?
It builds from previous work, in which a Japanese research team created an “anti-aging vaccine”, that responded to a problem more specific than aging as a whole, namely atherosclerosis.
They found that a certain* protein was upregulated (i.e., it was made at a greater rate resulting in greater quantities) in patients (mouse and human alike) with atherosclerosis. So, they immunized the mice against that protein, and long story short, everything improved for them, from their atherosclerosis to general markers of aging—including growing back fur that had been lost due to age-related balding (just like in humans). They also lived longer, as is to be expected of a mouse who is now biologically younger.
*To avoid being mysterious: it was glycoprotein nonmetastatic melanoma protein B, known to its friends as GPNMB.
You may be wondering: how can one be immunized against a protein? If so, do bear in mind, a virus is also a protein. In this case, they developed an RNA vaccine, that works in a similar way to the COVID vaccines we all know and love (albeit with a different target).
You can read about this in abundant detail here: Senolytic vaccination improves normal and pathological age-related phenotypes and increases lifespan in progeroid mice
Hot on the heels of that, new approaches were found, including…
The combination
We’ll not keep you waiting; the combination is dasatinib plus quercetin, or else fisetin alone.
It’s about killing senescent (aging) “zombie cells” while sparing healthy cells, which that drug (dasatinib) and those supplements (quercetin and fisetin) do.
The researchers noted:
❝Senescent cells are resistant to apoptosis, which is governed through the upregulation of senescent cell anti-apoptotic pathways (SCAPs). Compounds were subsequently identified that disrupted the SCAPs, inducing death of senescent cells while leaving healthy cells unaffected. Forty-six potential senolytic agents were discovered through this process. To advance translational efforts, the majority of research has focused on agents with known safety profiles and limited off-target effects (Kirkland and Tchkonia, 2020).
The best characterized senolytic agents are dasatinib, a tyrosine kinase inhibitor approved for use in humans for cancer treatment, and quercetin, a naturally occurring plant flavonoid. The agents have a synergistic effect, making their combination more potent for senescent cell clearance (Zhu et al., 2015). As senescent cells do not divide and accumulate over a period of weeks, they can be administered using an intermittent approach, which further serves to reduce the risk of side effects (Kirkland and Tchkonia, 2020).
In preclinical trials, the combination of dasatinib and quercetin (D + Q) have been found to alleviate numerous chronic medical conditions including vascular stiffness, osteoporosis, frailty, and hepatic stenosis❞
Source: A geroscience motivated approach to treat Alzheimer’s disease: Senolytics move to clinical trials
As to how they expanded on this research:
❝In our study, oral D + Q were intermittently administered to tau transgenic mice with late-stage pathology (approximated to a 70-year-old human with advanced AD) (Musi et al., 2018). The treatment effectively reduced cellular senescence and associated senescence-associated secretory phenotype incidence. The 35 % reduction in neurofibrillary tangles was accompanied by enhanced neuron density, decreased ventricular enlargement, diminished tau accumulation, and restoration of aberrant cerebral blood flow. A subsequent preclinical study validated the findings, reporting that intermittently administered D + Q cleared senescent cells in the central nervous system, reduced amyloid-β plaques, attenuated neuroinflammation, and enhanced cognition❞
Source: Ibid.
And now taking it to humans:
❝The first clinical trial of D + Q for early-stage Alzheimer’s Disease (AD) has completed enrollment (Gonzales et al., 2021). The primary aim of the open-label pilot study was to examine the central nervous system penetrance of D and Q in a small sample of older adults with early-stage AD (NCT04063124). In addition, two placebo-controlled trials of D + Q for neurodegenerative disease are underway (NCT04685590 and NCT04785300).
One of the trials in development is a multi-site, double-blind, randomized, placebo-controlled study of senolytic therapy in older adults with amnestic mild cognitive impairment (MCI) or early-stage dementia (Clinical Dementia Rating Scale (CDR) Global 0.5–1) due to AD (elevated CSF total tau/Aβ42 ratio).
The treatment regimen will consist of 12-weeks of intermittently administered oral D + Q.❞
Source: Ibid.
The study is actually completed now, but its results are not yet published (again, at time of writing). Which means: they have the data, and now they’re writing the paper.
We look forward to providing an update about that, when the paper is published!
In the meantime…
Dasatinib is a drug usually prescribed to people with certain kinds of leukemia, and suffice it to say, it’s prescription-only. And unlike drugs that are often prescribed off-label (such as metformin for weight loss), getting your doctor to prescribe you an anticancer drug is unlikely unless you have the cancer in question.
You may be wondering: how is an anticancer drug helpful against aging? And the answer is that cancer and aging are very interrelated, and both have to do with “these old cells just won’t die, and are using the resources needed for young healthy cells”. So in both cases, killing those “zombie cells” while sparing healthy ones, is what’s needed. However, your doctor will probably not buy that as a reason to prescribe you a drug that is technically chemotherapy.
Quercetin, on the other hand, is a readily-available supplement, as is fisetin, and both have glowing (in a good way) safety profiles.
Want to know more?
You can read more about each of quercetin and fisetin (including how to get them), here:
Enjoy!
Share This Post
-
How weight bias in health care can harm patients with obesity: Research
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Patients who weigh more than what medical authorities generally consider healthy often avoid seeing doctors for fear of being judged, insulted or misdiagnosed, decades of research find. Meanwhile, academic studies consistently show many health care professionals discriminate against heavier patients and that weight bias can drive people with obesity to gain weight.
Weight bias refers to negative attitudes, stereotypes and discrimination aimed at individuals with excess body fat. When scholars reviewed 41 studies about weight bias in health care, published from 1989 to 2021, they found it comes in many forms: contemptuous language, inappropriate gestures, expressing a preference for thinner patients, avoiding physical touch and eye contact, and attributing all of a person’s health issues to their weight.
“Weight bias has been reported in physicians, nurses, dietitians, physiotherapists, and psychologists, as well as nutritionists and exercise professionals, and it is as pervasive among medical professionals as it is within the general population,” write the authors of the research review, published in 2021 in the journal Obesity.
That’s a problem considering an estimated 4 out of 10 U.S. adults aged 20 years and older have obesity, a complex and often misunderstood illness that the American Medical Association voted in 2013 to recognize as a disease. By 2030, half of U.S. adults will have obesity, researchers project in a 2020 paper in the International Journal of Epidemiology.
Worldwide, the obesity rate among adults aged 18 and older was 13% in 2016, according to the World Health Organization. If current trends continue, the World Obesity Federation projects that, by 2035, 51% of the global population will be living with overweight or obesity.
The harms of weight bias
Weight stigma — the societal devaluation of people perceived to be carrying excess weight — drives weight bias. It’s so physically and emotionally damaging that a panel of 36 international experts issued a consensus statement in 2020 to raise awareness about and condemn it. Dozens of medical and academic organizations, including 15 scholarly journals, endorsed the document, published in Nature Medicine.
The release of a consensus statement is a significant event in research, considering it represents the collective position that experts in a particular field have taken on an issue, based on an analysis of all the available evidence.
Research to date indicates heavier individuals who experience weight bias and stigma often:
- Avoid doctors and other health care professionals, skipping routine screenings as well as needed treatments.
- Change doctors frequently.
- Are at a higher risk for depression, anxiety, mood disorders and other mental health problems.
- Avoid or put off exercise.
- Consume more food and calories.
- Gain weight.
- Have disrupted sleep.
The consensus statement notes that educating health care providers, journalists, policymakers and others about obesity is key to changing the narrative around the disease.
“Weight stigma is reinforced by misconceived ideas about body-weight regulation and lack of awareness of current scientific evidence,” write the experts, led by Francesco Rubino, the chair of metabolic and bariatric surgery at Kings College London.
“Despite scientific evidence to the contrary, the prevailing view in society is that obesity is a choice that can be reversed by voluntary decisions to eat less and exercise more. These assumptions mislead public health policies, confuse messages in popular media, undermine access to evidence-based treatments, and compromise advances in research.”
Weight bias and stigma appear to stimulate the secretion of the stress hormone cortisol and promote weight gain, researchers write in a 2016 paper published in Obesity.
A. Janet Tomiyama, a psychology professor at UCLA who directs the university’s Dieting, Stress, and Health research lab, describes weight stigma as “a ‘vicious cycle’ — a positive feedback loop wherein weight stigma begets weight gain.”
“This happens through increased eating behavior and increased cortisol secretion governed by behavioral, emotional, and physiological mechanisms, which are theorized to ultimately result in weight gain and difficulty of weight loss,” Tomiyama writes in her 2014 paper, “Weight Stigma is Stressful. A Review of Evidence for the Cyclic Obesity/Weight-Based Stigma Model.”
The consensus statement spotlights 13 recommendations for eliminating weight bias and stigma, some of which are specifically aimed at health care providers, the media, researchers or policymakers. One of the recommendations for the health care community: “[Health care providers] specialized in treating obesity should provide evidence of stigma-free practice skills. Professional bodies should encourage, facilitate, and develop methods to certify knowledge of stigma and its effects, along with stigma-free skills and practices.”
The one recommendation for the media: “We call on the media to produce fair, accurate, and non-stigmatizing portrayals of obesity. A commitment from the media is needed to shift the narrative around obesity.”
Why obesity is a complicated disease
It’s important to point out that having excess body fat does not, by itself, mean an individual is unhealthy, researchers explain in a 2017 article in The Conversation, which publishes research-based news articles and essays. But it is a major risk factor for cardiovascular disease, including stroke, as well as diabetes, some types of cancer, and musculoskeletal disorders such as osteoarthritis.
Doctors often look at patients’ body mass index — a number that represents their weight in relation to their height — to gauge the amount of fat on their bodies. A BMI of 18.5 to 24.9 is ideal, according to the U.S. Centers for Disease Control and Prevention. A BMI of 25.0 to 29.9, indicates excess body fat, or “overweight,” while a BMI of 30 and above indicates obesity.
In June, the American Medical Association announced a new policy clarifying how BMI can be used to diagnose obesity. Because it’s an imperfect measure for body fat, the organization suggests BMI be used in conjunction with other measures such as a patient’s waist circumference and skin fold thickness.
Two specialists who have been working for years to dispel myths and misconceptions about obesity are Fatima Cody Stanford, an obesity physician and associate professor at Harvard Medical School, and Rebecca Puhl, the deputy director of the Rudd Center for Food Policy and Obesity at the University of Connecticut.
Cody Stanford has called obesity “a brain disease” because the brain tells the body how much to eat and what to do with the food consumed. One pathway in the brain directs the body to eat less and store less fat, she explains in a February 2023 podcast produced by the American Medical Association.
“For people that signal really great down this pathway, they tend to be very lean, not struggle with their weight in the same way that people that have excess weight do,” she says during the podcast, adding that people with obesity receive signals from an alternate pathway that “tells us to eat more and store more.”
Academic studies demonstrate that a wide variety of factors can affect weight regulation, including sleep quality and duration, gut health, genetics, medication, access to healthy foods and even early life experiences.
For example, a 2020 paper in the journal JAMA Network Open suggests female infants born by cesarean delivery have a higher risk of obesity during adulthood than female infants born by vaginal delivery. The study of 33,226 U.S. women born between 1946 and 1964 found that a cesarean delivery is associated with an 11% higher risk of developing obesity and a 46% higher risk of developing type 2 diabetes.
Scholars have also found that traumatic childhood experiences such as abuse and neglect are linked to adult obesity, according to a research review published in 2020.
Income inequality seems to play a role as well. When researchers from the Johns Hopkins Bloomberg School of Public Health studied the link between income inequality and obesity for a sample of 36,665 U.S. adults, they discovered women with lower incomes are more likely to have obesity than women with higher incomes.
Their analysis indicates the opposite is true for men, whose odds of obesity rise with their income, the researchers write in a 2021 paper in the International Journal of Environmental Research and Public Health.
Weight bias among doctor trainees
While scholars have learned a lot about obesity and weight bias in recent decades, the information might not be reaching people training to become doctors. A study published in October finds that some resident physicians believe obesity to be the result of poor choices and weak willpower.
Researchers asked 3,267 resident physicians who graduated from a total of 49 U.S. medical schools a series of questions to gauge their knowledge of obesity and attitudes toward heavier patients. What they learned: Nearly 40% of resident physicians agreed with the statement, “Fat people tend to be fat pretty much through their own fault.” Almost half agreed with the statement, “Some people are fat because they have no willpower.”
The study also reveals that about one-third of participants said they “feel more irritated when treating an obese patient than a non-obese patient.”
“Notably, more than a quarter of residents expressed slight-to-strong agreement with the item ‘I dislike treating obese patients,’” the researchers write.
Another takeaway from the paper: Resident physicians specializing in orthopedic surgery, anesthesiology and urology expressed the highest levels of dislike of heavier patients. Of the 16 medical specialties represented, residents in family medicine, psychiatry and pediatrics reported the lowest levels of dislike.
Kimberly Gudzune, medical director of the American Board of Obesity Medicine, asserts that doctors and medical students need to be educated about obesity. The topic “is grossly neglected” in medical schools and medical training programs worldwide, research has found.
Many physicians don’t understand obesity, Gudzune explains in a July 2023 interview on the internal medicine podcast “The Curbsiders.”
“I think back to when I was a medical student, when I was a resident, I really didn’t learn much about obesity and how to treat it, yet it’s a problem that affects the majority of our patients,” she tells podcast listeners. “I think there’s a lot of evidence out there showing that primary care physicians don’t really know where to start.”
In 2011, the American Board of Obesity Medicine established a program through which doctors could become certified in obesity medicine. Since then, a total of 6,729 U.S. doctors have earned certification, the vast majority of whom specialize in family and internal medicine.
What health care providers think
The experts who created the consensus statement on weight bias and stigma noted health care providers’ shortcomings in the document. They write that the common themes they discovered in the research include “contemptuous, patronizing, and disrespectful treatment” of patients, a lack of training, poor communication and assumptions about weight gain.
Puhl, the deputy director of the Rudd Center at the University of Connecticut, is a pioneer in weight bias research and one of the experts who wrote the consensus statement. During an episode of “The Leading Voices in Food,” a podcast created by Duke University’s World Food Policy Center, she shares details about what she has learned over the years.
“[Health care providers’] views that patients with obesity are lazy or lacking control, are to blame for their weight or noncompliant with treatment,” she says during the interview. “We know, for example, that some physicians spend less time in their appointments with patients [who] have a larger body size. They give them less education about health. They’re more reluctant to perform certain screenings. They talk about treating patients with obesity as being a greater waste of their time than providing care to thinner patients. And we know that patients seem to be aware of these biases from providers and that can really contribute to patients avoiding health care because they just don’t want to repeat those negative experiences of bias.”
To set the record straight, the experts who wrote the the consensus statement listed the following five common assumptions as being “at odds with a definitive body of biological and clinical evidence.”
1. Body weight = calories in – calories out.
This equation oversimplifies the relationship between body weight and energy consumed and used, the experts write. “Both variables of the equation depend on factors additional to just eating and exercising. For instance, energy intake depends on the amount of food consumed, but also on the amount of food-derived energy absorbed through the gastrointestinal tract, which in turn is influenced by multiple factors, such as digestive enzymes, bile acids, microbiota, gut hormones, and neural signals, none of which are under voluntary control.”
2. Obesity is primarily caused by voluntary overeating and a sedentary lifestyle.
According to the experts, overeating and forgoing exercise might be symptoms of obesity rather than the root causes. There are many possible causes and contributors “including geneticand epigenetic factors, foodborne factors, sleep deprivation and circadian dysrhythmia, psychological stress, endocrine disruptors, medications, and intrauterine and intergenerational effects. These factors do not require overeating or physical inactivity to explain excess weight.” they write.
3. Obesity is a lifestyle choice.
“People with obesity typically recognize obesity as a serious health problem, rather than a conscious choice,” the experts write. “Given the negative effects of obesity on quality of life, the well-known risks of serious complications and reduced life expectancy associated with it, it is a misconception to define obesity as a choice.”
4. Obesity is a condition, not a disease.
The criteria generally used to determine disease status “are clearly fulfilled in many individuals with obesity as commonly defined, albeit not all,” the experts explain. “These criteria include specific signs or symptoms (such as increased adiposity), reduced quality of life, and/or increased risk of further illness, complications, and deviation from normal physiology — or well-characterized pathophysiology (for example, inflammation, insulin resistance, and alterations of hormonal signals regulating satiety and appetite).”
5. Severe obesity is usually reversible by voluntarily eating less and exercising more.
“A large body of clinical evidence has shown that voluntary attempts to eat less and exercise more render only modest effects on body weight in most individuals with severe obesity,” the experts write. “When fat mass decreases, the body responds with reduced resting energy expenditure and changes in signals that increase hunger and reduce satiety (for example, leptin, ghrelin). These compensatory metabolic and biologic adaptations promote weight regain and persist for as long as persons are in the reduced-energy state, even if they gain some weight back.”
Health care facility improvements
The expert panel also determined that many health care facilities aren’t equipped to treat people with obesity. Examination gowns, blood pressure cuffs, chairs and examination tables often are too small, patients have reported.
When researchers from the University of Minnesota, Minneapolis Veterans Affairs Medical Center and Mayo Clinic studied the quality of care that patients with obesity receive, they learned that a clinic’s physical environment can have a big effect on a patient’s experience.
They write in a 2015 study published in Obesity Reviews: “Waiting room chairs with armrests can be uncomfortable or too small. Equipment such as scales, blood pressure cuffs, examination gowns and pelvic examination instruments are often designed for use with smaller patients. When larger alternatives are not available, or are stored in a place that suggests infrequent use, it can signal to patients that their size is unusual and that they do not belong. These experiences, which are not delivered with malicious intent, can be humiliating.”
When medical equipment is the wrong size, it may not work correctly. For instance, chances are high that a blood pressure reading will be inaccurate if a health care professional uses a blood pressure cuff that’s too small on a patient with obesity, a 2022 paper finds.
To create a comfortable environment for patients with high body weights, the Rudd Center for Food Policy and Obesity recommends that health care facilities provide, among other things, extra-large exam gowns, chairs that can support more than 300 pounds and do not have arms, and wide exam tables that are bolted to the floor so they don’t move.
The consensus statement also recommends improvements to health care facilities.
“Given the prevalence of obesity and obesity-related diseases,” the 36 international experts write, “appropriate infrastructure for the care and management of people with obesity, including severe obesity, must be standard requirement for accreditation of medical facilities and hospitals.”
Source list:
Weight Bias Among Health Care Professionals: A Systematic Review and Meta-Analysis
Blake J. Lawrence; et al. Obesity, November 2021.Joint International Consensus Statement for Ending Stigma of Obesity
Francesco Rubino, et al. Nature Medicine, March 2020.Perceived Weight Discrimination and Chronic Biochemical Stress: A Population-Based Study Using Cortisol in Scalp Hair
Sarah E. Jackson, Clemens Kirschbaum and Andrew Steptoe. Obesity, December 2016.Weight Stigma is Stressful. A Review of Evidence for the Cyclic Obesity/Weight-Based Stigma Model
A. Janet Tomiyama. Appetite, November 2014.Association of Birth by Cesarean Delivery with Obesity and Type 2 Diabetes Among Adult Women
Jorge E. Chavarro. JAMA Network Open, April 2020.Adverse Childhood Experiences and Adult Obesity: A Systematic Review of Plausible Mechanisms and Meta-Analysis of Cross-Sectional Studies
David A. Wiss and Timothy D. Brewerton. Physiology & Behavior, September 2020.Income Inequality and Obesity among U.S. Adults 1999–2016: Does Sex Matter?
Hossein Zare, Danielle D. Gaskin and Roland J. Thorpe Jr. International Journal of Environmental Research and Public Health, July 2021.Comparisons of Explicit Weight Bias Across Common Clinical Specialties of U.S. Resident Physicians
Samantha R. Philip, Sherecce A. Fields, Michelle Van Ryn and Sean M. Phelan. Journal of General Internal Medicine, October 2023.Impact of Weight Bias and Stigma on Quality of Care and Outcomes for Patients with Obesity
S.M. Phelan; et al. Obesity Reviews, April 2015.One Size Does Not Fit All: Impact of Using A Regular Cuff For All Blood Pressure Measurements
Tammy. M. Brady; et al. Circulation, April 2022.This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
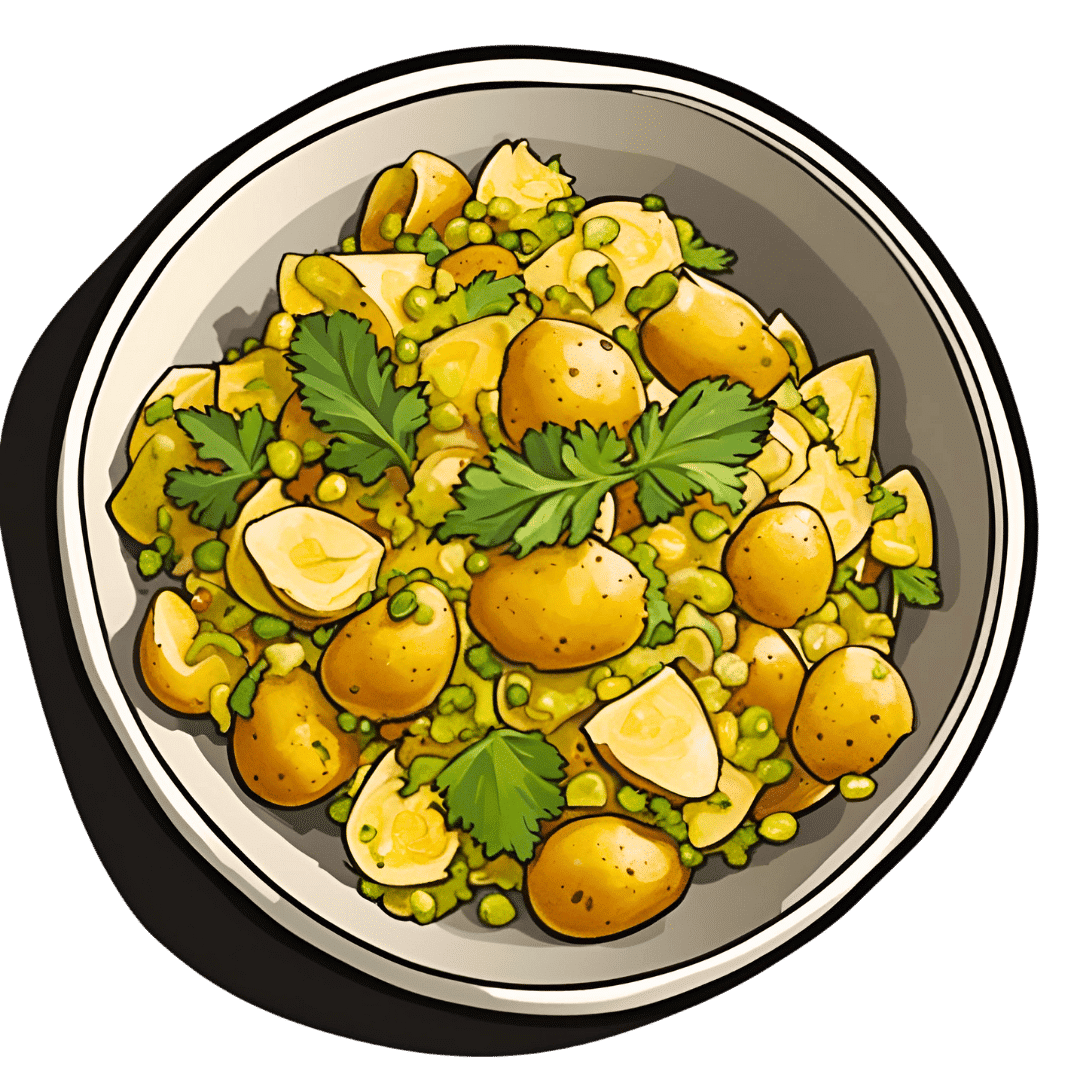
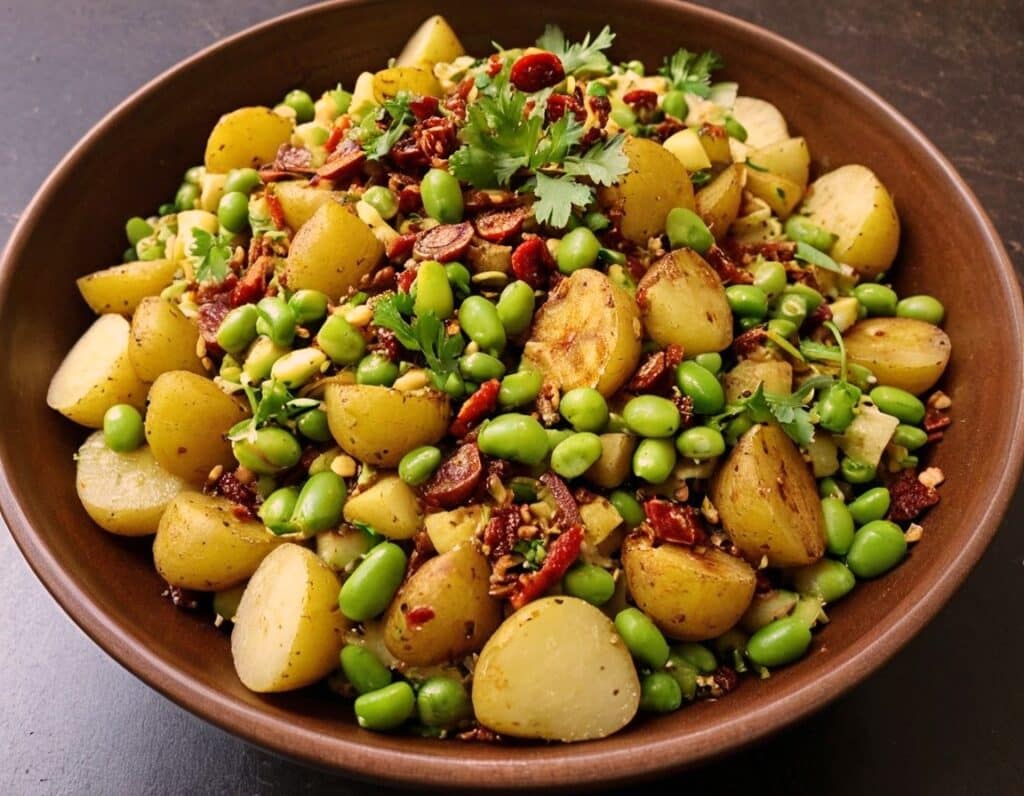
Chaat Masala Spiced Potato Salad With Beans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is an especially gut-healthy dish; the cooked-and-cooled potatoes are not rich with resistant starches (that’s good), the beans bring protein (as well as more fiber and micronutrients), and many of the spices bring their own benefits. A flavorful addition to your table!
You will need
- 1 lb new potatoes, boiled or steamed, with skin on, quartered, cooled ← this is a bit of a “mini recipe”, but we expect you can handle it
- 5 oz blanched broad beans
- 2 oz sun-dried tomatoes, chopped
- ¼ bulb garlic, crushed
- 1 tbsp extra virgin olive oil
- 2 tsp amchoor
- 2 tsp ground cumin
- 2 tsp ground coriander
- 1 tsp ground ginger
- 1 tsp ground asafoetida
- 1 tsp black pepper, coarse ground
- 1 tsp red chili powder
- 1 tsp ground turmeric
- ½ tsp MSG or 1 tsp low-sodium salt
- Juice of ½ lemon
And then…
- To garnish: finely chopped cilantro, or if you have the “cilantro tastes like soap” gene, then substitute with parsley
- To serve: a nice chutney; you can use our Spiced Fruit & Nut Chutney recipe
Method
(we suggest you read everything at least once before doing anything)
1) Mix all the ingredients from the main section, ensuring an even distribution on the spices.
2) Add the garnish, and serve with the chutney. That’s it. There was more work in the prep (and potentially, finding all the ingredients) today.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we scored all five today!
- Lycopene’s Benefits For The Gut, Heart, Brain, & More ← don’t underestimate those sun-dried tomatoes, either!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Holistic Approach To Resculpting A Face Affected By Hypothyroidism, PCOS, Or Menopause
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mila Magnani has PCOS and hypothyroidism, but the principles are the same for menopause because both menopause and PCOS are a case of a hormone imbalance resulting in androgenic effects, so there’s a large amount of overlap.
Obviously, a portion of the difference in the thumbnail is a matter of angle and make-up, but as you can see in the video itself, there’s also a lot of genuine change underneath, too:
Stress-free method
Firstly, she bids us get lab tests and work with a knowledgeable doctor to address potential thyroid, hormonal, or nutrient imbalances. Perhaps we already know at least part of what is causing our problems, but even if so, it doesn’t hurt to take steps to rule the others out. Imagine spending ages unsuccessfully battling PCOS or menopause, only to discover it was a thyroid issue, and you were fighting the wrong battle!
Magnani used a natural route to manage her PCOS and hypothyroidism, while acknowledging that medication is fine too; it’s usually cheaper and more convenient—and there’s a lot more standardization for medications than there is for supplements, which makes it a lot easier to navigate, find what works, and keep getting the exact same thing once it does work.
Other things she recommends include:
- Lymphatic drainage: addressing the lymphatic system to reduce puffiness. Techniques include lymphatic drainage massage, stretching, rebounding (trampoline), and dry brushing. She emphasizes that for facial de-puffing, it’s important to treat the whole upper body, not just the face.
- Low-impact exercise: she switched from high-intensity workouts to low-impact exercises like nature walking and gentle stretching to reduce stress and improve health.
- Nervous system regulation: she worked on nervous system regulation by means of journaling, breathwork, and stimulating the vagus nerve, which improved sleep and reduced stress and anxiety. These things, of course, have knock-on benefits for almost every part of health.
- Diet: she adopted a low-glycemic diet, reduced salt intake, and cooked at home to avoid water retention caused by high sodium in restaurant meals.
- Natural diuretics: she uses teas like hibiscus and chamomile to reduce puffiness after consuming high-sodium foods.
- Sauna and sweating: consider a sauna mat or hot baths to detox and reduce swelling; that’s what she uses in lieu of a convenient sauna.
You may be wondering how quickly you can expect results: it took 3–6 months of daily effort to see significant changes, and she now maintains the routine less frequently (every 2–3 days, instead of daily).
For more on all this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- What Does “Balance Your Hormones” Even Mean?
- 7-Minute Face Fitness For Lymphatic Drainage & Youthful Jawline
- Saunas: Health Benefits (& Caveats)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tinnitus: Quieting The Unwanted Orchestra In Your Ears
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tinnitus—When a “minor” symptom becomes disruptive
Tinnitus (typically: ringing in the ears) is often thought of less as a condition in and of itself, and more a symptom related to other hearing-related conditions. Paradoxically, it can be associated with hearing loss as well as with hyperacusis (hearing supersensitivity, which sounds like a superpower, but can be quite a problem too).
More than just ringing
Tinnitus can manifest not just as ringing, but also as whistling, hissing, pulsing, buzzing, hooting, and more.
For those who don’t suffer from this, it can seem very trivial; for those who do… Sometimes it can seem trivial too!
But sometimes it’s hard to carry on a conversation when at random moments it suddenly sounds like someone is playing a slide-whistle directly into your earhole, or like maybe a fly got stuck in there.
It’s distracting, to say the least.
What causes it?
First let’s note, tinnitus can be acute or chronic. So, some of these things may just cause tinnitus for a while, whereas some may give you tinnitus for life. In some cases, it depends on how long the thing in question persisted for.
A lot of things can cause it, but common causes include:
- Noise exposure (e.g. concerts, some kinds of industrial work, war)
- High blood pressure
- Head/neck injuries
- Ear infection
- Autoimmune diseases (e.g. Type 1 Diabetes, Lupus, Multiple Sclerosis)
So what can be done about it?
Different remedies will work (or not) for different people, depending on the cause and type of tinnitus.
Be warned also: some things that will work for one person’s tinnitus will make another person’s worse, so you might need to try a degree of experimentation and some of it might not be fun!
That in mind, here are some things you might want to try if you haven’t already:
- Earplugs or noise-canceling headphones—while tinnitus is an internal sound, not external, it often has to do with some part(s) of your ears being unduly sensitive, so giving them less stimulus may ease the tinnitus that occurs in reaction to external noise.
- A great option (that this writer uses personally and considers a life-changer) is silicon earplugs that live in a little case on a keyring when not in use—no more heart-racing fleeing from supermarket checkout boops or pedestrian crossing bips or traffic noises or babies crying or (etc)
- White noise—if you also have hyperacusis, a lower frequency range will probably not hurt the way a higher range might. If you don’t also have hyperacusis, you have more options here and this is a popular remedy. Either way, white noise outperforms “relaxing” soundscapes.
- Hearing aids—counterintuitively, for some people whose tinnitus has developed in response to hearing loss, hearing aids can help bring things “back to normal” and eliminate tinnitus in the process.
- Customized sound machines—if you have the resources to get fancy, science currently finds this to be best of all. They work like white noise, but are tailored to your specific tinnitus.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: