A short history of sunscreen, from basting like a chook to preventing skin cancer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australians have used commercial creams, lotions or gels to manage our skin’s sun exposure for nearly a century.
But why we do it, the preparations themselves, and whether they work, has changed over time.
In this short history of sunscreen in Australia, we look at how we’ve slathered, slopped and spritzed our skin for sometimes surprising reasons.
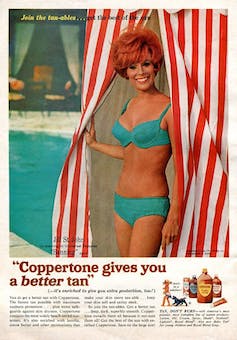
At first, suncreams helped you ‘tan with ease’
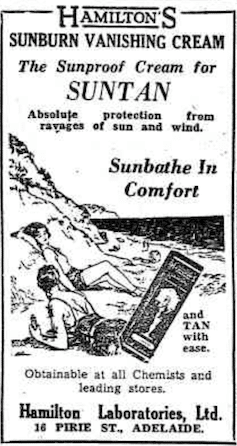
Trove/NLA
Sunscreens have been available in Australia since the 30s. Chemist Milton Blake made one of the first.
He used a kerosene heater to cook batches of “sunburn vanishing cream”, scented with French perfume.
His backyard business became H.A. Milton (Hamilton) Laboratories, which still makes sunscreens today.
Hamilton’s first cream claimed you could “
Sunbathe in Comfort and TAN with ease”. According to modern standards, it would have had an SPF (or sun protection factor) of 2.
The mirage of ‘safe tanning’
A tan was considered a “modern complexion” and for most of the 20th century, you might put something on your skin to help gain one. That’s when “safe tanning” (without burning) was thought possible.
SenseiAlan/Flickr, CC BY-SA
Sunburn was known to be caused by the UVB component of ultraviolet (UV) light. UVA, however, was thought not to be involved in burning; it was just thought to darken the skin pigment melanin. So, medical authorities advised that by using a sunscreen that filtered out UVB, you could “safely tan” without burning.
But that was wrong.
From the 70s, medical research suggested UVA penetrated damagingly deep into the skin, causing ageing effects such as sunspots and wrinkles. And both UVA and UVB could cause skin cancer.
Sunscreens from the 80s sought to be “broad spectrum” – they filtered both UVB and UVA.
Researchers consequently recommended sunscreens for all skin tones, including for preventing sun damage in people with dark skin.
Delaying burning … or encouraging it?
Up to the 80s, sun preparations ranged from something that claimed to delay burning, to preparations that actively encouraged it to get that desirable tan – think, baby oil or coconut oil. Sun-worshippers even raided the kitchen cabinet, slicking olive oil on their skin.
One manufacturer’s “sun lotion” might effectively filter UVB; another’s merely basted you like a roast chicken.
Since labelling laws before the 80s didn’t require manufacturers to list the ingredients, it was often hard for consumers to tell which was which.
At last, SPF arrives to guide consumers
In the 70s, two Queensland researchers, Gordon Groves and Don Robertson, developed tests for sunscreens – sometimes experimenting on students or colleagues. They printed their ranking in the newspaper, which the public could use to choose a product.
An Australian sunscreen manufacturer then asked the federal health department to regulate the industry. The company wanted standard definitions to market their products, backed up by consistent lab testing methods.
In 1986, after years of consultation with manufacturers, researchers and consumers, Australian Standard AS2604 gave a specified a testing method, based on the Queensland researchers’ work. We also had a way of expressing how well sunscreens worked – the sun protection factor or SPF.
This is the ratio of how long it takes a fair-skinned person to burn using the product compared with how long it takes to burn without it. So a cream that protects the skin sufficiently so it takes 40 minutes to burn instead of 20 minutes has an SPF of 2.
Manufacturers liked SPF because businesses that invested in clever chemistry could distinguish themselves in marketing. Consumers liked SPF because it was easy to understand – the higher the number, the better the protection.
Australians, encouraged from 1981 by the Slip! Slop! Slap! nationwide skin cancer campaign, could now “slop” on a sunscreen knowing the degree of protection it offered.
How about skin cancer?
It wasn’t until 1999 that research proved that using sunscreen prevents skin cancer. Again, we have Queensland to thank, specifically the residents of Nambour. They took part in a trial for nearly five years, carried out by a research team led by Adele Green of the Queensland Institute of Medical Research. Using sunscreen daily over that time reduced rates of squamous cell carcinoma (a common form of skin cancer) by about 60%.
Follow-up studies in 2011 and 2013 showed regular sunscreen use almost halved the rate of melanoma and slowed skin ageing. But there was no impact on rates of basal cell carcinoma, another common skin cancer.
By then, researchers had shown sunscreen stopped sunburn, and stopping sunburn would prevent at least some types of skin cancer.
What’s in sunscreen today?
An effective sunscreen uses one or more active ingredients in a cream, lotion or gel. The active ingredient either works:
-
“chemically” by absorbing UV and converting it to heat. Examples include PABA (para-aminobenzoic acid) and benzyl salicylate, or
-
“physically” by blocking the UV, such as zinc oxide or titanium dioxide.
Physical blockers at first had limited cosmetic appeal because they were opaque pastes. (Think cricketers with zinc smeared on their noses.)
With microfine particle technology from the 90s, sunscreen manufacturers could then use a combination of chemical absorbers and physical blockers to achieve high degrees of sun protection in a cosmetically acceptable formulation.
Where now?
Australians have embraced sunscreen, but they still don’t apply enough or reapply often enough.
Although some people are concerned sunscreen will block the skin’s ability to make vitamin D this is unlikely. That’s because even SPF50 sunscreen doesn’t filter out all UVB.
There’s also concern about the active ingredients in sunscreen getting into the environment and whether their absorption by our bodies is a problem.
Sunscreens have evolved from something that at best offered mild protection to effective, easy-to-use products that stave off the harmful effects of UV. They’ve evolved from something only people with fair skin used to a product for anyone.
Remember, slopping on sunscreen is just one part of sun protection. Don’t forget to also slip (protective clothing), slap (hat), seek (shade) and slide (sunglasses).
Laura Dawes, Research Fellow in Medico-Legal History, Australian National University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
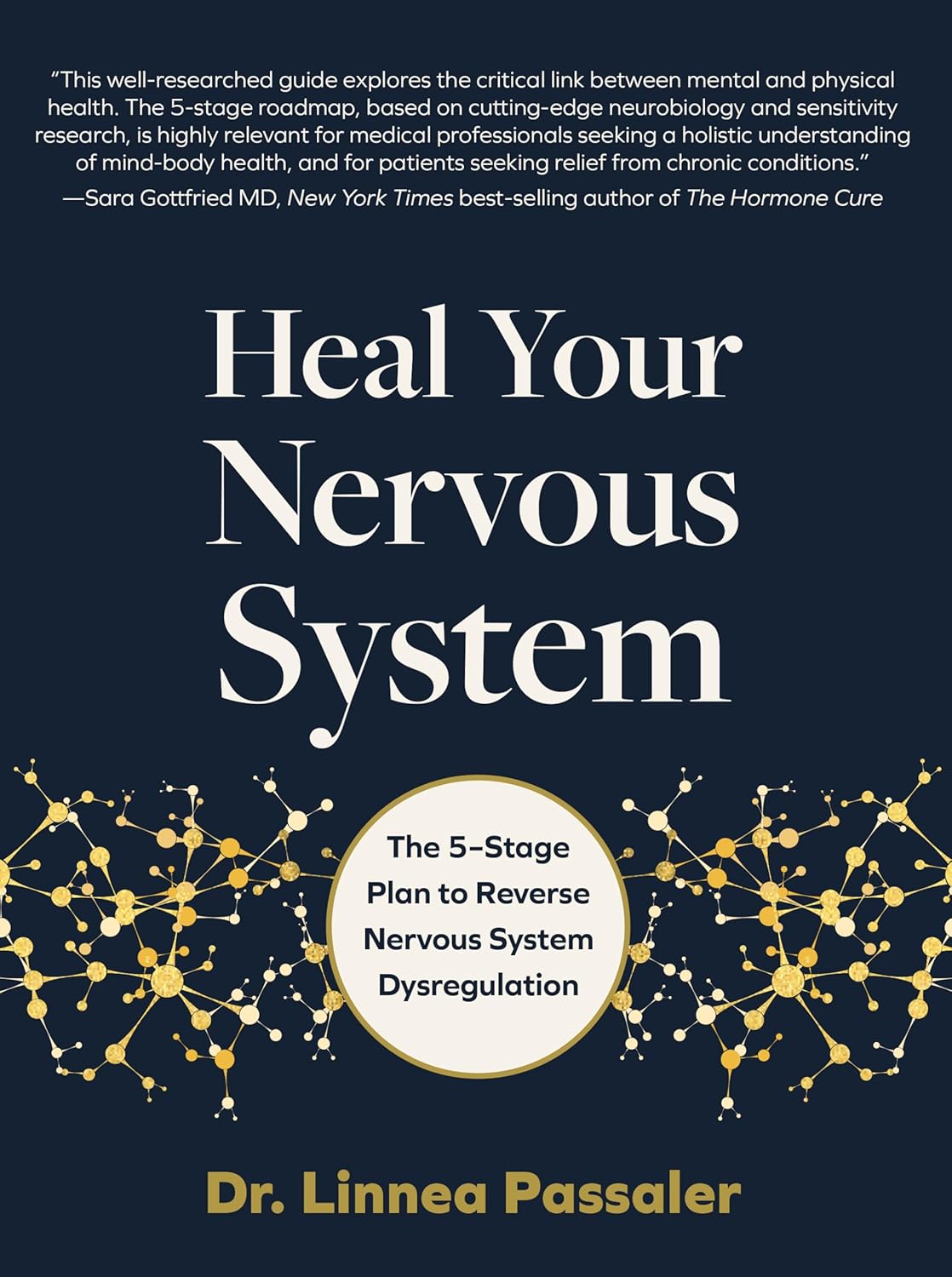
Heal Your Nervous System – by Dr. Linnea Passaler
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book focuses on the oft-overlooked connection between nervous system dysregulation (i.e. sympathetic nervous system dominance, keeping the brain in “may have to fight for my life at any moment” mode) and the many symptoms—mental and physical—that can arise as a result.
While there is a lot of theory explained in here, there’s practicality too, providing the reader with tools to assess our own levels of nervous system dysregulation and what factors affect that.
In particular in that category, a lot of value is delivered in terms of practical guidance on avoiding common pitfalls in the healing journey. Dr. Passaler discusses the four biggest mistakes people make when attempting to heal, and gives clear strategies to sidestep each of them, with exercises to do and habits to implement.
Another thing that sets this book apart from many of its genre is her emphasis on the importance of sequencing healing practices in the right order. By offering a structured approach, the book helps us implement healing practices without getting overwhelmed or hitting the proverbial brick wall and getting frustrated, which makes a big difference.
The style is easy-to-understand pop-science, albeit with a reassuring 20 pages of references at the back.
Bottom line: if you feel like “peace of mind” is something that’s always just out of reach, this book can help you to get where you need to be, physically as well as mentally.
Click here to check out Heal Your Nervous System, and get things into much better order!
Share This Post
-
Visceral Belly Fat & How To Lose It
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Visceral Belly Fat & How To Lose It
We’ve talked before about how waist circumference is a much more useful indicator of metabolic health than BMI.
So, let’s say you’ve a bit more around the middle than you’d like, but it stubbornly stays there. What’s going on underneath what you can see, why is it going on, and how can you get it to change?
What is visceral fat?
First, let’s talk about subcutaneous fat. That’s the fat directly under your skin. Women usually have more than men, and that’s perfectly healthy (up to a point); it’s supposed to be that way. We (women) will tend to accumulate this mostly in places such as our breasts, hips, and butt, and work outwards from there. Men will tend to put it on more to the belly and face.
Side-note: if you’re undergoing (untreated) menopause, the changes in your hormone levels will tend to result in more subcutaneous fat to the belly and face too. That’s normal, and/but normal is not always good, and treatment options are great (with hormone replacement therapy, HRT, topping the list).
Visceral fat (also called visceral adipose tissue), on the other hand, is the fat of the viscera—the internal organs of the abdomen.
So, this is fat that goes under your abdominal muscles—you can’t squeeze this (directly).
So what can we do?
Famously “you can’t do spot reduction” (lose fat from a particular part of your body by focusing exercises on that area), but that’s about subcutaneous fat. There are things you can do that will reduce your visceral fat in particular.
Some of these advices you may think “that’s just good advice for losing fat in general” and it is, yes. But these are things that have the biggest impact on visceral fat.
Cut alcohol use
This is the biggie. By numerous mechanisms, some of which we’ve talked about before, alcohol causes weight gain in general yes, but especially for visceral fat.
Get better sleep
You might think that hitting the gym is most important, but this one ranks higher. Yes, you can trim visceral fat without leaving your bed (and even without getting athletic in bed, for that matter). Not convinced?
- Here’s a study of 101 people looking at sleep quality and abdominal adiposity
- Oh, and here’s a meta-analysis with 56,000 people (finding the same thing), in case that one study didn’t convince you.
So, the verdict is clear: you snooze, you lose (visceral fat)!
Tweak your diet
You don’t have to do a complete overhaul (unless you want to), but a few changes can make a big difference, especially:
- Getting more fiber (this is the biggie when it comes to diet)
- Eating less sugar (not really a surprise, but relevant to mention)
- Eat whole foods (skip the highly processed stuff)
If you’d like to learn more and enjoy videos, here’s an informative one to get you going!
Click Here If The Embedded Video Doesn’t Load Automatically! Share This Post
-
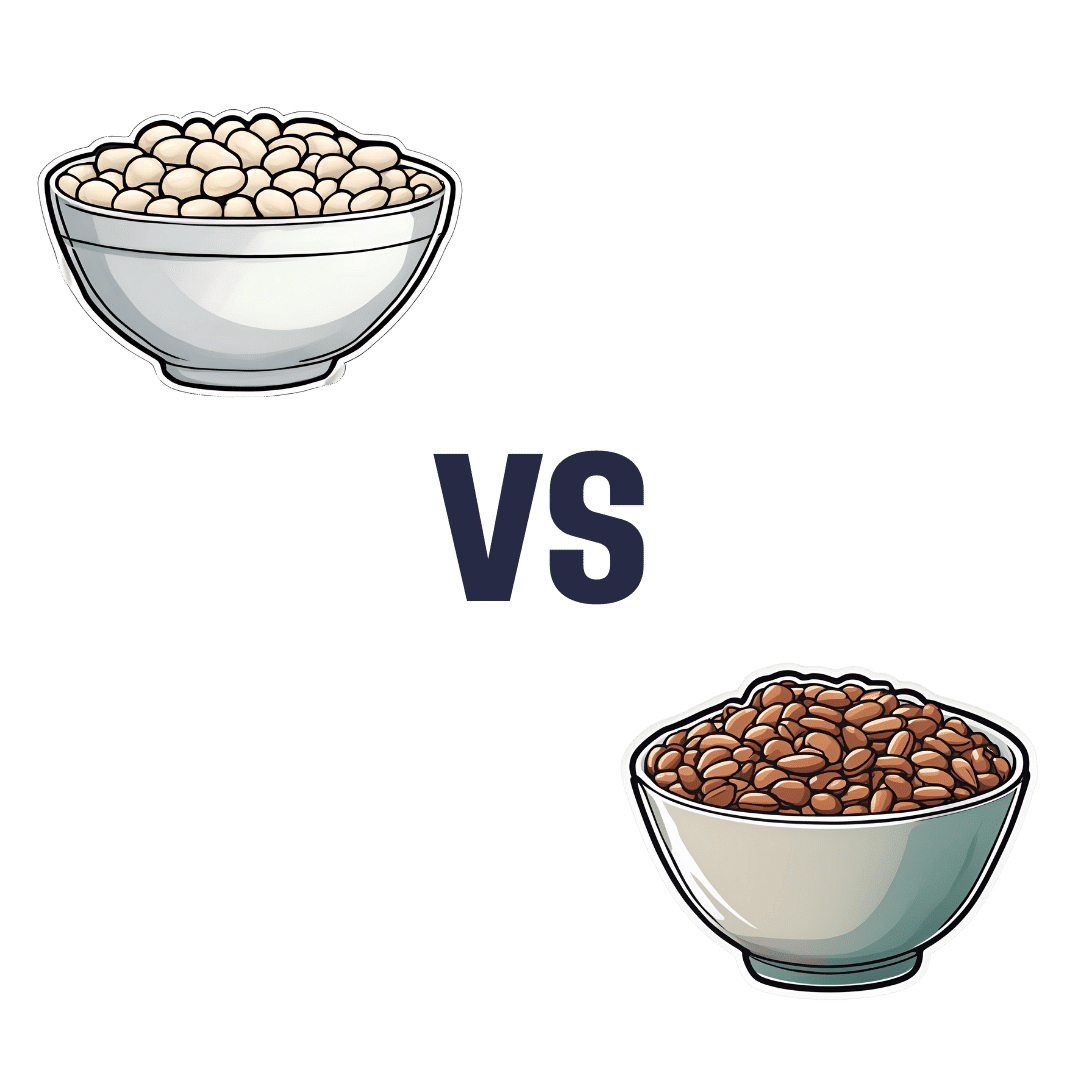
White Beans vs Pinto Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing white beans to pinto beans, we picked the pinto beans.
Why?
Both are good and both have their strengths! But we say the pinto beans come out on top in total:
In terms of macros, the two beans are about equal in protein and carbs, while pinto beans have notably more fiber. White beans were already good, but we say having 1.5x the fiber makes pinto beans the winner in this category.
In the category of vitamins, white beans are not higher in any vitamins, while pinto beans have more of vitamins B1, B2, B3, B6, B7, B9, and C, making for a 7:0 win for pinto beans. It’s worth mentioning that both beans are equal in vitamins B5, E, K, and choline, though. Still, pinto beans win easily on the strength of those 7 vitamins they have more of.
When it comes to minerals, white beans have more calcium, copper, iron, magnesium, manganese, potassium, and zinc, while pinto beans have more phosphorus and selenium, making for a win for white beans this time.
Adding up the sections makes for an overall win for pinto beans, but by all means, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Share This Post
Related Posts
-
Terminal lucidity: why do loved ones with dementia sometimes ‘come back’ before death?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dementia is often described as “the long goodbye”. Although the person is still alive, dementia slowly and irreversibly chips away at their memories and the qualities that make someone “them”.
Dementia eventually takes away the person’s ability to communicate, eat and drink on their own, understand where they are, and recognise family members.
Since as early as the 19th century, stories from loved ones, caregivers and health-care workers have described some people with dementia suddenly becoming lucid. They have described the person engaging in meaningful conversation, sharing memories that were assumed to have been lost, making jokes, and even requesting meals.
It is estimated 43% of people who experience this brief lucidity die within 24 hours, and 84% within a week.
Why does this happen?
Terminal lucidity or paradoxical lucidity?
In 2009, researchers Michael Nahm and Bruce Greyson coined the term “terminal lucidity”, since these lucid episodes often occurred shortly before death.
But not all lucid episodes indicate death is imminent. One study found many people with advanced dementia will show brief glimmers of their old selves more than six months before death.
Lucidity has also been reported in other conditions that affect the brain or thinking skills, such as meningitis, schizophrenia, and in people with brain tumours or who have sustained a brain injury.
Moments of lucidity that do not necessarily indicate death are sometimes called paradoxical lucidity. It is considered paradoxical as it defies the expected course of neurodegenerative diseases such as dementia.
But it’s important to note these episodes of lucidity are temporary and sadly do not represent a reversal of neurodegenerative disease.
Sadly, these episodes of lucidity are only temporary. Pexels/Kampus Production Why does terminal lucidity happen?
Scientists have struggled to explain why terminal lucidity happens. Some episodes of lucidity have been reported to occur in the presence of loved ones. Others have reported that music can sometimes improve lucidity. But many episodes of lucidity do not have a distinct trigger.
A research team from New York University speculated that changes in brain activity before death may cause terminal lucidity. But this doesn’t fully explain why people suddenly recover abilities that were assumed to be lost.
Paradoxical and terminal lucidity are also very difficult to study. Not everyone with advanced dementia will experience episodes of lucidity before death. Lucid episodes are also unpredictable and typically occur without a particular trigger.
And as terminal lucidity can be a joyous time for those who witness the episode, it would be unethical for scientists to use that time to conduct their research. At the time of death, it’s also difficult for scientists to interview caregivers about any lucid moments that may have occurred.
Explanations for terminal lucidity extend beyond science. These moments of mental clarity may be a way for the dying person to say final goodbyes, gain closure before death, and reconnect with family and friends. Some believe episodes of terminal lucidity are representative of the person connecting with an afterlife.
Why is it important to know about terminal lucidity?
People can have a variety of reactions to seeing terminal lucidity in a person with advanced dementia. While some will experience it as being peaceful and bittersweet, others may find it deeply confusing and upsetting. There may also be an urge to modify care plans and request lifesaving measures for the dying person.
Being aware of terminal lucidity can help loved ones understand it is part of the dying process, acknowledge the person with dementia will not recover, and allow them to make the most of the time they have with the lucid person.
For those who witness it, terminal lucidity can be a final, precious opportunity to reconnect with the person that existed before dementia took hold and the “long goodbye” began.
Yen Ying Lim, Associate Professor, Turner Institute for Brain and Mental Health, Monash University and Diny Thomson, PhD (Clinical Neuropsychology) Candidate and Provisional Psychologist, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
8 Signs Of Iodine Deficiency You Might Not Expect
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health Coach Kait (BSc Nutrition & Exercise) is a certified health and nutrition coach, and today she’s here to talk about iodine—which is important for many of our body functions, from thyroid hormone production to metabolic regulation to heart rate management, as well as more superficial-but-important-too things like our skin and hair.
Kait’s hitlist
Here’s what she recommends we look out for:
- Swollen neck: even a slightly swollen neck might indicate low iodine levels (this is because that’s where the thyroid glands are)
- Hair loss: iodine is needed for healthy hair growth, so a deficiency can lead to hair loss / thinning hair
- Dry and flaky skin: with iodine’s role in our homeostatic system not being covered, our skin can dry out as a result
- Feeling cold all the time: because of iodine’s temperature-regulating activities
- Slow heart rate: A metabolic slump due to iodine deficiency can slow down the heart rate, leading to fatigue and weakness (and worse, if it persists)
- Brain fog: trouble focusing can be a symptom of the same metabolic slump
- Fatigue: this is again more or less the same thing, but she said eight signs, so we’re giving you the eight!
- Irregular period (if you normally have such, of course): because iodine affects reproductive hormones too, an imbalance can disrupt menstrual cycles.
For more on each of these, as well as how to get more iodine in your diet, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
You might also like to read:
- A Fresh Take On Hypothyroidism
- Foods For Managing Hypothyroidism (incl. Hashimoto’s)
- Eat To Beat Hyperthyroidism!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Never Too Late To Start Over: Finding Purpose At Any Age
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dana Findwell’s late 50s were not an easy time, but upon now hitting 60 (this week, at time of writing), she’s enthusiastically throwing herself into the things that bring her purpose, and so can you.
Start where you are
Findwell was already no stranger to starting again, having been married and divorced twice, and having moved frequently, requiring constant “life resets”.
Nevertheless, she always had her work to fall back on; she was a graphic designer and art director for 30 years… Until burnout struck.
And when burnout struck, so did COVID, resulting in the loss of her job. Her job wasn’t the only thing she lost though, as her mother died around the same time. All in all, it was a lot, and not the fun kind of “a lot”.
Struggling to find a new career direction, she ended up starting a small business for herself, so that she could direct the pace; pressing forwards as and when she had the energy. This became her new “ikigai“, the main thing that brings a sense of purpose to her life, but getting one part of her life back into order brought her attention to the rest; she realized she’d neglected her health, so she joined a gym. And a weightlifting class. And a hip-hop class. And she took up the practice of Japanese drumming (for the unfamiliar, this can be a rather athletic ability; it’s not a matter of sitting at a drum kit).
And now? Her future is still not clear, but that’s ok, because she’s making it as she goes, and she’s doing it her way, trusting in her ability to handle what may come up, and doing the things now that future-her will be glad of having done (e.g. laying the groundwork of both financial security and good health).
Change can sometimes be triggered by adverse circumstances, but there’s always the opportunity to find something better. For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: