Can We Drink To Good Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can we drink to good health?
We asked you for your thoughts on alcohol and heart health, and we got quite an even spread of results!
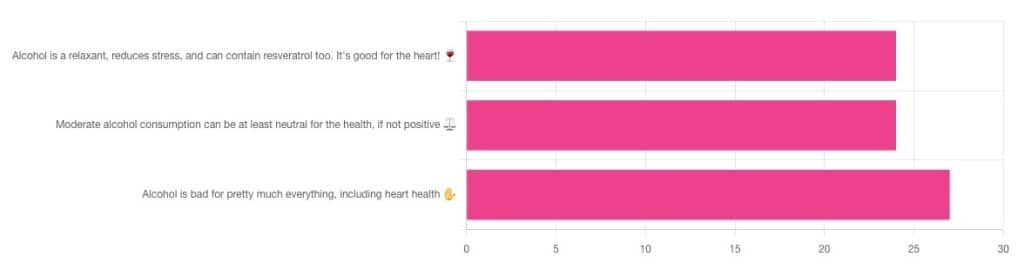
If perchance that’s too tiny to read, the figures were:
- 32% voted for “Alcohol is a relaxant, reduces stress, and can contain resveratrol too. It’s good for the heart!”
- 32% voted for: “Moderate alcohol consumption can be at least neutral for the health, if not positive ⚖️”
- 36% voted for: “Alcohol is bad for pretty much everything, including heart health ✋”
One subscriber who voted for “Alcohol is a relaxant, reduces stress, and can contain resveratrol too. It’s good for the heart!” added the following thoughts:
❝While it isn’t necessary to consume alcohol, moderate amounts can be beneficial and contribute to well-being through social activity, celebrations, etc.❞
That’s an interesting point, and definitely many people do see alcohol that way! Of course, that does not mean that one will find no social activities, celebrations, etc, in parts of the world where alcohol consumption is uncommon. Indeed, in India, wedding parties where no alcohol is consumed can go on for days!
But, “we live in a society” and all that, and while we’re a health newsletter not a social issues newsletter, it’d be remiss of us to not acknowledge the importance of socialization for good mental health—and thus the rest of our health too.
So, if indeed all our friends and family drink alcohol, it can certainly make abstaining more of a challenge.
On that note, let’s take a moment to consider “The French Paradox” (an observation of a low prevalence of ischemic heart disease despite high intakes of saturated fat, a phenomenon accredited to the consumption of red wine).
As it happens, a comprehensive review in “Circulation”, a cardiovascular health journal, has suggested the French Paradox may not be so paradoxical after all.
Research suggests it has more to do with other lifestyle factors (and historic under-reporting of cardiovascular disease by French doctors), which would explain why Japan has lower rates of heart disease, despite drinking little wine, and more beer and spirits.
So, our subscriber’s note may not be completely without reason! It’s just about the party, not the alcohol.
One subscriber who voted for “Moderate alcohol consumption can be at least neutral for the health, if not positive ⚖️” wrote:
❝Keeping in mind, moderate means one glass of wine for women a day and two for men. Hard alcohol doesn’t have the same heart benefits as wine❞
That is indeed the guideline according to some health bodies!
In other places with different guiding advisory bodies, that’s been dropped down to one a day for everyone (the science may be universal, but how government institutions interpret that is not).
About that wine… Specifically, red wine, for its resveratrol content:
While there are polyphenols such as resveratrol in red wine that could boost heart health, there’s so little per glass that you may need 100–1000 glasses to get the dosage that provides benefits in mouse studies. If you’re not a mouse, you might even need more.
To this end, many people prefer resveratrol supplementation. ← link is to an example product, but there are plenty more so feel free to shop around
A subscriber who voted for “Alcohol is bad for pretty much everything, including heart health ✋” says:
❝New guidelines suggest 1 to 2 drinks a week are okay but the less the better.❞
If you haven’t heard these new guidelines, we’ll mention again: every government has its own official bodies and guidelines so perhaps your local guidelines differ, but for example here’s what that World Health Organization has to say (as of January this year):
WHO: No level of alcohol consumption is safe for our health
So, whom to believe? The governments who hopefully consider the welfare of their citizenry more important than the tax dollars from alcohol sales, or the World Health Organization?
It’s a tough one, but we’ll always err on the side of the science.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Synergistic Brain-Training
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let The Games Begin (But It Matters What Kind)
Exercise is good for brain health; we’ve written about this before, for example:
How To Reduce Your Alzheimer’s Risk ← there are many advices here, but exercise, especially cardiovascular exercise in this case, is an important item on the list!
Today it’s Psychology Sunday though, and we’re going to talk about looking after brain health by means of brain-training, via games.
“Brain-training” gets a lot of hype and flak:
- Hype: do sudoku every day and soon you will have an IQ of 200 and still have a sharp wit at the age of 120
- Flak: brain-training is usually training only one kind of cognitive function, with limited transferability to the rest of life
The reality is somewhere between the two. Brain training really does improve not just outwardly measurable cognitive function, but also internally measurable improvements visible on brain scans, for example:
- Cognitive training modified age-related brain changes in older adults with subjective memory decline
- Functional brain changes associated with cognitive training in healthy older adults: A preliminary ALE meta-analysis
But what about the transferability?
Let us play
This is where game-based brain-training comes in. And, the more complex the game, the better the benefits, because there is more chance of applicability to life, e.g:
- Sudoku: very limited applicability
- Crosswords: language faculties
- Chess: spatial reasoning, critical path analysis, planning, memory, focus (also unlike the previous two, chess tends to be social for most people, and also involve a lot of reading, if one is keen)
- Computer games: wildly varied depending on the game. While an arcade-style “shoot-em-up” may do little for the brain, there is a lot of potential for a lot of much more relevant brain-training in other kinds of games: it could be planning, problem-solving, social dynamics, economics, things that mirror the day-to-day challenges of running a household, even, or a business.
- It’s not that the skills are useful, by the way. Playing “Stardew Valley” will not qualify you to run a real farm, nor will playing “Civilization” qualify you to run a country. But the brain functions used and trained? Those are important.
It becomes easily explicable, then, why these two research reviews with very similar titles got very different results:
- A Game a Day Keeps Cognitive Decline Away? A Systematic Review and Meta-Analysis of Commercially-Available Brain Training Programs in Healthy and Cognitively Impaired Older Adults
- Game-based brain training for improving cognitive function in community-dwelling older adults: A systematic review and meta-regression
The first review found that game-based brain-training had negligible actual use. The “games” they looked at? BrainGymmer, BrainHQ, CogMed, CogniFit, Dakim, Lumosity, and MyBrainTrainer. In other words, made-for-purpose brain-trainers, not actual computer games per se.
The second reviewfound that game-based training was very beneficial. The games they looked at? They didn’t name them, but based on the descriptions, they were actual multiplayer online turn-based computer games, not made-for-purpose brain-trainers.
To summarize the above in few words: multiplayer online turn-based computer games outperform made-for-purpose brain-trainers for cognitive improvement.
Bringing synergy
However, before you order that expensive gaming-chair for marathon gaming sessions (research suggests a tail-off in usefulness after about an hour of continuous gaming per session, by the way), be aware that cognitive training and (physical) exercise training combined, performed close in time to each other or simultaneously, perform better than the sum of either alone:
See also:
❝Simultaneous training was the most efficacious approach for cognition, followed by sequential combinations and cognitive training alone, and significantly better than physical exercise.
Our findings suggest that simultaneously and sequentially combined interventions are efficacious for promoting cognitive alongside physical health in older adults, and therefore should be preferred over implementation of single-domain training❞
~ Dr. Hanna Malmberg Gavelin et al.
Take care!
Share This Post
-
Bell Pepper vs Sweetcorn – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing bell pepper to sweetcorn, we picked the corn.
Why?
If you’re thinking “but wait, which color bell pepper, don’t they have different nutritional properties?” then firstly, well-remembered, and secondly, it doesn’t matter in this case. The main things that it affects are vitamins A and C and various polyphenols, and even the weakest bell pepper for them wins on both of those vitamins (while the strongest bell peppers for them still lose on vitamins in total) and even the strongest bell pepper for them loses on polyphenols, so the results go the same with any color.
In terms of macros, the corn has more carbs, protein, and fiber; however, both are low in glycemic index, so we’ll go with the “more food per food” option, the corn.
In the category of vitamins, even green bell peppers (the least well-endowed) have more of vitamins A, B6, C, E, and K, while sweetcorn has more of vitamins B1, B2, B3, B5, B9, and choline, compared to even yellow or red bell peppers (which are the best peppers for vitamins). So, a moderate win for the corn.
When it comes to minerals, bell peppers have more calcium and copper, while sweetcorn has more iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. An easy win for sweetcorn.
In short, enjoy both, but the corn is the overall winner today!
Want to learn more?
You might like to read:
- Brain Food? The Eyes Have It! ← green bell peppers are a good source of lutein, as is sweetcorn
- A Spectrum Of Specialties: Which Bell Peppers To Pick?
Take care!
Share This Post
-
How To Be 7.5x More Likely To Develop Chronic Fatigue Syndrome
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what is it?
Many more people have chronic fatigue, which is the symptom of being exhausted all the time, than have chronic fatigue syndrome (CFS) which is the illness of myalgic encephalomyelitis (ME).
This is because fatigue can be a symptom of many, many other conditions, and can be heavily influenced by lifestyle factors too.
A lot of the advice for dealing with chronic fatigue is often the same in both cases, but some will be different, because for example:
- If your fatigue is from some other condition, that condition probably impacts what lifestyle factors you are (and are not) able to change, too
- If your fatigue is from lifestyle factors, that hopefully means you can change those and enjoy less fatigue…
- But if it’s not from lifestyle factors, as in ME/CFS, then advice to “exercise more” etc is not going to help so much.
There are ways to know the difference though:
Check out: Do You Have Chronic Fatigue Syndrome?
The chronic disease pipeline
While it had been strongly suspected that COVID infection could lead to CFS, with long COVID having chronic fatigue as one of its characteristic symptoms, a research team led by Dr. Suzanne Vernon has now established the nature of the relationship.
It was a large (n=13,224) longitudinal observational cohort study of people with no pre-existing ME/CFS, grouped according to their COVID infection status:
- acute infected, enrolled within 30 days of infection or enrolled as uninfected who became infected (n=4,515)
- post-acute infected, enrolled greater than 30 days after infection (n=7,270)
- uninfected (n=1,439).
(to be clear, that last means “never infected”, or else they would be in group 2)
Note: people who had COVID and were hospitalized for it were excluded from the study, so this risk is the risk represented by even just more “moderate” infections.
What they found:
❝The proportion of all RECOVER-Adult participants that met criteria for ME/CFS following SARS-CoV-2 infection was 4.5% (531 of 11,785) compared to 0.6% (9 of 1439) in uninfected participants.❞
There are then different numbers if we look per 100 person-years, as the study also did—in which case, we get a re-modelled increase in risk of 5x instead of 7.5x, but a) that’s still not good b) the “here-and-now” figures of 4.5% vs 0.6% are also relevant.
Read in full: Incidence and Prevalence of Post-COVID-19 Myalgic Encephalomyelitis: A Report from the Observational RECOVER-Adult Study
The killer nobody wants to talk about anymore
Of course, as we all know the pandemic is over, because politicians declared it so, which is very reassuring.
Nevertheless, COVID is currently the still 4th leading cause of death in the US, placing it higher than stroke, Alzheimer’s, diabetes, and others.
See also: Emergency or Not, Covid Is Still Killing People. Here’s What Doctors Advise to Stay Safe
So, while it’s very good to take care of our hearts, brains, blood sugars, and so forth, let’s at the very least continue to keep on top of our vaccinations, avoid enclosed crowded spaces where possible, etc.
And for extra boosts to one’s chances: Why Some People Get Sick More (And How To Not Be One Of Them)
What if I do get (or already have) long COVID and/or ME/CFS?
Well, that is definitely going to suck, but there are still some things that can be done.
Here’s a big one: How To Eat To Beat Chronic Fatigue ← this will not, of course, cure you, but it’s a way of getting maximum nutrition for minimum effort, given that for someone with chronic fatigue, effort is a very finite resource that must be used sparingly
Finally, here are some further resources:
Support For Long COVID & Chronic Fatigue
Take care!
Share This Post
Related Posts
-
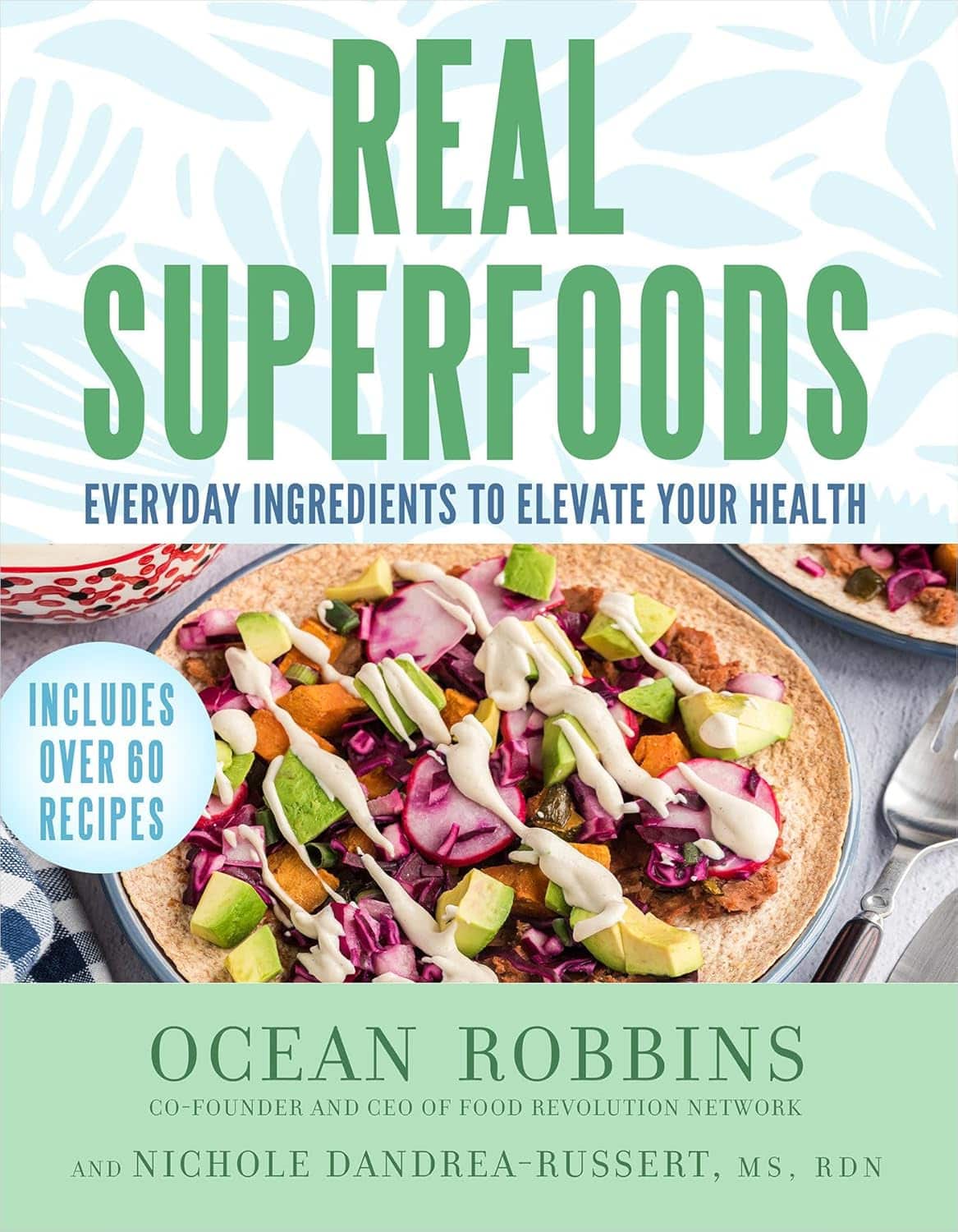
Real Superfoods – by Ocean Robbins & Nichole Dandrea-Russert
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Of the two authors, the former is a professional public speaker, and the latter is a professional dietician. As a result, we get a book that is polished and well-presented, while actually having a core of good solid science (backed up with plenty of references).
The book is divided into two parts; the first part has 9 chapters pertaining to 9 categories of superfood (with more details about top-tier examples of each, within), and the second part has 143 pages of recipes.
And yes, as usual, a couple of the recipes are “granola” and “smoothie”, but when are they not? Most of the recipes are worthwhile, though, with a lot of good dishes that should please most people.
Bottom line: this is half pop-science presentation of superfoods, and half cookbook featuring those ingredients. Definitely a good way to increase your consumption of superfoods, and get the most out of your diet.
Click here to check out Real Superfoods, and power up your health!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A new emergency procedure for cardiac arrests aims to save more lives – here’s how it works
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As of January this year, Aotearoa New Zealand became just the second country (after Canada) to adopt a groundbreaking new procedure for patients experiencing cardiac arrest.
Known as “double sequential external defibrillation” (DSED), it will change initial emergency response strategies and potentially improve survival rates for some patients.
Surviving cardiac arrest hinges crucially on effective resuscitation. When the heart is working normally, electrical pulses travel through its muscular walls creating regular, co-ordinated contractions.
But if normal electrical rhythms are disrupted, heartbeats can become unco-ordinated and ineffective, or cease entirely, leading to cardiac arrest.
Defibrillation is a cornerstone resuscitation method. It gives the heart a powerful electric shock to terminate the abnormal electrical activity. This allows the heart to re-establish its regular rhythm.
Its success hinges on the underlying dysfunctional heart rhythm and the proper positioning of the defibrillation pads that deliver the shock. The new procedure will provide a second option when standard positioning is not effective.
Using two defibrillators
During standard defibrillation, one pad is placed on the right side of the chest just below the collarbone. A second pad is placed below the left armpit. Shocks are given every two minutes.
Early defibrillation can dramatically improve the likelihood of surviving a cardiac arrest. However, around 20% of patients whose cardiac arrest is caused by “ventricular fibrillation” or “pulseless ventricular tachycardia” do not respond to the standard defibrillation approach. Both conditions are characterised by abnormal activity in the heart ventricles.
DSED is a novel method that provides rapid sequential shocks to the heart using two defibrillators. The pads are attached in two different locations: one on the front and side of the chest, the other on the front and back.
A single operator activates the defibrillators in sequence, with one hand moving from the first to the second. According to a recent randomised trial in Canada, this approach could more than double the chances of survival for patients with ventricular fibrillation or pulseless ventricular tachycardia who are not responding to standard shocks.
The second shock is thought to improve the chances of eliminating persistent abnormal electrical activity. It delivers more total energy to the heart, travelling along a different pathway closer to the heart’s left ventricle.
Evidence of success
New Zealand ambulance data from 2020 to 2023 identified about 1,390 people who could potentially benefit from novel defibrillation methods. This group has a current survival rate of only 14%.
Recognising the potential for DSED to dramatically improve survival for these patients, the National Ambulance Sector Clinical Working Group updated the clinical procedures and guidelines for emergency medical services personnel.
The guidelines now specify that if ventricular fibrillation or pulseless ventricular tachycardia persist after two shocks with standard defibrillation, the DSED method should be administered. Two defibrillators need to be available, and staff must be trained in the new approach.
Though the existing evidence for DSED is compelling, until recently it was based on theory and a small number of potentially biased observational studies. The Canadian trial was the first to directly compare DSED to standard treatment.
From a total of 261 patients, 30.4% treated with this strategy survived, compared to 13.3% when standard resuscitation protocols were followed.
The design of the trial minimised the risk of other factors confounding results. It provides confidence that survival improvements were due to the defibrillation approach and not regional differences in resources and training.
The study also corroborates and builds on existing theoretical and clinical scientific evidence. As the trial was stopped early due to the COVID-19 pandemic, however, the researchers could recruit fewer than half of the numbers planned for the study.
Despite these and other limitations, the international group of experts that advises on best practice for resuscitation updated its recommendations in 2023 in response to the trial results. It suggested (with caution) that emergency medical services consider DSED for patients with ventricular fibrillation or pulseless ventricular tachycardia who are not responding to standard treatment.
Training and implementation
Although the evidence is still emerging, implementation of DSED by emergency services in New Zealand has implications beyond the care of patients nationally. It is also a key step in advancing knowledge about optimal resuscitation strategies globally.
There are always concerns when translating an intervention from a controlled research environment to the relative disorder of the real world. But the balance of evidence was carefully considered before making the decision to change procedures for a group of patients who have a low likelihood of survival with current treatment.
Before using DSED, emergency medical personnel undergo mandatory education, simulation and training. Implementation is closely monitored to determine its impact.
Hospitals and emergency departments have been informed of the protocol changes and been given opportunities to ask questions and give feedback. As part of the implementation, the St John ambulance service will perform case reviews in addition to wider monitoring to ensure patient safety is prioritised.
Ultimately, those involved are optimistic this change to cardiac arrest management in New Zealand will have a positive impact on survival for affected patients.
Vinuli Withanarachchie, PhD candidate, College of Health, Massey University; Bridget Dicker, Associate Professor of Paramedicine, Auckland University of Technology, and Sarah Maessen, Research Associate, Auckland University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Do We Need Sunscreen In Winter, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I keep seeing advice that we shoudl wear sunscreen out in winter even if it’s not hot or sunny, but is there actually any real benefit to this?❞
Short answer: yes (but it’s indeed not as critical as it is during summer’s hot/sunny days)
Longer answer: first, let’s examine the physics of summer vs winter when it comes to the sun…
In summer (assuming we live far enough from the equator to have this kind of seasonal variation), the part of the planet where we live is tilted more towards the sun. This makes it closer, and more importantly, it’s more directly overhead during the day. The difference in distance through space isn’t as big a deal as the difference in distance through the atmosphere. When the sun is more directly overhead, its rays have a shorter path through our atmosphere, and thus less chance of being blocked by cloud cover / refracted elsewhere / bounced back off into space before it even gets that far.
In winter, the opposite of all that is true.
Morning/evening also somewhat replicate this compared to midday, because the sun being lower in the sky has a similar effect to seasonal variation causing it to be less directly overhead.
For this reason, even though visually the sun may be just as bright on a winter morning as it is on a summer midday, the rays have been filtered very differently by the time they get to us.
This is one reason why you’re much less likely to get sunburned in the winter, compared to the summer (others include the actual temperature difference, your likely better hydration, and your likely more modest attire protecting you).
However…
The reason it is advisable to wear sunscreen in winter is not generally about sunburn, and is rather more about long-term cumulative skin damage (ranging from accelerated aging to cancer) caused by the UV rays—specifically, mostly UVA rays, since UVB rays (with their higher energy but shorter wavelength) have nearly all been blocked by the atmosphere.
Here’s a good explainer of that from the American Cancer Society:
UV (Ultraviolet) Radiation and Cancer Risk
👆 this may seem like a no-brainer, but there’s a lot explained here that demystifies a lot of things, covering ionizing vs non-ionizing radiation, x-rays and gamma-rays, the very different kinds of cancer caused by different things, and what things are dangerous vs which there’s no need to worry about (so far as best current science can say, at least).
Consequently: yes, if you value your skin health and avoidance of cancer, wearing sunscreen when out even in the winter is a good idea. Especially if your phone’s weather app says the UV index is “moderate” or above, but even if it’s “low”, it doesn’t hurt to include it as part of your skincare routine.
But what if sunscreens are dangerous?
Firstly, not all sunscreens are created equal:
Learn more: Who Screens The Sunscreens?
Secondly: consider putting on a protective layer of moisturizer first, and then the sunscreen on top. Bear in mind, this is winter we’re talking about, so you’re probably not going out in a bikini, so this is likely a face-neck-hands job and you’re done.
What about vitamin D?
Humans evolved to have more or less melanin in our skin depending on where we lived, and white people evolved to wring the most vitamin D possible out of the meagre sun far from the equator. Black people’s greater melanin, on the other hand, offers some initial protection against the sun (but any resultant skin cancer is then more dangerous than it would be for white people if it does occur, so please do use sunscreen whatever your skintone).
Nowadays many people live in many places which may or may not be the places we evolved for, and so we have to take that into account when it comes to sun exposure.
Here’s a deeper dive into that, for those who want to learn:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: