You May Have More Air Pollution In Your Home Than In The Street
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Certainly, gas stoves and heaters can cause indoor air pollution, with carbon monoxide (CO) being the main risk. Even if you have a CO alarm, the level at which it will go off is usually the “this will kill you tonight if you don’t do something about it soon” level, rather than the “this will slowly kill your brain cells but you’ll keep functioning otherwise, until one day you don’t” levels of CO.
Still, do by all means have a CO alarm if you have anything in your house that can release CO!
Fun fact about those stoves:
❝Just 1 kilogram of cooking fuel emits 10 quadrillion particles smaller than 3 nanometers, which matches or exceeds what’s emitted from cars with internal combustion engines.
At that rate, you might be inhaling 10-100 times more of these sub-3 nanometer particles from cooking on a gas stove indoors than you would from car exhaust while standing on a busy street.❞
But today, we’re not here about that
Rather, we are looking at some more innocent-seeming things, such as scented cleaning products and air fresheners. Notably, the biggest problem is often not even the cleaning chemicals themselves. Of course: please don’t breathe bleach fumes, etc.
But that’s an obvious risk, and today we’re about the less obvious risks.
So… What is the less obvious risk here?
It’s the fragrances. The terpenes used to hold them react with ozone in the air, to create new nanoparticles. And, just like the nanoparticles from the stove, these can reach very high concentrations indoors, and suffice it to say, if you can smell the fragrance then you have the pollutants inside you.
You can read about how badly different products score, here:
Rapid Nucleation and Growth of Indoor Atmospheric Nanocluster Aerosol during the Use of Scented Volatile Chemical Products in Residential Buildings ← you’ll need to scroll down to the table with different cleaning products and air fresheners
Further, the seemingly-harmless scented candle is, as it turns out, quite a menace too:
❝Full-scale emission experiments were conducted in the Purdue zEDGE Test House using a variety of scented candles (n = 5) and wax warmers/melts (n = 14) under different outdoor air exchange rates (AERs). Terpene concentrations were measured in real-time using a proton transfer reaction time-of-flight mass spectrometer (PTR-TOF-MS). PTR-TOF-MS measurements revealed that scented candle and wax warmer/melt products emit a variety of monoterpenes (C10H16) and oxygen-containing monoterpenoids (C10H14O, C10H16O, C10H18O, C10H20O), with peak concentrations in the range of 10−1 to 102 ppb. Monoterpene EFs were much greater for scented wax warmers/melts (C10H16 EFs ∼ 102 mg per g wax consumed) compared to scented candles (C10H16 EFs ∼ 10−1 to 100 mg per g wax consumed). Significant emissions of reactive terpenes from both products, along with nitrogen oxides (NO, NO2) from candles, depleted indoor ozone (O3) concentrations. Terpene iFs were similar between the two products (iFs ∼ 103 ppm) and increased with decreasing outdoor AER. Terpene iFs during concentration decay periods were similar to, or greater than, iFs during active emission periods for outdoor AERs ≤ 3.0 h−1.
Overall, scented wax warmers/melts were found to release greater quantities of monoterpenes compared to other fragranced consumer products used in the home, including botanical disinfectants, hair care products, air fresheners, and scented sprays.❞
Put in fewer words: scented candles are bad, and wax melts (the kind with no flame, that one might easily expect to thus produce fewer emissions) are at least as bad if not worse, and both are even worse than cleaning products.
Some of the same research team conducted further studies, because of this this, finding:
❝We performed field measurements in a residential test house to investigate atmospheric nanoparticle formation from scented wax melt use. We employed a high-resolution particle size magnifier-scanning mobility particle sizer (PSMPS) and a proton transfer reaction time-of-flight mass spectrometer (PTR-TOF-MS) for real-time monitoring of indoor atmospheric nanoparticle size distributions and terpene mixing ratios, respectively.
Our findings reveal that terpenes released from scented wax melts react with indoor atmospheric ozone (O3) to initiate new particle formation (NPF) events, resulting in significant indoor atmospheric nanoparticle concentrations (>106 cm–3) comparable to those emitted by combustion-based scented candles, gas stoves, diesel engines, and natural gas engines.
We show that scented wax melt-initiated NPF events can result in significant respiratory exposures, with nanoparticle respiratory tract deposited dose rates similar to those determined for combustion-based sources.
Our results challenge the perception of scented wax melts as a safer alternative to combustion-based aromatherapy❞
Read in full: Flame-Free Candles Are Not Pollution-Free: Scented Wax Melts as a Significant Source of Atmospheric Nanoparticles
In short: you might want to ditch the fragranced products!
Want to do more?
Give your household hair a makeover with this multi-vector approach to deal with different risks:
What’s Lurking In Your Household Air?
For that matter, the air is a very important factor for the health of your lungs (and thus, for the health of everything that’s fed oxygen by your lungs), and there are more things we can do in that regard as well:
Seven Things To Do For Good Lung Health!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
High-Protein Paneer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Paneer (a kind of Desi cheese used in many recipes from that region) is traditionally very high in fat, mostly saturated. Which is delicious, but not exactly the most healthy.
Today we’ll be making a plant-based paneer that does exactly the same jobs (has a similar texture and gentle flavor, takes on the flavors of dishes in the same way, etc) but with a fraction of the fat (of which only a trace amount is saturated, in this plant-based version), and even more protein. We’ll use this paneer in some recipes in the future, but it can be enjoyed by itself already, so let’s get going…
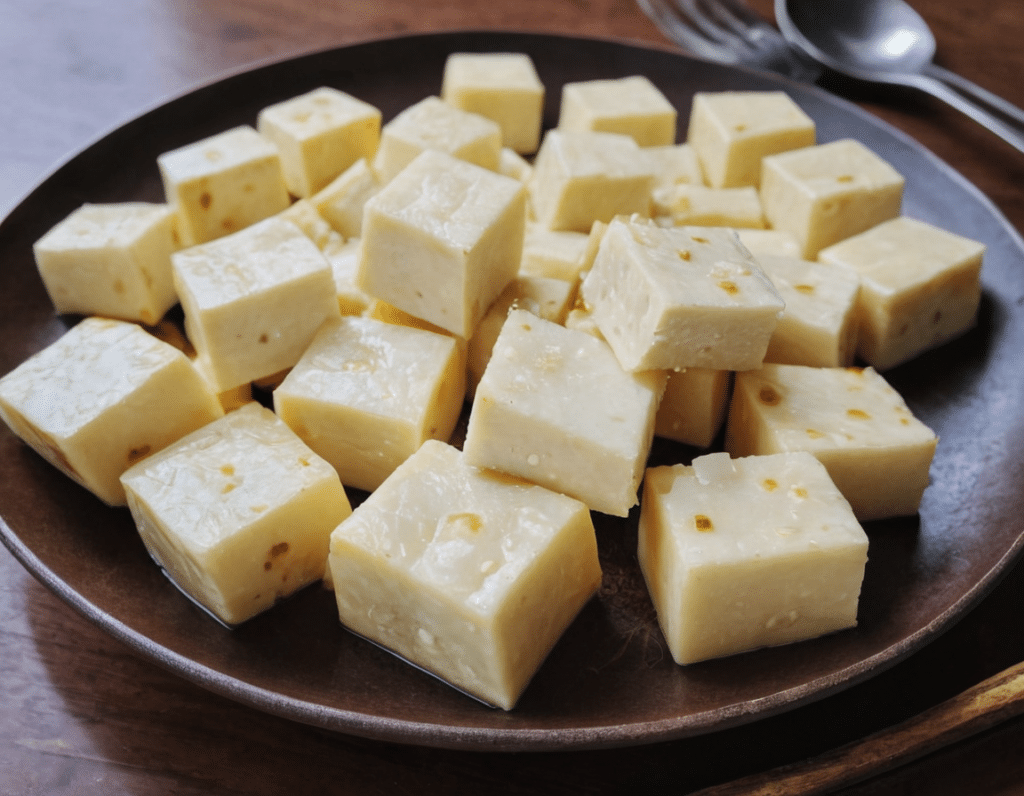
You will need
- ½ cup gram flour (unwhitened chickpea flour)
- Optional: 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Whisk the flour (and salt, if using) with 2 cups water in a big bowl, whisking until the texture is smooth.
2) Transfer to a large saucepan on a low-to-medium heat; you want it hot, but not quite a simmer. Keep whisking until the mixture becomes thick like polenta. This should take 10–15 minutes, so consider having someone else to take shifts if the idea of whisking continually for that long isn’t reasonable to you.
3) Transfer to a non-stick baking tin that will allow you to pour it about ½” deep. If the tin’s too large, you can always use a spatula to push it up against two or three sides, so that it’s the right depth
3) Refrigerate for at least 10 minutes, but longer is better if you have the time.
4) When ready to serve/use, cut it into ½” cubes. These can be served/used now, or kept for about a week in the fridge.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
Take care!
Share This Post
-
Sweet Dreams Are Made of THC (Or Are They?)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I’m one of those older folks that have a hard time getting 7 hrs. I know a lot of it my fault…like a few beers at nite…🥰am now trying THC gummies for anxiety, instead of alcohol……less calories 😁how does THC affect our sleep,? Safer than alcohol…..I know your next article 😊😊😊😊❣️😊alot of us older kids do take gummies 😲😲😲thank you❞
Great question! We wrote a little about CBD gummies (not THC) before:
…and went on to explore THC’s health benefits and risks here:
For starters, let’s go ahead and say: you’re right that it’s safer (for most people) than alcohol—but that’s not a strong claim, because alcohol is very bad for pretty much everything, including sleep.
So how does THC measure up when it comes to sleep quality?
Good news: it affects the architecture of sleep in such a way that you will spend longer in deep sleep (delta wave activity), which means you get more restorative and restful sleep!
See also: Alpha, beta, theta: what are brain states and brain waves? And can we control them?
Bad news: it does so at the cost of reducing your REM sleep, which is also necessary for good brain health, and will cause cognitive impairment if you skip too much. Normally, if you are sleep-deprived, the brain will prioritize REM sleep at the cost of other kinds of sleep; it’s that important. However, if you are chemically impaired from getting healthy REM sleep, there’s not much your brain can do to save you from the effects of REM sleep loss.
See: Cannabis, Cannabinoids, and Sleep: a Review of the Literature
This is, by the way, a reason that THC gets prescribed for some sleep disorders, in cases where the initial sleep disruption was because of nightmares, as it will reduce those (along with any other dreams, as collateral damage):
One thing to be careful of if using THC as a sleep aid is that withdrawal may make your symptoms worse than they were to start with:
Updates in the use of cannabis for insomnia
With all that in mind, you might consider (if you haven’t already tried it) seeing whether CBD alone improves your sleep, as while it does also extend time in deep sleep, it doesn’t reduce REM nearly as much as THC does:
👆 this study was paid for by the brand being tested, so do be aware of potential publication bias. That’s not to say the study is necessarily corrupt, and indeed it probably wasn’t, but rather, the publication of the results was dependent on the company paying for them (so hypothetically they could have pulled funding from any number of other research groups that didn’t get the results they wanted, leaving this one to be the only one published). That being said, the study is interesting, which is why we’ve linked it, and it’s a good jumping-off-point for finding a lot of related papers, which you can see listed beneath it.
CBD also has other benefits of its own, even without THC:
CBD Oil: What Does The Science Say?
Take care!
Share This Post
-
Severe Complications for Pregnant Veterans Nearly Doubled in the Last Decade, a GAO Report Finds
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Series: Post-Roe America:Abortion Access Divides the Nation
After the Supreme Court overturned Roe v. Wade, ending nearly 50 years of federal protection for abortion, some states began enforcing strict abortion bans while others became new havens for the procedure. ProPublica is investigating how sweeping changes to reproductive health care access in America are affecting people, institutions and governments.
Over the past decade, the rate of veterans suffering severe pregnancy complications has risen dramatically, a new federal report found.
Veterans have raced to the hospital with dangerous infections, kidney failure, aneurysms or blood loss. They’ve required hysterectomies, breathing machines and blood transfusions to save their lives. Between 2011 and 2020, 13 veterans died after such complications.
The report found that among people getting health care benefits through the Department of Veterans Affairs, the rate of severe complications nearly doubled during that time, from about 93 per 10,000 hospitalizations in 2011 to just over 184 per 10,000 hospitalizations in 2020. Black veterans had the highest rates.
The report, which was put together by the Government Accountability Office, also made recommendations for reducing the problem, which focus on conducting more routine screenings throughout pregnancy and in the postpartum period.
“It is imperative that the VA help ensure veterans have the healthiest pregnancy outcomes possible,” the report said, highlighting the increasing number of veterans using the agency’s maternity benefits as well as the troublesome complication rates faced by Black women.
The report’s findings are an unfortunate trend, said Alyssa Hundrup, director of health care at the GAO. The office analyzed data on 40,000 hospitalizations related to deliveries paid for by the VA. It captures a time period before 21 states banned or greatly restricted abortion and the military was thrust into a political battle over whether it would pay for active service members to travel for abortion care if a pregnancy was a risk to their health.
Hundrup, who led the review, said the analysis included hospital records from days after delivery to a year postpartum. The report was mandated after Congress passed a law in 2021 that aimed to address the maternal health crisis among veterans. The law led to a $15 million investment in maternity care coordination programs for veterans.
The report recommended that the VA analyze and collect more data on severe complications as well as data on the mental health, race and ethnicity of veterans who experience complications to understand the causes behind the increase and the reasons for the disparity. The report also states that oversight is needed to ensure screenings are being completed.
Studies show there’s a connection between mental health conditions and pregnancy-related complications, VA officials said.
The report recommended expanding the screening questions that providers ask patients at appointments to glean more information about their mental health, including anxiety and PTSD symptoms. It urged the VA to review the data more regularly.
“You don’t know what you don’t measure,” Hundrup said in an interview with ProPublica.
The VA health system, which historically served a male population, does not provide maternity care at its facilities. Instead, the agency has outsourced maternity care. But when patients were treated by those providers, the VA failed to track whether they were getting screened for other health issues and mental health problems.
Officials hope the improved data collection will help the VA study underlying issues that may lead to complications. For example, do higher rates of anxiety have a connection to rates of high blood pressure in pregnant people?
VA officials are working with a maternal health review committee to monitor the data as it is gathered. The agency recently conducted its first review of data going back five years about pregnancy-related complications, said Dr. Amanda Johnson, acting head of the VA’s Office of Women’s Health, who is overseeing the implementation of the report’s recommendations.
The VA has created a dashboard to monitor pregnant veterans’ health outcomes. The VA’s data analysis team will also examine the impact of veterans’ ages on complications and whether they differ for people who live in urban and rural areas.
VA officials will begin to review mental health screenings conducted by maternal care coordinators in March. The coordinators advocate for veterans, helping them between health care visits, whether their providers are inside or outside the VA.
Johnson said that reducing racial and ethnic disparities is a priority for the agency. In 2018, ProPublica published “Lost Mothers,” a series that shed light on the country’s maternal health crisis. Studies have shown that in the general population, Black women are three times more likely than white women to die from pregnancy-related complications. While deaths made up only a small portion of the bad outcomes for Black veterans cited in the report, VA care could not spare them from elevated rates of severe complications. Johnson said the maternal health crisis also persists within the VA.
“There is a disparity,” Johnson said. “We are not immune to that.”
Research shows pregnant people who have used the VA’s coverage have higher rates of trauma and mental conditions that can increase their risks of complications and bad outcomes.
This may be because many people who join the military enter it having already faced trauma, said Dr. Laura Miller, a psychiatrist and the medical director of reproductive mental health at the VA.
She said veterans with PTSD have higher rates of complications such as preeclampsia, a potentially fatal condition related to high blood pressure, gestational diabetes and postpartum depression. If untreated during pregnancy, depression also increases the likelihood of preterm birth and lingering problems for babies.
Hundrup said she hopes this proactive work will improve maternal health.
“We want these numbers trending in the other direction,” Hundrup said.
Share This Post
Related Posts
-
Wrong Arm Position = Wrong Measurement Of Blood Pressure
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is especially important to know if you measure your own blood pressure at home.
Even if you don’t, it’s still good to know this as healthcare providers also can (and often will) do it wrong, especially if they are under time pressure (e.g. they need to get you out of their office and the next person in):
From the heart
Many things can change our blood pressure, and even gravity changes (considerably!) our blood pressure locally.
For example, even with good circulation, so long as we are in the Earth’s gravity under normal conditions (e.g. not skydiving, not riding a rollercoaster, etc), our blood pressure will always be higher below our heart, and lower above it, because gravity is pulling our blood downwards; this is also why if your circulation is not good, you may feel light-headed upon sitting up or standing up, as the bloodstream takes a moment to win a battle against gravity. This is also why blood rushes to your head if you are hanging upside down—increasing the local blood pressure in your head, which unlike your feet, isn’t used to it, so you feel it, and the effect may be visible from the outside, too.
When it comes to having your arm above or below your heart, the difference is less pronounced as it’s only a small change, but that small change can make a big difference:
- If the cuff is above heart level → Lower blood pressure reading.
- If the cuff is below heart level → Higher blood pressure reading.
- Every 1-inch difference causes a 2 mmHg change in readings.
For the reading to be accurate, the blood pressure cuff therefore needs to be at the same height as your heart.
You may be thinking: “my heart is bigger than an inch; do I aim for the middle?”
And the answer is: ideally the cuff should be at the same height as the right atrium of the heart, which is under the midpoint of the sternum.
However, your arm needs to be supported at that height, because if you have to keep it there using your own power, that will mean a tensing of your muscles, and increase in both heart rate and blood pressure. In fact, studies cited in the video found:
- Unsupported arm, in healthy patients → Systolic +8 mmHg, Diastolic +7 mmHg.
- Unsupported arm, in high blood pressure patients → Systolic +23 mmHg, Diastolic +10 mmHg.
Some other considerations; firstly, correct sitting posture:
- Sit upright with back support
- Feet flat on the floor, legs uncrossed
- Arm should be outward from the body and, as per the above explanation, supported (armrest, table, etc.)
And finally, you should be relaxed and at rest.
For example, your writer here is due for a regular checkup in a couple of weeks, and usually when I go there, I will have walked a couple of miles to get there, then bounced cheerfully up 6 flights of stairs. However, for this appointment, I will need to make sure to arrive early, so that I have time for my (so far as I know, happy and healthy) heart to return to its resting pulse and blood pressure.
Also, if you are anything like this writer, the blood pressure cuff activating is not a relaxing experience (and so invites a higher pulse and blood pressure), so it’s better to take three readings and then discard the first one, and record the average of the second two (I do it this way at home).
Similarly, if a medical environment in general is stressful for you, then taking two minutes to do a little mindfulness meditation, or even just breathing exercises, can be good.
For more on all of these, plus also comments on issues such as correct cuff size and tightness, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Common Hospital Blood Pressure Mistake (Don’t Let This Happen To You Or A Loved One)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Your Brain Is Really Doing When You’re Doing “Nothing”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Unless we are dead, our brain is never truly inactive. And it’s not just a matter of regulating autonomic functions, either…
Default Mode Network
When the brain is at rest but not necessarily asleep, the Default Mode Network (DMN) engages. This makes up for around 20% of the brain’s overall activity, and contributes to complex cognitive processes.
What constitutes “at rest”: the DMN activates when external tasks stop and is engaged during self-reflection, mind-wandering, and relaxed memory recall (i.e. reminiscing, rather than answering questions in a difficult test, for example).
As for its neurophysiology, the DMN is connected to the hippocampus and plays a key role in episodic, prospective, and semantic memory (memories of experiences, future plans, and general knowledge), as well as being involved in self-reflection, social cognition, and understanding others’ thoughts (theory of mind). The DMN thus also helps integrate memories and thoughts to create a cohesive internal narrative and sense of self.
However, it doesn’t work alone: the DMN interacts with other networks like the salience network, which switches attention to external stimuli. Disruptions between these networks are linked to psychiatric disorders (e.g., schizophrenia, Alzheimer’s, depression), in various different ways depending on the nature of the disruption.
Sometimes, for some people in some circumstances, the option to disrupt the DMN is useful. For example, research shows that psilocybin disrupts the DMN, leading to changes in brain activity and potential therapeutic benefits for depression* and other psychiatric disorders by enhancing neuroplasticity.
*Essentially, kicking the brain out of the idling gear it got stuck in, and into action
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- The Wandering Mind – by Dr. Michael Corballis ← a book, largely about the DMN and how to use it beneficially
- Taking A Trip Through The Evidence On Psychedelics ← for a shorter read, touching on psilocybin
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Uric Acid’s Extensive Health Impact (And How To Lower It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Uric Acid’s Extensive Health Impact (And How To Lower It)
This is Dr. David Perlmutter. He’s a medical doctor, and a Fellow of the American College of Nutrition. He’s a member of the Editorial Board for the Journal of Alzheimer’s Disease, and has been widely published in many other peer-reviewed journals.
What does he want us to know?
He wants us to know about the health risks of uric acid (not something popularly talked about so much!), and how to reduce it.
First: what is it? Uric acid is a substance we make in our own body. However, unlike most substances we make in our body, we have negligible use for it—it’s largely a waste product, usually excreted in urine.
However, if we get too much, it can build up (and crystallize), becoming such things as kidney stones, or causing painful inflammation if it shows up in the joints, as in gout.
More seriously (unpleasant as kidney stones and gout may be), this inflammation can have a knock-on effect triggering (or worsening) other inflammatory conditions, ranging from non-alcoholic fatty liver disease, to arthritis, to dementia, and even heart problems. See for example:
- David Perlmutter | Uric Acid and Cognitive Decline
- American Heart Association | Uric acid linked to later risk for irregular heart rhythm
- World Journal of Gastroenterology | The role of uric acid in non-alcoholic steatohepatitis development
How can we reduce our uric acid levels?
Uric acid is produced when we metabolize purine nucleotides, which are found in many kinds of food. We can therefore reduce our uric acid levels by reducing our purine intake, as well as things that mess up our liver’s ability to detoxify things. Offsetting the values for confounding variables (such as fiber content, or phytochemicals that mitigate the harm), the worst offenders include…
Liver-debilitating things:
- Alcohol (especially beer)
- High-fructose corn syrup (and other fructose-containing things that aren’t actual fruit)
- Other refined sugars
- Wheat / white flour products (this is why beer is worse than wine, for example; it’s a double-vector hit)
Purine-rich things:
- Red meats and game
- Organ meats
- Oily fish, and seafood (great for some things; not great for this)
Some beans and legumes are also high in purines, but much like real fruit has a neutral or positive effect on blood sugar health despite its fructose content, the beans and legumes that are high in purines, also contain phytochemicals that help lower uric acid levels, so have a beneficial effect.
Eggs (consumed in moderation) and tart cherries have a uric-acid lowering effect.
Water is important for all aspects of health, and doubly important for this.
Hydrate well!
Lifestyle matters beyond diet
The main key here is metabolic health, so Dr. Perlmutter advises the uncontroversial lifestyle choices of moderate exercise and good sleep, as well as (more critically) intermittent fasting. We wrote previously on other things that can benefit liver health:
…in this case, that means the liver gets a break to recuperate (something it’s very good at, but does need to get a chance to do), which means that while you’re not giving it something new to do, it can quickly catch up on any backlog, and then tackle any new things fresh, next time you start eating.
Want to know more about this from Dr. Perlmutter?
You might like his article:
An Integrated Plan for Lowering Uric Acid ← more than we had room for here; he also talks about extra things to include in your diet/supplementation regime for beneficial effects!
And/or his book:
…on which much of today’s main feature was based.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: