Which Style Of Yoga Is Best For You?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For you personally, that is—so let’s look at some options, their benefits, and what kind of person is most likely to benefit from each.
Yoga is, of course, an ancient practice, and like any ancient practice, especially one with so many practitioners (and thus also: so many teachers), there are very many branches to the tree of variations, that is to say, different schools and their offshoots.
Since we cannot possibly cover all of them, we’ll focus on five broad types that are popular (and thus, likely available near to you, unless you live in a very remote place):
Hatha Yoga
This is really the broadest of umbrella categories for yoga as a physical practice of the kind that most immediately comes to mind in the west:
- Purpose: energizes the practitioner through controlled postures and breath.
- Practice: non-heated, slow asanas held for about a minute with intentional transitions
- Benefits: reduces stress, improves flexibility, tones muscles, and boosts circulation.
- Best for: beginners with an active lifestyle.
Vinyasa Yoga
You may also have heard of this called simply “Flow”, without reference to the Mihaly Csikszentmihalyi sense of the word. Rather, it is about a flowing practice:
- Purpose: builds heat and strength through continuous, flowing movement paired with breath.
- Practice: dynamic sequences of the same general kind as the sun salutation, leading to a final resting pose.
- Benefits: enhances heart health, strengthens core, tones muscles, and improves flexibility.
- Best for: beginner to intermediate yogis seeking a cardio-based practice.
Hot Yoga
This one’s well-known and the clue is in the name; it’s yoga practised in a very hot room:
- Purpose: uses heat to increase heart rate, and loosen muscles.
- Practice: heated studio (32–42℃, which is 90–108℉), often with vinyasa flows, resulting in heavy sweating*
- Benefits: burns calories, improves mood, enhances skin, and builds bone density.
- Best for: intermediate yogis comfortable with heat; not recommended for certain health conditions.
*and also sometimes heat exhaustion / heat stroke. This problem arises most readily when the ambient temperature is higher than human body temperature, because that is the point at which sweating ceases to fulfil its biological function of cooling us down.
Noteworthily, a study found that doing the same series of yoga postures in the same manner, but without the heat, produced the same health benefits without the risk:
❝The primary finding from this investigation is that the hatha yoga postures in the Bikram yoga series produce similar enhancements in endothelium-dependent vasodilatation in healthy, middle-aged adults regardless of environmental temperature. These findings highlight the efficacy of yoga postures in producing improvements in vascular health and downplay the necessity of the heated practice environment in inducing vascular adaptations.❞
(“Bikram yoga” is simply the brand name of a particular school of hot yoga)
Yin Yoga
This is a Chinese variation, and is in some ways the opposite of the more vigorous forms, being gentler in pretty much all ways:
- Purpose: promotes deep tissue stretching and circulation by keeping muscles cool.
- Practice: passive, floor-based asanas held for 5–20 minutes in a calming environment.
- Benefits: increases flexibility, enhances circulation, improves mindfulness, and emotional release.
- Best for: all levels, regardless of health or flexibility.
Restorative Yoga
This is often tailored to a specific condition, but it doesn’t have to be:
- Purpose: encourages relaxation and healing through supported, restful poses.
- Practice: reclined, prop-supported postures in a soothing, low-lit setting.
- Benefits: relieves stress, reduces chronic pain, calms the nervous system, and supports healing.
- Best for: those recovering from illness/injury or managing emotional stress.
See for example: Yoga Therapy for Arthritis: A Whole-Person Approach to Movement and Lifestyle
Want to know more?
If you’re still unsure where to start, check out:
Yoga Teacher: “If I wanted to get flexible (from scratch) in 2025, here’s what I’d do”
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
HRT Side Effects & Troubleshooting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Heather Hirsch. She’s a board-certified internist, and her clinical expertise focuses on women’s health, particularly in midlife and menopause, and its intersection with chronic diseases (ranging from things associated with sexual health, to things like osteoporosis and heart disease).
So, what does she want us to know?
HRT can be life-changingly positive, but it can be a shaky start
Hormone Replacement Therapy (HRT), and in this context she’s talking specifically about the most common kind, Menopausal Hormone Therapy (MHT), involves taking hormones that our body isn’t producing enough of.
If these are “bioidentical hormones” as used in most of the industrialized world and increasingly also in N. America, then this is by definition a supplement rather than a drug, for what it’s worth, whereas some non-bioidentical hormones (or hormone analogs, which by definition function similarly to hormones but aren’t the same thing) can function more like drugs.
We wrote a little about his previously:
Hormone Replacement Therapy: A Tale Of Two Approaches
For most people most of the time, bioidentical hormones are very much the best way to go, as they are not only more effective, but also have fewer side effects.
That said, even bioidentical hormones can have some undesired effects, so, how to deal with those?
Don’t worry; bleed happy
A reprise of (usually quite light) menstrual bleeding is the most common side effect of menopausal HRT.
This happens because estrogen affects* the uterus, leading to a build-up and shedding of the uterine lining.
*if you do not have a uterus, estrogen can effect uterine tissue. That’s not a typo—here we mean the verb “effect”, as in “cause to be”. It will not grow a new uterus, but it can cause some clumps of uterine tissue to appear; this means that it becomes possible to get endometriosis without having a uterus. This information should not be too shocking, as endometriosis is a matter of uterine tissue growing inconveniently, often in places where it shouldn’t, and sometimes quite far from the uterus (if present, or its usual location, if absent). However, the risk of this happening is far lower than if you actually have a uterus:
What you need to know about endometriosis
Back to “you have a uterus and it’s making you wish you didn’t”:
This bleeding should, however, be light. It’ll probably be oriented around a 28-day cycle even if you are taking your hormones at the same dose every day of the month, and the bleeding will probably taper off after about 6 months of this.
If the bleeding is heavier, all the time, or persists longer than 6 months, then speak to your gynecologist about it. Any of those three; it doesn’t have to be all three!
Bleeding outside of one’s normal cycle can be caused by anything from fibroids to cancer; statistically speaking it’s probably nothing too dire,but when your safety is in question, don’t bet on “probably”, and do get it checked out:
When A Period Is Very Late (i.e., Post-Menopause)
Dr. Hirsch recommends, as possible remedies to try (preferably under your gynecologist’s supervision):
- lowering your estrogen dose
- increasing your progesterone dose
- taking progesterone continuously instead of cyclically
And if you’re not taking progesterone, here’s why you might want to consider taking this important hormone that works with estrogen to do good things, and against estrogen to rein in some of estrogen’s less convenient things:
Progesterone Menopausal HRT: When, Why, And How To Benefit
(the above link contains, as well as textual information, an explanatory video from Dr. Hirsch herself)
Get the best of the breast
Calm your tits. Soothe your boobs. Destress your breasts. Hakuna your tatas. Undo the calamity beleaguering your mammaries.
Ok, more seriously…
Breast tenderness is another very common symptom when starting to take estrogen. It can worry a lot of people (à la “aagh, what is this and is it cancer!?”), but is usually nothing to worry about. But just to be sure, do also check out:
Keeping Abreast Of Your Cancer Risk: How To Triple Your Breast Cancer Survival Chances
Estrogen can cause feelings of breast fullness, soreness, nipple irritation, and sometimes lactation, but this later will be minimal—we’re talking a drop or two now and again, not anything that would feed a baby.
Basically, it happens when your body hasn’t been so accustomed to normal estrogen levels in a while, and suddenly wakes up with a jolt, saying to itself “Wait what are we doing puberty again now? I thought we did menopause? Are we pregnant? What’s going on? Ok, checking all systems!” and then may calm down not too long afterwards when it notes that everything is more or less as it should be already.
If this persists or is more than a minor inconvenience though, Dr. Hirsch recommends looking at the likely remedies of:
- Adjust estrogen (usually the cause)
- Adjust progesterone (less common)
- If it’s progesterone, changing the route of administration can ameliorate things
What if it’s not working? Is it just me?
Dr. Hirsch advises the most common reasons are simply:
- wrong formulation (e.g. animal-derived estrogen or hormone analog, instead of bioidentical)
- wrong dose (e.g. too low)
- wrong route of administration (e.g. oral vs transdermal; usually transdermal estradiol is most effective but many people do fine on oral; progesterone meanwhile is usually best as a pessary/suppository, but many people do fine on oral)
Writer’s example: in 2022 there was an estrogen shortage in my country, and while I had been on transdermal estradiol hemihydrate gel, I had to go onto oral estradiol valerate tablets for a few months, because that’s what was available. And the tablets simply did not work for me at all. I felt terrible and I have a good enough intuitive sense of my hormones to know when “something wrong is not right”, and a good enough knowledge of the pharmacology & physiology to know what’s probably happening (or not happening). And sure enough, when I got my blood test results, it was as though I’d been taking nothing. It was such a relief to get back on the gel once it became available again!
So, if something doesn’t seem to be working for you, speak up and get it fixed if at all possible.
See also: What You Should Have Been Told About Menopause Beforehand
Want to know more from Dr. Hirsch?
You might like this book of hers, which we haven’t reviewed yet, but present here for your interest:
Enjoy!
Share This Post
-
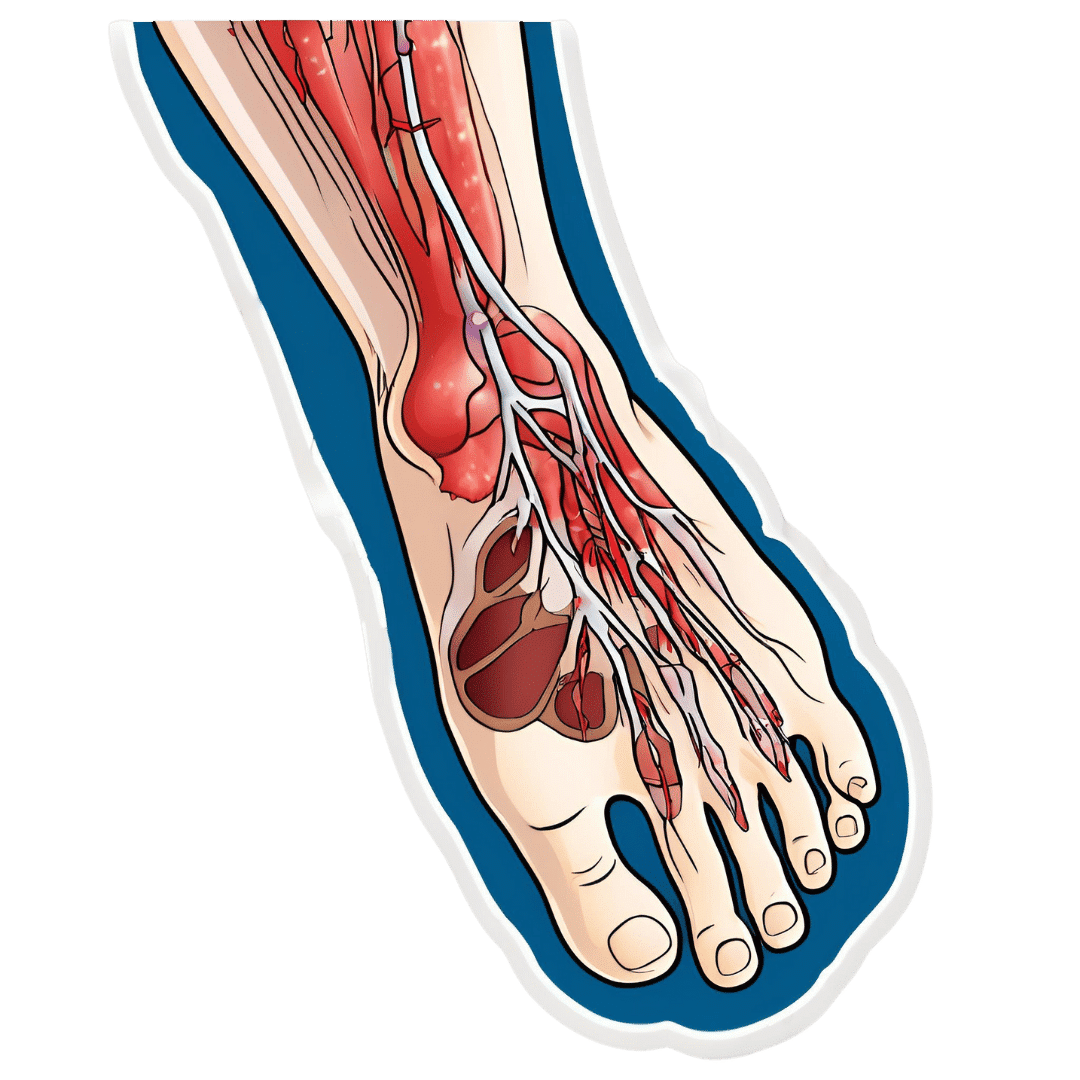
How To Stay A Step Ahead Of Peripheral Artery Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Far less well-known than Coronary Artery Disease, it can still result in loss of life and limb (not in that order). Fortunately, there are ways to be on your guard:
What it is
Peripheral Artery Disease (PAD) is the same thing as Coronary Artery Disease (CAD), just, in the periphery—which by definition means “outside of the heart and brain”, but in practice, it starts with the extremities. And of the extremities, it tends to start with the feet and legs, for the simple reason that if someone’s circulation is sluggish, then because of gravity, that’s where’s going to get blocked first.
In both CAD and PAD, the usual root cause is atherosclerosis, that is to say, the build-up of fatty material inside the arteries, usually commensurate to LDL (“bad”) cholesterol, especially in men (high LDL is still a predictor of cardiovascular disease in women though, just more modestly so, at least pre-menopause or in cases of treated menopause whereby HRT has returned hormones to pre-menopause levels).
See also: Demystifying Cholesterol
And for that about sex differences: His & Hers: The Hidden Complexities of Statins and Cardiovascular Disease (CVD)
Why it is
This one’s straightforward, as it’s the same things as any kind of cardiovascular disease: high blood pressure, high cholesterol, older age, obesity, smoking, drinking, diabetes, and genetic factors (so, a risk factor is: family history of heart disease).
However, while those are the main causes and/or risk factors, it absolutely can still strike other people, so it’s as well to be watch out for…
What to look out for
Many people first notice signs and symptoms that turn out to be PAD when they experience pain or numbness in the foot or feet, and/or a discoloration of the feet (especially toes), and slow wound healing.
At that stage, chances are you will need to go urgently to a specialist, and surgery is a likely necessity. With a little luck, it’ll be a minimally-invasive surgery to unblock an artery; failing that, an amputation will be in order.
At that stage, under 50% will be alive 5 years from diagnosis:
You probably want to avoid those. Good news is, you can, by catching it earlier!
What to look out for before that
The most common test for PAD is one you can do at home, but enlisting a nurse to do it for you will help ensure accurate readings. It’s called the Ankle-Brachial Index (ABI) test, and it involves comparing the blood pressure in your ankle with the blood pressure in your arm, and expressing them as a ratio.
Here’s how to do it (instructions and a video demonstration if you want it):
Do Try This At Home: ABI Test For Clogged Arteries
If you need a blood pressure monitor, by the way, here’s an example product on Amazon.
- A healthy ABI score is between 1.0 and 1.4; anything outside this range may indicate arterial problems.
- Low ABI scores (below 0.8) suggest plaque is likely obstructing blood flow
- High ABI scores (above 1.4) may indicate artery hardening
Do note also that yes, if you have plaque obstructing blood flow and hardened arteries, your scores may cancel out and give you a “healthy” score, despite your arteries being very much not healthy.
For this reason, this test can be used to raise the alarm, but not to give the “all clear”.
There are other tests that clinicians can do for you, but you can’t do at home unless you have an MRI machine, a CT scanner, an x-ray machine, a doppler-and-ultrasound machine, etc. We’ll not go into those in detail here, but ask your doctor about them if you’re concerned.
What to do about it
In the mid-to-late stages of the disease, the options are medication and surgery, respectively, but your doctor will advise about those in that eventuality.
In the early stages of the disease, the first-line recommend treatment is exercise, of which, especially walking:
Lower Extremity Peripheral Artery Disease: Diagnosis and Treatment
Given that this more often happens when someone hasn’t been walking so much, it can be a walk-rest-walk approach at first (a treadmill on a low setting can be very useful for this):
See also: Exercise Comparison Head-to-Head: Treadmill vs Road
Take care!
Share This Post
-
Terminal lucidity: why do loved ones with dementia sometimes ‘come back’ before death?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dementia is often described as “the long goodbye”. Although the person is still alive, dementia slowly and irreversibly chips away at their memories and the qualities that make someone “them”.
Dementia eventually takes away the person’s ability to communicate, eat and drink on their own, understand where they are, and recognise family members.
Since as early as the 19th century, stories from loved ones, caregivers and health-care workers have described some people with dementia suddenly becoming lucid. They have described the person engaging in meaningful conversation, sharing memories that were assumed to have been lost, making jokes, and even requesting meals.
It is estimated 43% of people who experience this brief lucidity die within 24 hours, and 84% within a week.
Why does this happen?
Terminal lucidity or paradoxical lucidity?
In 2009, researchers Michael Nahm and Bruce Greyson coined the term “terminal lucidity”, since these lucid episodes often occurred shortly before death.
But not all lucid episodes indicate death is imminent. One study found many people with advanced dementia will show brief glimmers of their old selves more than six months before death.
Lucidity has also been reported in other conditions that affect the brain or thinking skills, such as meningitis, schizophrenia, and in people with brain tumours or who have sustained a brain injury.
Moments of lucidity that do not necessarily indicate death are sometimes called paradoxical lucidity. It is considered paradoxical as it defies the expected course of neurodegenerative diseases such as dementia.
But it’s important to note these episodes of lucidity are temporary and sadly do not represent a reversal of neurodegenerative disease.
Sadly, these episodes of lucidity are only temporary. Pexels/Kampus Production Why does terminal lucidity happen?
Scientists have struggled to explain why terminal lucidity happens. Some episodes of lucidity have been reported to occur in the presence of loved ones. Others have reported that music can sometimes improve lucidity. But many episodes of lucidity do not have a distinct trigger.
A research team from New York University speculated that changes in brain activity before death may cause terminal lucidity. But this doesn’t fully explain why people suddenly recover abilities that were assumed to be lost.
Paradoxical and terminal lucidity are also very difficult to study. Not everyone with advanced dementia will experience episodes of lucidity before death. Lucid episodes are also unpredictable and typically occur without a particular trigger.
And as terminal lucidity can be a joyous time for those who witness the episode, it would be unethical for scientists to use that time to conduct their research. At the time of death, it’s also difficult for scientists to interview caregivers about any lucid moments that may have occurred.
Explanations for terminal lucidity extend beyond science. These moments of mental clarity may be a way for the dying person to say final goodbyes, gain closure before death, and reconnect with family and friends. Some believe episodes of terminal lucidity are representative of the person connecting with an afterlife.
Why is it important to know about terminal lucidity?
People can have a variety of reactions to seeing terminal lucidity in a person with advanced dementia. While some will experience it as being peaceful and bittersweet, others may find it deeply confusing and upsetting. There may also be an urge to modify care plans and request lifesaving measures for the dying person.
Being aware of terminal lucidity can help loved ones understand it is part of the dying process, acknowledge the person with dementia will not recover, and allow them to make the most of the time they have with the lucid person.
For those who witness it, terminal lucidity can be a final, precious opportunity to reconnect with the person that existed before dementia took hold and the “long goodbye” began.
Yen Ying Lim, Associate Professor, Turner Institute for Brain and Mental Health, Monash University and Diny Thomson, PhD (Clinical Neuropsychology) Candidate and Provisional Psychologist, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Rapamycin Can Slow Aging By 20% (But Watch Out)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Rapamycin’s Pros & Cons
Rapamycin is generally heralded as a wonderdrug that (according to best evidence so far) can slow down aging, potentially adding decades to human lifespan—and yes, healthspan.
It comes from a kind of soil bacteria, which in turn comes from the island of Rapa Nui (a Chilean territory best known for its monumental moai statues), hence the name rapamycin.
Does it work?
Yes! Probably! With catches!
Like most drugs that are tested for longevity-inducing properties, research in humans is very slow. Of course for drugs in general, they must go through in vitro and in vivo animal testing first before they can progress to human randomized clinical trials, but for longevity-inducing drugs, it’s tricky to even test in humans, without waiting entire human lifetimes for the results.
Nevertheless, mouse studies are promising:
Rapamycin: An InhibiTOR of Aging Emerges From the Soil of Easter Island
(“Easter Island” is another name given to the island of Rapa Nui)
That’s not a keysmash in the middle there, it’s a reference to rapamycin’s inhibitory effect on the kinase mechanistic target of rapamycin, sometimes called the mammalian target of rapamycin, and either way generally abbreviated to “mTOR”—also known as “FK506-binding protein 12-rapamycin-associated protein 1” or “FRAP1“ to its friends, but we’re going to stick with “mTOR”.
What’s relevant about this is that mTOR regulates cell growth, cell proliferation, cell motility, cell survival, protein synthesis, autophagy, and transcription.
Don’t those words usually get associated with cancer?
They do indeed! Rapamycin and its analogs have well-demonstrated anti-cancer potential:
❝Rapamycin, the naturally occurring inhibitor of mTOR, along with a number of recently developed rapamycin analogs (rapalogs) consisting of synthetically derived compounds containing minor chemical modifications to the parent structure, inhibit the growth of cell lines derived from multiple tumor types in vitro, and tumor models in vivo.
Results from clinical trials indicate that the rapalogs may be useful for the treatment of subsets of certain types of cancer.❞
…and as such, gets used sometimes as an anticancer drug—especially against renal cancer. See also:
Research perspective: Cancer prevention with rapamycin
What’s the catch?
Aside from the fact that its longevity-inducing effects are not yet proven in humans, the mouse models find its longevity effects to be sex-specific, extending the life of male mice but not female ones:
Rapamycin‐mediated mouse lifespan extension: Late‐life dosage regimes with sex‐specific effects
One hypothesis about this is that it may have at least partially to do with rapamycin’s immunomodulatory effect, bearing in mind that estrogen is immune-enhancing and testosterone is immunosuppressant.
And rapamycin? That’s another catch: it is an immunosuppressant.
This goes in rapamycin’s favor for its use to avoiding rejection when it comes to some transplants (most notably including for kidneys), though the very same immunosuppressant effect is a reason it is contraindicated for certain other transplants (such as in liver or lung transplants), where it can lead to an unacceptable increase in risk of lymphoma and other malignancies:
Prescribing Information: Rapamune, Sirolimus Solution / Sirolimus Tablet
(Sirolimus is another name for rapamycin, and Rapamune is a brand name)
What does this mean for the future?
Researchers think that rapamycin may be able to extend human lifespan to a more comfortable 120–125 years, but acknowledge there’s quite a jump to get there from the current mouse studies, and given the current drawbacks of sex-specificity and immunosuppression:
Advances in anti-aging: Rapamycin shows potential to extend lifespan and improve health
Noteworthily, rapamycin has also shown promise in simultaneously staving off certain diseases associated most strongly with aging, including Alzheimer’s and cardiac disease—or even, starting earlier, to delay menopause, in turn kicking back everything else that has an uptick in risk peri- or post-menopause:
Effect of Rapamycin in Ovarian Aging (Rapamycin)
👆 an upcoming study whose results are thus not yet published, but this is to give an idea of where research is currently at. See also:
Pilot Study Evaluates Weekly Pill to Slow Ovarian Aging, Delay Menopause
Where can I try it?
Not from Amazon, that’s for sure!
It’s still tightly regulated, but you can speak with your physician, especially if you are at risk of cancer, especially if kidney cancer, about potentially being prescribed it as a preventative—they will be able to advise about safety and applicability in your personal case.
Alternatively, you can try getting your name on the list for upcoming studies, like the one above. ClinicalTrials.gov is a great place to watch out for those.
Meanwhile, take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
New News From The Centenarian Blue Zones
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From Blue To Green…
We sometimes write about supercentenarians, which word is usually used in academia to refer to people who are not merely over 100 years of age, but over 110 years. These people can be found in many countries, but places where they have been found to be most populous (as a percentage of the local population) have earned the moniker “Blue Zones”—of which Okinawa and Sardinia are probably the most famous, but there are others too.
This is in contrast to, for example “Red Zones”, a term often used for areas where a particular disease is endemic, or areas where a disease is “merely” epidemic, but particularly rife at present.
In any case, back to the Blue Zones, where people live the longest and healthiest—because the latter part is important too! See also:
- Lifespan: how long we live
- Healthspan: how long we stay healthy (portmanteau of “healthy lifespan”)
Most of our readers don’t live in a Blue Zone (in fact, many live in a COVID Red Zone, a diabetes Red Zone, and a heart disease Red Zone), but that doesn’t mean we can’t all take tips from the Blue Zones and apply them, for example:
- The basics: The Blue Zones’ Five Pillars Of Longevity
- Going beyond: The Five Key Traits Of Healthy Aging
You may be wondering… How much good will this do me? And, we do have an answer for that:
When All’s Said And Done, How Likely Are You To Live To 100?
Now that we’re all caught-up…
The news from the Blues
A team of researchers did a big review of observational studies of centenarians and near-centenarians (aged 95+). Why include the near-centenarians, you ask? Well, most of the studies are also longitudinal, and if we’re doing an observational study of the impact of lifestyle factors on a 100-year-old, it’s helpful to know what they’ve been doing recently. Hence nudging the younger-end cutoff a little lower, so as to not begin each study with fresh-faced 100-year-olds whom we know nothing about.
Looking at thousands of centenarians (and near-centenarians, but also including some supercentenarians, up the age of 118), the researchers got a lot of very valuable data, far more than we have room to go into here (do check out the paper at the bottom of this article, if you have time; it’s a treasure trove of data), but one of the key summary findings was a short list of four factors they found contributed the most to extreme longevity:
- A diverse diet with low salt intake: in particular, a wide variety of plant diversity, including protein-rich legumes, though fish featured prominently also. On average they got 57% and 65% of their energy intake from carbohydrates, 12% to 32% from protein, and 27% to 31% from fat. As for salt, they averaged 1.6g of sodium per day, which is well within the WHO’s recommendation of averaging under 2g of sodium per day. As a matter of interest, centenarians in Okinawa itself averaged 1.1g of sodium per day.
- Low medication use: obviously there may be a degree of non-causal association here, i.e. the same people who just happened to be healthier and therefore lived longer, correspondingly took fewer medications—they took fewer medications because they were healthier; they weren’t necessarily healthier because they took fewer medications. That said, overmedication can be a big problem, especially in places with a profit motive like the US, and can increase the risk of harmful drug interactions, and side effects that then need more medications to treat the side effects, as well as direct iatrogenic damage (i.e. this drug treats your condition, but as the cost of harming you in some other way). Naturally, sometimes we really do need meds, but it’s a good reminder to do a meds review with one’s doctor once in a while, and see if everything’s still of benefit.
- Getting good sleep: not shocking, and this one’s not exactly news. But what may be shocking is that 68% of centenarians reported consistently getting enough good-quality sleep. To put that into perspective, only 35% of 10almonds readers reported regularly getting sleep in the 7–9 hours range.
- Rural living environment: more than 75% of the centenarians and near-centenarians lived in rural areas. This is not usually something touted as a Blue Zones thing on lists of Blue zones things, but this review strongly highlighted it as very relevant. In the category of things that are more obvious once it’s pointed out, though, this isn’t necessarily such a difference between “country folk” and “city folk”, so much as the ability to regularly be in green spaces has well-established health benefits physically, mentally, and both combined (such as: neurologically).
And showing that yes, even parks in cities make a significant difference:
Want to know more?
You can read the study in full here:
A systematic review of diet and medication use among centenarians and near-centenarians worldwide
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Apples vs Figs – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apples to figs, we picked the figs.
Why?
These two fruits are both known for being quite rich in sugar (but also rich in fiber, which offsets it metabolically), and indeed their macros are quite similar. That said, figs have slightly more protein, fiber, and carbs. Both are considered low glycemic index foods. We can consider this category a tie, or perhaps a nominal win for apples, whose glycemic index is the lower of the two. But since figs’ GI is also low, it’s really not a deciding factor.
In terms of vitamins, apples have more of vitamins C and E, while figs have more of vitamins A, B1, B2, B3, B5, B6, B9, and choline, with noteworthy margins of difference. A clear for figs here.
When it comes to minerals, apples are not higher in any minerals, while figs are several times higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. An overwhelming win for figs.
Of course, enjoy either or both, but if you want nutritional density, apples simply cannot compete with figs.
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: