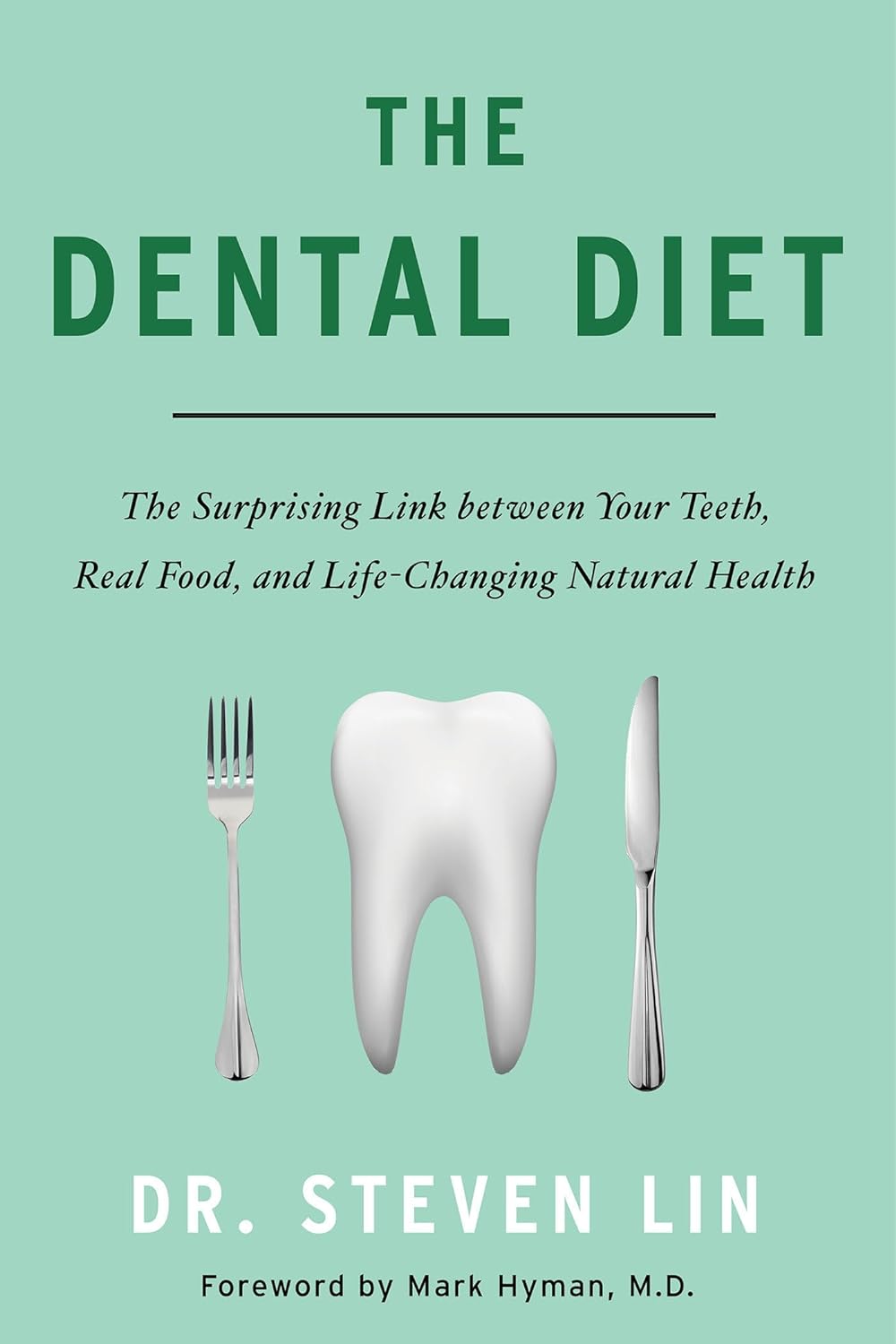
The Dental Diet – by Dr. Steven Lin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As it turns out, there’s a lot more to healthy teeth than skipping the sugar and getting some calcium.
The author’s journey started with the realization that most of his work as a dentist should be unnecessary, and not just in the “you should have been flossing” sense. Rather, he came to the same conclusions as his fellow dentist Weston Price before him, and this time (unlike Price) he stuck to his own field, dentistry—meaning that the conclusions he kept were the more valid ones.
Another thing he does better than Price is that he contextualizes the information—we don’t need, for example, to be eating seal fat as a main component of our diet, but we do need to be getting sufficient amounts of certain fat-soluble vitamins. And most people aren’t. Same with what’s good or bad for our oral microbiome, and by extension, our saliva, and by extension, our teeth and gums.
There’s a lot of nutritional information in here; macros and micronutrients alike, but the book goes further than that, to also recommend minimally-processed food that requires more chewing, for example. Not just for its nutritional content, but because that helps our teeth move to (and then stay) where they are ideally supposed to be. No amount of perfectly-blended nutritional supplement drink will align your maxilla for you, say. But chomping on raw carrots? Different story.
Dr. Lin offers a 40-day meal plan, but aware that if you’re vegetarian or vegan you’re probably going to have to rethink it yourself using the information he gives, because his meal plan includes animal products.
Bottom line: if you’d like to eat for better oral health (nutritionally, physically, and for your oral microbiome), this book has all the information you’ll need.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Resistance Beyond Weights
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Resistance, Your Way
We’ve talked before about the importance of resistance training:
Resistance Is Useful! (Especially As We Get Older)
And we’ve even talked about how to make resistance training more effective:
(High Intensity Interval Training, but make it High Intensity Resistance Training)
Which resistance training exercises are best?
There are two reasonable correct answers here:
- The resistance training exercises that you will actually do (because it’s no good knowing the best exercise ever if you’re not going to do it because it is in some way offputting to you)
- The resistance training exercises that will prevent you from getting a broken bone in the event of some accident or incident
This latter is interesting, because when people think resistance training, the usually immediate go-to exercises are often things like the bench press, or the chest machine in the gym.
But ask yourself: how often do we hear about some friend or relative who in their old age has broken their humerus?
It can happen, for sure, but it’s not as often as breaking a hip, a tarsal (ankle bones), or a carpal (wrist bones).
So, how can we train to make those bones strong?
Strong bones grow under strong muscles
When archaeologists dig up a skeleton from a thousand years ago, one of the occupations that’s easy to recognize is an archer. Why?
An archer has an unusual frequent exercise: pushing with their left arm while pulling with their right arm. This will strengthen different muscles on each side, and thus, increase bone density in different places on each arm. The left first metacarpal and right first and second metacarpals and phalanges are also a giveaway.
This is because: one cannot grow strong muscles on weak bones (or else the muscles would just break the bones), so training muscles will force the body to strengthen the relevant bones.
So: if you want strong bones, train the muscles attached to those bones
This answers the question of “how am I supposed to exercise my hips” etc.
Weights, bodyweight, resistance bands
If you go to the gym, there’s a machine for everything, and a member of gym staff will be able to advise which of their machines will strengthen which muscles.
If you train with free weights at home:
- Wrist curls (forearm supported and stationary, lifting a dumbbell in your hand, palm-upwards) will strengthen the wrist
- The farmer’s walk (carrying a heavy weight in each hand) will also strengthen your wrist
- A modified version of this involves holding the weight with just your fingertips, and then raising and lowering it by curling and uncurling your fingers)
- Lateral leg raises (you will need ankle-weights for this) will strengthen your ankles and your hips, as will hip abductions (as in today’s featured video), especially with a weight attached.
- Ankle raises (going up on your tip-toes and down again, repeat) while holding weights in your hands will strengthen your ankles
If you don’t like weights:
- Press-ups will strengthen your wrists
- Fingertip press-ups are even better: to do these, do your press-ups as normal, except that the only parts of your hands in contact with the ground are your fingertips
- This same exercise can be done the other way around, by doing pull-ups
- And that same “even better” works by doing pull-ups, but holding the bar only with one’s fingertips, and curling one’s fingers to raise oneself up
- Lateral leg raises and hip abductions can be done with a resistance band instead of with weights. The great thing about these is that whereas weights are a fixed weight, resistance bands will always provide the right amount of resistance (because if it’s too easy, you just raise your leg further until it becomes difficult again, since the resistance offered is proportional to how much tension the band is under).
Remember, resistance training is still resistance training even if “all” you’re resisting is gravity!
If it fells like work, then it’s working
As for the rest of preparing to get older?
Check out:
Training Mobility Ready For Later Life
Take care!
Share This Post
-
Instant Quiz Results, No Email Needed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
❓ Q&A With 10almonds Subscribers!
Q: I like that the quizzes (I’ve done two so far) give immediate results , with no “give us your email to get your results”. Thanks!
A: You’re welcome! That’s one of the factors that influences what things we include here! Our mission statement is “to make health and productivity crazy simple”, and the unwritten part of that is making sure to save your time and energy wherever we reasonably can!
Share This Post
-
The Hidden Risk of Stretching: Avoiding Hamstring Injuries in Yoga
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What is Yoga Butt
Have you ever experienced a mysterious pain while stretching, or perhaps during yoga? You might be dealing with “yoga butt,” a common—although rarely discussed—injury. In the below video, the Lovely Liv from Livinleggings shares her journey of discovering, and overcoming, “yoga butt”.
Dealing With Yoga Butt
Yoga butt, or proximal hamstring tendinopathy, occurs when the hamstrings are overstretched without adequate strengthening. Many yoga poses help stretch the hamstrings, but often don’t focus on strengthening said hamstrings; this imbalance is what can lead to damage over time.
To help prevent Yoga butt, it’s essential to balance stretching with strengthening. You can look into incorporating hamstring-strengthening exercises like Romanian deadlifts, hamstring curls, and modified yoga poses into your routine.
(If you’re new to strengthening exercises, we recommend reading Women’s Strength Training Anatomy Workouts or Strength Training for Seniors).
Watch the full video to learn more and hopefully protect yourself from long-term injuries:
Let us know your thoughts, and whether you have any other topics you’d like us to cover.
Share This Post
Related Posts
-
How to Fall Asleep Faster: CBT-Insomnia Treatment
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Insomnia affects a lot of people, and is even more common as we get older. Happily, therapist Emma McAdam is here with a drug-free solution that will work for most people most of the time.
Cognitive Behavioral Therapy for Insomnia (CBTI)
While people think of causes of insomnia as being things such as stress, anxiety, overthinking, disturbances, and so forth, these things affect sleep in the short term, but don’t directly cause chronic insomnia.
We say “directly”, because chronic insomnia is usually the result of the brain becoming accustomed to the above, and thus accidentally training itself to not sleep.
The remedy: cut the bad habit of staying in bed while awake. Lying in bed awake trains the brain to associate lying in bed with wakefulness (and any associated worrying, etc). In essence, we lie down, and the brain thinks “Aha, we know this one; this is the time and place for worrying, ok, let’s get to work”.
So instead: if you’re in bed and not asleep within 15 minutes, get up and do something non-stimulating until you feel sleepy, then return to bed. This may cause some short term tiredness, but it will usually correct the chronic insomnia within a week.
For more details, tips, and troubleshooting with regard to the above, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How to Fall Back Asleep After Waking Up in the Middle of the Night
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fluoride Toothpaste vs Non-Fluoride Toothpaste – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing fluoride toothpaste to non-fluoride toothpaste, we picked the fluoride.
Why?
Fluoride is indeed toxic; that’s why it’s in toothpaste (to kill things; namely, bacteria whose waste products would harm our teeth). However, we are much bigger than those bacteria.
Given the amount of fluoride in toothpaste (usually under 1mg per strip of toothpaste to cover a toothbrush head), the amount that people swallow unintentionally (about 1/20th of that, so about 0.1mg daily if brushing teeth twice daily), and the toxicity level of fluoride (32–64mg/kg), then even if we take the most dangerous ends of all those numbers (and an average body size), to suffer ill effects from fluoride due to brushing your teeth, would require that you brush your teeth more than 23,000 times per day.
Alternatively, if you were to ravenously eat the toothpaste instead of spitting it out, you’d only need to brush your teeth a little over 1,000 times per day.
All the same, please don’t eat toothpaste; that’s not the message here.
However! In head-to-head tests, fluoride toothpaste has almost always beaten non-fluoride toothpaste.
Almost? Yes, almost: hydroxyapatite performed equally in one study, but that’s not usually an option on as many supermarket shelves.
We found some on Amazon, though, which is the one we used for today’s head-to-head. Here it is:
However, before you rush to buy it, do be aware that the toxicity of hydroxyapatite appears to be about twice that of fluoride:
Scientific Committee on Consumer Safety Opinion On Hydroxyapatite (Nano)
…which is still very safe (you’d need to brush your teeth, and eat all the toothpaste, about 500 times per day, to get to toxic levels, if we run with the same numbers we discussed before. Again, please do not do that, though).
But, since the science so far suggests it’s about twice as toxic as fluoride, then regardless of that still being very safe, the fluoride is obviously (by the same metric) twice as safe, hence picking the fluoride.
Want more options?
Check out our previous main feature:
Less Common Oral Hygiene Options
(the above article also links back to our discussion of different toothpastes and mouthwashes, by the way)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
L-Theanine: What’s The Tea?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
L-Theanine: What’s The Tea?
We’ve touched previously on l-theanine, when this newsletter was new, and we had only a few hundred subscribers and the carefully organized format wasn’t yet what it is today.
So now it’s time to give this potent dietary compound / nutritional supplement the “Monday Research Review” treatment…
What is it?
L-theanine is an amino acid found in tea. The human body can’t produce it, and/but it’s not essential for humans. It does have a lot of benefits, though. See for example:
L-Theanine as a Functional Food Additive: Its Role in Disease Prevention and Health Promotion
How does it work?
L-theanine works by moderating and modulating the brain’s neurotransmitters.
This sounds fancy, but basically it means: it doesn’t actually add anything in the manner of a drug, but it changes how we use what we have naturally.
What does it do? Read on…
It increases mental focus
It has been believed that l-theanine requires the presence of caffeine to achieve this (i.e., it’s a combination-only effect). For example:
But as it turns out, when a group of researchers actually checked… This isn’t true, as Foxe et al. write:
❝We asked whether either compound alone, or both in combination, would affect performance of the task in terms of reduced error rates over time, and whether changes in alpha-band activity would show a relationship to such changes in performance. When treated with placebo, participants showed a rise in error rates, a pattern that is commonly observed with increasing time-on-task, whereas after caffeine and theanine ingestion, error rates were significantly reduced. The combined treatment did not confer any additional benefits over either compound alone, suggesting that the individual compounds may confer maximal benefits at the dosages employed❞
It promotes a calmly wakeful feeling of serenity
Those are not words typically found in biopharmaceutical literature, but they’re useful here to convey:
- L-theanine promotes relaxation without causing drowsiness
- L-theanine promotes mental alertness without being a stimulant
Here is where l-theanine really stands out from caffeine. If both substances promote mental focus, but one of them does it by making us “wired” and the other does it while simultaneously promoting calm, it makes the choice between them clearer!
Read more: L-theanine, a natural constituent in tea, and its effect on mental state
It relieves stress and anxiety
Building on from the above, but there’s more: l-theanine relieves stress and anxiety in people experiencing stressful situations, without any known harmful side effects… This is something that sets it apart from a lot of anxiolytic (antianxiety) drugs!
Here’s what a big systematic review of clinical trials had to say:
Theanine consumption, stress and anxiety in human clinical trials: A systematic review
L-theanine has other benefits too
We’ve talked about some of the most popular benefits of l-theanine, and we can’t make this newsletter too long, but research also suggests that it…
- Supports healthy weight management
- Reduces inflammation
- Supports immune health
- Helps fight cancer
- May extend lifespan ← this one’s a C. elegans study, but despite being a tiny worm, they actually function very similarly to humans on a cellular level; it’s why they’re used so much for anti-aging research
If you’re interested in this topic, we recommend also reading our previous article on l-theanine—pardon that we hadn’t really nailed down our style yet—but there’s a bunch of useful information about how l-theanine makes caffeine “better” in terms of benefits. We also talk dosage, and reference some other studies we didn’t have room to include today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: