Cabbage vs Cauliflower – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cabbage to cauliflower, we picked the cauliflower.
Why?
First, let’s note: these are two different cultivars of the same species (Brassica oleracea) and/but as usual (we say, as there are a lot of cultivars of Brassica oleracea, and we’ve done a fair few pairings of them before) there are still nutritional differences to consider, such as…
In terms of macros, cabbage has very slightly more carbs and fiber, while cauliflower has very slightly more protein. However, the numbers are all so close (and the glycemic index equal), such that we’re going to call the macros category a tie.
In the category of vitamins, cabbage has more of vitamins A, B1, E, and K, while cauliflower has more of vitamins B2, B3, B5, B6, B7, B9, C, and choline. Superficially, this is a clear 8:4 win for cauliflower; it’s worth noting though that the differences in amounts are mostly small, so this isn’t as big a win as it looks like. Still a win for cauliflower, though.
When it comes to minerals, it’s a similar story: cabbage has a little more calcium, iron, and manganese, while cauliflower has a little more copper, magnesium, phosphorus, potassium, and zinc. This time a 6:3 win for cauliflower, and again, the margins are small so there’s really not as much between them as it looks like. Still a win for cauliflower, though.
In short: enjoy either or both (diversity is good), but the most nutritionally dense is cauliflower, even if cabbage isn’t far behind it.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
100 Ways to Change Your Life – by Liz Moody
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sometimes we crave changing things up, just to feel something new. This can result in anything from bad haircut decisions or impulsive purchases, to crashing and burning-out of a job, project, or relationship. It doesn’t have to be that way, though!
This book brings us (as the title suggest) 100 evidence-based ways of changing things up in a good way—small things that can make a big difference in many areas of life.
In terms of format, these are presented in 100 tiny chapters, each approximately 2 pages long (obviously it depends on the edition, but you get the idea). Great to read in any of at least three ways:
- Cover-to-cover
- One per day for 100 days
- Look up what you need on an ad hoc basis
Bottom line: even if you already do half of these things, the other half will each compound your health happiness one-by-one as you add them. This is a very enjoyable and practical book!
Click here to check out 100 Ways to Change Your Life, and level-up yours!
Share This Post
-
Why 7 Hours Sleep Is Not Enough
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Sleep-Deprived Are You, Really?
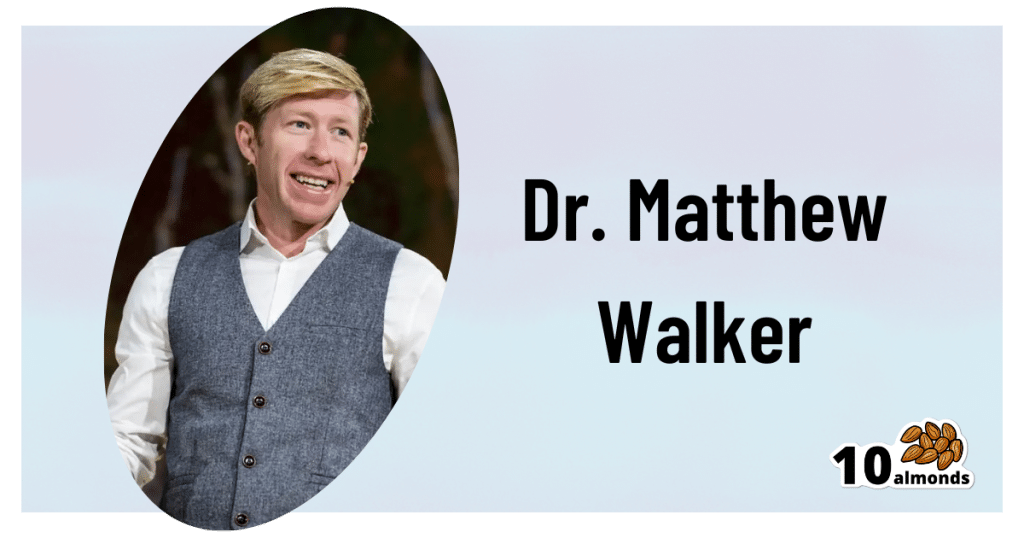
This is Dr. Matthew Walker. He’s a neuroscientist and sleep specialist, and is the Director of the Center for Human Sleep Science at UC Berkeley’s Department of Psychology. He’s also the author of the international bestseller “Why We Sleep”.
What does he want us to know?
Sleep deprivation is more serious than many people think it is. After about 16 hours without sleep, the brain begins to fail, and needs more than 7 hours of sleep to “reset” cognitive performance.
Note: note “seven or more”, but “more than seven”.
After ten days with only 7 hours sleep (per day), Dr. Walker points out, the brain is as dysfunctional as it would be after going without sleep for 24 hours.
Here’s the study that sparked a lot of Dr. Walker’s work:
Importantly, in Dr. Walker’s own words:
❝Three full nights of recovery sleep (i.e., more nights than a weekend) are insufficient to restore performance back to normal levels after a week of short sleeping❞
~ Dr. Matthew Walker
See also: Why You Probably Need More Sleep
Furthermore: the sleep-deprived mind is unaware of how sleep-deprived it is.
You know how a drunk person thinks they can drive safely? It’s like that.
You do not know how sleep-deprived you are, when you are sleep-deprived!
For example:
❝(60.7%) did not signal sleepiness before a sleep fragment occurred in at least one of the four MWT trials❞
Source: Sleepiness is not always perceived before falling asleep in healthy, sleep-deprived subjects
Sleep efficiency matters
With regard to the 7–9 hours band for optimal health, Dr. Walker points out that the sleep we’re getting is not always the sleep we think we’re getting:
❝Assuming you have a healthy sleep efficiency (85%), to sleep 9 hours in terms of duration (i.e. to be a long-sleeper), you would need to be consistently in bed for 10 hours and 36 minutes a night. ❞
~ Dr. Matthew Walker
At the bottom end of that, by the way, doing the same math: to get only the insufficient 7 hours sleep discussed earlier, a with a healthy 85% sleep efficiency, you’d need to be in bed for 8 hours and 14 minutes per night.
The unfortunate implication of this: if you are consistently in bed for 8 hours and 14 minutes (or under) per night, you are not getting enough sleep.
“But what if my sleep efficiency is higher than 85%?”
It shouldn’t be.If your sleep efficiency is higher than 85%, you are sleep-deprived and your body is having to enforce things.
Want to know what your sleep efficiency is?
We recommend knowing this, by the way, so you might want to check out:
Head-To-Head Comparison of Google and Apple’s Top Sleep-Monitoring Apps
(they will monitor your sleep and tell you your sleep efficiency, amongst other things)
Want to know more?
You might like his book:
Why We Sleep: Unlocking the Power of Sleep and Dreams
…and/or his podcast:
…and for those who like videos, here’s his (very informative) TED talk:
Prefer text? Click here to read the transcript
Want to watch it, but not right now? Bookmark it for later
Enjoy!
Share This Post
-
Running or yoga can help beat depression, research shows – even if exercise is the last thing you feel like
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At least one in ten people have depression at some point in their lives, with some estimates closer to one in four. It’s one of the worst things for someone’s wellbeing – worse than debt, divorce or diabetes.
One in seven Australians take antidepressants. Psychologists are in high demand. Still, only half of people with depression in high-income countries get treatment.
Our new research shows that exercise should be considered alongside therapy and antidepressants. It can be just as impactful in treating depression as therapy, but it matters what type of exercise you do and how you do it.
Walk, run, lift, or dance away depression
We found 218 randomised trials on exercise for depression, with 14,170 participants. We analysed them using a method called a network meta-analysis. This allowed us to see how different types of exercise compared, instead of lumping all types together.
We found walking, running, strength training, yoga and mixed aerobic exercise were about as effective as cognitive behaviour therapy – one of the gold-standard treatments for depression. The effects of dancing were also powerful. However, this came from analysing just five studies, mostly involving young women. Other exercise types had more evidence to back them.
Walking, running, strength training, yoga and mixed aerobic exercise seemed more effective than antidepressant medication alone, and were about as effective as exercise alongside antidepressants.
But of these exercises, people were most likely to stick with strength training and yoga.
Antidepressants certainly help some people. And of course, anyone getting treatment for depression should talk to their doctor before changing what they are doing.
Still, our evidence shows that if you have depression, you should get a psychologist and an exercise plan, whether or not you’re taking antidepressants.
Join a program and go hard (with support)
Before we analysed the data, we thought people with depression might need to “ease into it” with generic advice, such as “some physical activity is better than doing none.”
But we found it was far better to have a clear program that aimed to push you, at least a little. Programs with clear structure worked better, compared with those that gave people lots of freedom. Exercising by yourself might also make it hard to set the bar at the right level, given low self-esteem is a symptom of depression.
We also found it didn’t matter how much people exercised, in terms of sessions or minutes a week. It also didn’t really matter how long the exercise program lasted. What mattered was the intensity of the exercise: the higher the intensity, the better the results.
Yes, it’s hard to keep motivated
We should exercise caution in interpreting the findings. Unlike drug trials, participants in exercise trials know which “treatment” they’ve been randomised to receive, so this may skew the results.
Many people with depression have physical, psychological or social barriers to participating in formal exercise programs. And getting support to exercise isn’t free.
We also still don’t know the best way to stay motivated to exercise, which can be even harder if you have depression.
Our study tried to find out whether things like setting exercise goals helped, but we couldn’t get a clear result.
Other reviews found it’s important to have a clear action plan (for example, putting exercise in your calendar) and to track your progress (for example, using an app or smartwatch). But predicting which of these interventions work is notoriously difficult.
A 2021 mega-study of more than 60,000 gym-goers found experts struggled to predict which strategies might get people into the gym more often. Even making workouts fun didn’t seem to motivate people. However, listening to audiobooks while exercising helped a lot, which no experts predicted.
Still, we can be confident that people benefit from personalised support and accountability. The support helps overcome the hurdles they’re sure to hit. The accountability keeps people going even when their brains are telling them to avoid it.
So, when starting out, it seems wise to avoid going it alone. Instead:
- join a fitness group or yoga studio
get a trainer or an exercise physiologist
- ask a friend or family member to go for a walk with you.
Taking a few steps towards getting that support makes it more likely you’ll keep exercising.
Let’s make this official
Some countries see exercise as a backup plan for treating depression. For example, the American Psychological Association only conditionally recommends exercise as a “complementary and alternative treatment” when “psychotherapy or pharmacotherapy is either ineffective or unacceptable”.
Based on our research, this recommendation is withholding a potent treatment from many people who need it.
In contrast, The Royal Australian and New Zealand College of Psychiatrists recommends vigorous aerobic activity at least two to three times a week for all people with depression.
Given how common depression is, and the number failing to receive care, other countries should follow suit and recommend exercise alongside front-line treatments for depression.
I would like to acknowledge my colleagues Taren Sanders, Chris Lonsdale and the rest of the coauthors of the paper on which this article is based.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Michael Noetel, Senior Lecturer in Psychology, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
The Food Additive You Do Want
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Q: When Is A Fiber Not A Fiber?
A: when it’s a resistant starch. What’s it resistant to? Digestion. So, it functions as though a fiber, and by some systems, may get classified as such.
It’s a little like how sucralose is technically a sugar, but the body processes it like a fiber (but beware, because the sweetness of this disaccharide alone can trigger an insulin response anyway—dose dependent)
There may be other problems too:
But today’s not about sucralose, it’s about…
Guar gum’s surprising dietary role
You may have noticed “guar gum” on the list of ingredients of all kinds of things from baked goods to dairy products to condiments to confectionary and more.
It’s also used in cosmetics and explosives, but let’s not focus on that.
It’s used in food products as…
- a bulking agent
- a thickener
- a stabilizer
Our attention was caught by a new study, that found:
Resistant starch intake facilitates weight loss in humans by reshaping the gut microbiota
Often people think of “fiber helps weight loss” as “well yes, if you are bulking out your food with sawdust, you will eat less”, but it’s not that.
There’s an actual physiological process going on here!
We can’t digest it, but our gut microbiota can and will ferment it. See also:
Fiber against pounds: Resistant starch found to support weight loss
Beyond weight loss
Not everyone wants to lose weight, and even where weight loss is a goal, it’s usually not the only goal. As it turns out, adding guar gum into our diet does more things too:
Resistant starch supplement found to reduce liver triglycerides in people with fatty liver disease
(specifically, this was about NAFLD, non-alcoholic fatty liver disease)
Digging a little, it seems the benefits don’t stop there either:
Diet high in guar gum fiber limits inflammation and delays multiple sclerosis symptoms
(this one was a rodent study, but still, it’s promising and it’s consistent with what one would expect based on what else we know about its function in diet)
Should we just eat foods with guar gum in as an additive?
That depends on what they are, but watch out for the other additives if you do!
You can just buy guar gum by itself, by the way (here’s an example product on Amazon).
It’s doubtlessly no fun to take as a supplement (we haven’t tried this one), but it can be baked into bread, if baking’s your thing, or just used as a thickener in recipes where ordinarily you might use cornstarch or something else.
Can I get similar benefits from other foods?
The relevant quality is also present in resistant starches in general, so you might want to check out these foods, for example:
9 Foods That Are High in Resistant Starch
You can also check out ways to increase your fiber intake in general:
Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A Peek Behind The 10almonds Curtain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At 10almonds we give a lot of health information, so you may wonder: how much do we (the 10almonds team) put into practice? Is it even possible to do all these things? Do we have an 80:20 rule going on?
So, here’s what someone who thinks, reads, and writes about health all day, does for her health—and how it ties in with what you read here at 10almonds.
Hi, it’s me, a member of the 10almonds team and regular writer here, and I’m going to do the rest of this article in the first-person, since it’s using me as an example!
(PS: yes, the thumbnail is a digital impression of my appearance, though I would correct it that my hair is much longer, and my eyes are more gray; I must admit though it captured my smile, not to mention my collarbones-that-you-could-sit-on)
Dietary habits
Before we get to foods, let’s talk intermittent fasting. I practise 16:8 intermittent fasting… Approximately. That is to say, I’m mostly not religious about it, but I will generally breakfast around 12 noon, and have finished eating dinner before 8pm, with no food outside of those hours.
See also: Intermittent Fasting: What’s the truth?
Importantly, while I feel free to be a little flexible around start and finish times, I do very consciously decide “I am now fasting” and “I will now break the fast”.
Note my imperfection: it would be ideal to have the eating period earlier in the day, and have a bigger breakfast and small dinner. However, that doesn’t really work for me (leisurely evening meal is an important daily event in this household), so this is how I do it instead.
Foods!
It gets an exclamation mark because a thing about me is that I do love foods.
Breakfast: a typical breakfast for me these past months is a couple of ounces of mixed nuts with about 1oz of goji berries.
The mixed nuts are in equal proportions: almonds, walnuts, hazelnuts, cashews. Why those four? Simple, it’s because that’s what Aldi sells as “mixed nuts” and they are the cheapest nuts around, as well as containing absolute nutritional heavyweights almonds and walnuts in generous portions.
Often, but not always, I’ll have some dates with it, or dried apricots, or prunes.
I go through phases; sometimes I’ll enjoy overnight oats as my breakfast for a month or two at a time. I really just follow my gut in this regard.
See for example: Spiced Pear & Pecan Polyphenol Porridge
Lunch: I don’t really lunch per se, but between breakfast and dinner I’ll usually snack on a 3–5 organic carrots (I literally just cut the tops off and otherwise eat them like Bugs Bunny—peeling them would be extra work just to lose fiber). Note my imperfection: I don’t buy all of my vegetables organic, but I do for the ones where it makes the biggest difference.
If I’m feeling like it, I may lunch on a selection of herbs sabzi khordan style (see: Invigorating Sabzi Khordan), though I’m vegan so for simplicity I just skip the cheeses that are also traditional with that dish. On the other hand, for protein and fat I’ll usually add a cup of beans (usually black beans or kidney beans), seasoned with garlic and black pepper in an olive oil and balsamic vinegar dressing (that I make myself, so it’s just those ingredients). See also: Kidney Beans vs Black Beans – Which Is Healthier?
Dinner: this is my main sit-down meal of the day, and it’s enjoyed in a leisurely fashion (say, 40 minutes average with a normal distribution bell curve running between 20 and 60 minutes) with my son who lives with me. I mention all of this, because of the importance of relaxed mindful eating. In the instances of it being nearer the 20 minutes end, it’s not because of rushing, but rather because of a lighter meal some days.
See also: How To Get More Nutrition From The Same Food
Regular recurrences in the menu include:
I’ll often snack on something probiotic (e.g. kimchi) while I’m cooking.
See also: Make Friends With Your Gut! (You Can Thank Us Later)
In terms of what’s not in my diet: as mentioned, I’m vegan, so animal products are out. I don’t drink alcohol or use other recreational drugs, and I mostly drink decaffeinated coffee, but I’ll have a caffeinated one if I’m out somewhere. I’m not a puritan when it comes to sugar, but also, I simply don’t like it and I know well its health effects, so it doesn’t really form part of my diet except insofar as it’s in some ready-made condiments I may sometimes use (e.g. sriracha, teriyaki sauce). I’m also not a puritan when it comes to wheat, but it’s not something I consume daily. Usually on a weekly basis I’ll have a wholegrain pasta dish, and a dish with some kind of wholegrain flatbread.
See also:
Exercise!
First, some things that are lifestyle factors:
- I do not own a car, and I dislike riding in cars, buses, etc. So, I walk everywhere, unless it’s far enough that I must take the train, and even then I usually stand between carriages rather than sitting down.
- I have a standing desk setup, that hasn’t been lowered even once since I got it. I highly recommend it, as someone who spends a lot of time at my desk.
- You may imagine that I spend a lot of time reading; if it’s books (as opposed to scientific papers etc, which I read at my desk), then I’ll most of the time read them while perched like a gargoyle in a sitting squat (Slav squat, Asian squat, resting squat, deep squat, etc) on a balance ball. Yes, it is comfortable once you’re used to it!
About that latter, see also: The Most Anti Aging Exercise
In terms of “actual” exercise, I get 150–300 minutes “moderate exercise” per week, which is mostly composed of:
- Most days I walk into town to get groceries; it’s a 40-minute round trip on foot
- On days I don’t do that, even if I do walk to a more local shop, I spend at least 20 minutes on my treadmill.
See also: The Doctor Who Wants Us To Exercise Less, & Move More
Strength and mobility training, for me, comes mostly in what has been called “exercise snacking”, that is to say, I intersperse my working day with brief breaks to do Pilates exercises. I have theme days (lower body, core, upper body) and on average one rest day (from Pilates exercises) per week, though honestly, that’s usually more likely because of time constraints than anything else, because a deadline is looming.
See also: Four Habits That Drastically Improve Mobility
You may be wondering about HIIT: when I’m feeling extra-serious about it, I use my exercise bike for this, but I’ll be honest, I don’t love the bike, so on a daily basis, I’m much more likely to do HIIT by blasting out a hundred or so Hindu squats, resting, and repeating.
See also: How To Do HIIT (Without Wrecking Your Body)
Supplements
First I’ll mention, I do have HRT, of which the hormones I have are bioidentical estradiol gel in the morning, and a progesterone pessary in the evening. They may not be for everybody, but they’ve made a world of difference to me.
See also: HRT: A Tale Of Two Approaches
In terms of what one usually means when one says supplements, many I use intermittently (which is good in some cases, as otherwise the body may stop using them so well, or other problems can arise), but regular features include:
- Magnesium glycinate, malate, & citrate (See: Which Magnesium? (And: When?))
- Active vitamers of vitamins B9 and B12 (See: Which B Vitamins? It Makes A Difference!)
- Liposomal vitamin C (I actually get enough for general purposes in my diet, but as a vegan I don’t get dietary collagen, so this helps collagen synthesis)
- L-theanine (bedtime only) (See: L-Theanine: What’s The Tea?)
- Lion’s mane mushroom (See: What does lion’s mane mushroom actually do, anyway?)
- Quercetin (See: Fight Inflammation & Protect Your Brain, With Quercetin)
- Fisetin (weekends only) (See: Fisetin: The Anti-Aging Assassin)
Why weekends only for Fisetin? See: The Drug & Supplement Combo That Reverses Aging ← the supplement is fisetin, which outperforms quercetin in this role, and/but it only needs be taken for two days every two weeks, as a sort of “clearing out” of senescent cells. There is no need to take it every day, because if you just cleared out your senescent cells, then guess what, they’re not there now. Also, while sensescent cells are a major cause of aging, on a lower level they do have some anti-tumor effects, so it can be good to let some live a least for a while now and again. In short, cellular sensescence can help prevent tumors on a daily level, but it doesn’t hurt that capacity to have a clearing-out every couple of weeks; so says the science (linked above). Note my imperfection: I take it at weekends instead of for two days every two weeks (as is standard in studies, like those linked above), because it is simpler than remembering to count the weeks.
Cognitive exercise
Lest we forget, exercising our mind is also important! In my case:
- I’m blessed to have work that’s quite cognitively stimulating; our topics here at 10almonds are interesting. If it weren’t for that, I’d still be reading and writing a lot.
- I play chess, though these days I don’t play competitively anymore, and play rather for the social aspect, but this too is important in avoiding cognitive decline.
- I am one of those people who compulsively learns languages, and uses them a lot. This is very beneficial, as language ability is maintained in a few small areas of the brain, and it’s very much “use it or lose it”. Now, while I may not need my French or Russian or Arabic to keep the lights on in this part of the brain or that, the fact that I am pushing my limits every day is the important part. It’s not about how much I know—it’s about how much I engage those parts of my brain on a daily basis. Thus, even if you speak only one language right now, learning even just one more, and learning even only a little bit, you will gain the brain benefits—because you’re engaging it regularly in a new way, and that forces the brain to wire new synapses and also to maintain volume in those parts.
See also: How To Reduce Your Alzheimer’s Risk
And about language-learning specifically: An Underrated Tool Against Alzheimer’s ←this also shows how you don’t have to be extreme about language learning like I admittedly am.
How’s all this working out for me?
I can say: it works! My general health is better now than it was decades ago. I’ve personally focused a lot on reducing inflammation, and that really pays dividends when it comes to the rest of health. I didn’t talk about it above, but focusing on my sleep regularity and quality has helped a lot too.
In terms of measurable results, I recently had a general wellness checkup done by means of a comprehensive panel of 14 blood tests, and various physical metrics (BMI, body fat %, blood pressure, etc), and per those, I could not be in better health; it was as though I had cheated and written in all the best answers. I say this not to brag (you don’t know me, after all), but rather to say: it can be done!
Even without extreme resources, and without an abundance of free time, etc, it can be done!
Caveat: if you have some currently incurable chronic disease, there may be some limits. For example, if you have Type 1 Diabetes, probably your HbA1c* is going to be a little off even if you do everything right.
*HbA1c = glycated hemoglobin, a very accurate measure of what your blood glucose has been on average for the past 2–3 months—why 2–3 months? Because that’s the approximate lifespan of a red blood cell, and we’re measuring how much hemoglobin (in the red blood cells) has been glycated (because of blood glucose).
In summary
The stuff we write about at 10almonds can be implemented, on a modest budget and while juggling responsibilities (work, family, classes, etc).
I’m not saying that my lifestyle should be everyone’s template, but it’s at least an example of one that can work.
- Maybe you hate walking and love swimming.
- Maybe you have no wish to give up fish and eggs, say (both of which are fine/good in moderation healthwise).
- Maybe you have different priorities with supplements.
- Maybe you find language-learning uninteresting but take singing lessons.
- And so on.
In the absolute fewest words, the real template is:
- Decide your health priorities (what matters most for you)
- Look them up on 10almonds
- Put the things into action in a way that works for you!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Kitchen Doctor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
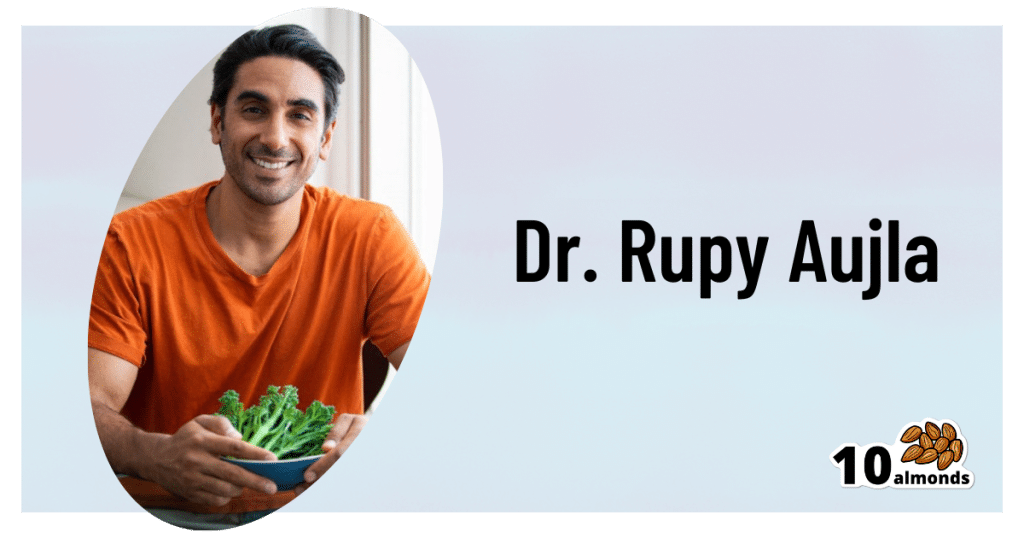
Dr. Rupy Aujla: The Kitchen Doctor
This is Dr. Rupy Aujla, and he’s a medical doctor. He didn’t set out to become a “health influencer”.
But then, a significant heart condition changed his life. Having a stronger motivation to learn more about nutritional medicine, he did a deep dive into the scientific literature, because that’s what you do when your life is on the line, especially if you’re a doctor!
Using what he learned, he was able to reverse his condition using a food and lifestyle approach. Now, he devotes himself to sharing what he learned—and what he continues to learn as he goes along.
One important thing he learned because of what happened to him, was that he hadn’t been paying enough attention to what his body was trying to tell him.
He wants us to know about interoception—which isn’t a Chris Nolan movie. Rather, interoception is the sense of what is going on inside one’s own body.
The counterpart of this is exteroception: our ability to perceive the outside world by means of our various senses.
Interoception is still using the senses, but is sensing internal body sensations. Effectively, the brain interprets and integrates what happens in our organs.
When interoception goes wrong, researchers found, it can lead to a greater likelihood of mental health problems. Having an anxiety disorder, depression, mood disorder, or an eating disorder often comes with difficulties in sensing what is going on inside the body.
Improving our awareness of body cues
Those same researchers suggested therapies and strategies aimed at improving awareness of mind-body connections. For example, mindfulness-based stress reduction, yoga, meditation and movement-based treatments. They could improve awareness of body cues by attending to sensations of breathing, cognitions and other body states.
But where Dr. Aujla puts his focus is “the heart of the home”, the kitchen.
The pleasure of food
❝Eating is not simply ingesting a mixture of nutrients. Otherwise, we would all be eating astronaut food. But food is not only a tool for health. It’s also an important pleasure in life, allowing us to connect to others, the present moment and nature.❞
Dr. Rupy Aujla
Dr. Aujla wants to help shift any idea of a separation between health and pleasure, because he believes in food as a positive route to well-being, joy and health. For him, it starts with self-awareness and acceptance of the sensory pleasures of eating and nourishing our bodies, instead of focusing externally on avoiding perceived temptations.
Most importantly:
We can use the pleasure of food as an ally to healthy eating.
Instead of spending our time and energy fighting the urge to eat unhealthy things that may present a “quick fix” to some cravings but aren’t what our body actually wants, needs, Dr. Aujla advises us to pay just a little more attention, to make sure the body’s real needs are met.
His top tips for such are:
- Create an enjoyable relaxing eating environment
To help cultivate positive emotions around food and signal to the nervous system a shift to food-processing time. Try setting the table with nothing else on it beyond what’s relevant to the dinner, putting away distractions, using your favorite plates, tablecloth, etc.
- Take 3 deep abdominal breaths before eating
To help you relax and ground yourself in the present moment, which in turn is to prepare your digestive system to receive and digest food.
- Pay attention to the way you sit
Take some time to sit comfortably with your feet grounded on the floor, not slouching, to give your stomach space to digest the food.
- Appreciate what it took to bring this food to your plate
Who was involved in the growing process and production, the weather and soil it took to grow the food, and where in the world it came from.
- Enjoy the sensations
When you’re cooking, serving, and eating your food, be attentive to color, texture, aroma and even sound. Taste the individual ingredients and seasonings along the way, when safe and convenient to do so.
- Journal
If you like journaling, you can try adding a mindful eating section to that. Ask questions such as: “how did I feel before, during, and after the meal?”
In closing…
Remember that this is a process, not only on an individual level but as a society too.
Oftentimes it’s hard to eat healthily… We can be given to wonder even “what is healthy, after all?”, and we can be limited by what is available, what is affordable, and what we have time to prepare.
But if we make a conscious commitment to make the best choices we reasonably can as we go along, then small changes can soon add up.
Interested in what kind of recipes Dr. Aujla goes for?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: