Dancing vs Parkinson’s Depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a fun study, and the results are/were very predictable, and/but not necessarily something that people might think of in advance. First, let’s look at how some things work:
Parkinson’s disease & depression
Parkinson’s disease is a degenerative neurological disease that, amongst other things, is characterized by low dopamine levels.
For the general signs and symptoms, see: Recognize The Early Symptoms Of Parkinson’s Disease
Dopamine is the neurotransmitter responsible for feelings of reward, is involved in our language faculties and the capacity to form plans (even simple plans such as “make a cup of coffee”) as well as being critical for motor functions.
See also: Neurotransmitter Cheatsheet ← for demystifying some of “what does what” for commonly-conflated chemicals
You can see, therefore, why Parkinson’s disease will often have depression as a comorbidity—there may be influencing social factors as well (many Parkinson’s disease sufferers are quite socially isolated, which certainly does not help), but a clear neurochemical factor that we can point to is “a person with low dopamine levels will feel joyless, bored, and unmotivated”.
Let movement be thy medicine
Parkinson’s disease medications, therefore, tend to involve increasing dopamine levels and/or the brain’s ability to use dopamine.
Antidepressant medications, however, are more commonly focused on serotonin, as serotonin is another neurotransmitter associated with happiness—it’s the one we get when we look at open green spaces with occasional trees and a blue sky ← we get it in other ways too, but for evolutionary reasons, it seems our brains still yearn the most for landscapes that look like the Serengeti, even if we have never even been there personally.
There are other kinds of antidepressants too, and (because depression can have different causes) what works for one person won’t necessarily work for another. See: Antidepressants: Personalization Is Key!
In the case of Parkinson’s disease, because the associated depression is mostly dopamine-related, those green spaces and blue skies and SSRIs won’t help much. But you know what does?
Dance!
A recent (published last month, at time of writing) study by Dr. Karolina Bearss et al. did an interventional study that found that dance classes significantly improved both subjective experience of depression, and objective brain markers of depression, across people with (68%) and without (32%) Parkinson’s disease.
The paper is quite short and it has diagrams, and discusses the longer-term effect as well as the per-session effect:
Dance is thought to have a double-effect, improving both cognitive factors and motor control factors, for obvious reasons, and all related to dopamine response (dancing is an activity we are hardwired to find rewarding*, plus it is exercise which also triggers various chemicals to be made, plus it is social, which also improves many mental health factors).
*You may have heard the expression that “dancing is a vertical expression of a horizontal desire”, and while that may not be true for everyone on an individual level, on a species level it is a very reasonable hypothesis for why we do it and why it is the way it is.
Want to learn more?
We wrote previously about battling depression (of any kind) here:
The Mental Health First-Aid That You’ll Hopefully Never Need
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sleep wrinkles are real. Here’s how they leave their mark
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You wake up, stagger to the bathroom and gaze into the mirror. No, you’re not imagining it. You’ve developed face wrinkles overnight. They’re sleep wrinkles.
Sleep wrinkles are temporary. But as your skin loses its elasticity as you age, they can set in.
Here’s what you can do to minimise the chance of them forming in the first place.
How side-sleeping affects your face
Your skin wrinkles for a number of reasons, including ageing, sun damage, smoking, poor hydration, habitual facial expressions (such as grinning, pouting, frowning, squinting) and sleeping positions.
When you sleep on your side or stomach, your face skin is squeezed and crushed a lot more than if you sleep on your back. When you sleep on your side or stomach, gravity presses your face against the pillow. Your face skin is distorted as your skin is stretched, compressed and pulled in all directions as you move about in your sleep.
You can reduce these external forces acting on the face by sleeping on your back or changing positions frequently.
Doctors can tell which side you sleep on by looking at your face
In a young face, sleep wrinkles are transient and disappear after waking.
Temporary sleep wrinkles can become persistent with time and repetition. As we age, our skin loses elasticity (recoil) and extensibility (stretch), creating ideal conditions for sleep wrinkles or lines to set in and last longer.
The time spent in each sleeping position, the magnitude of external forces applied to each area of the face, as well as the surface area of contact with the pillow surface, also affects the pattern and rate of sleep wrinkle formation.
Skin specialists can often recognise this. People who favour sleeping on one side of their body tend to have a flatter face on their sleeping side and more visible sleep lines.
Can a night skincare routine avoid sleep wrinkles?
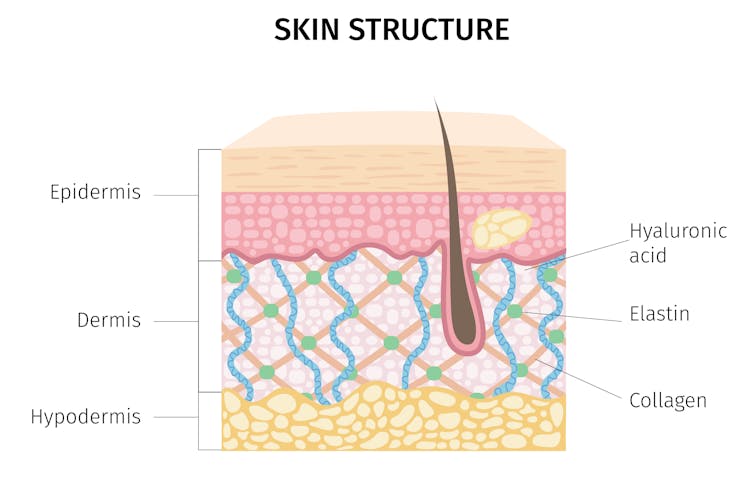
Collagen and elastin are two primary components of the dermis (inner layer) of skin. They form the skin structure and maintain the elasticity of skin.
The dermis is the inner layer of skin. mermaid3/Shutterstock Supplementing collagen through skincare routines to enhance skin elasticity can help reduce wrinkle formation.
Hyaluronic acid is a naturally occurring molecule in human bodies. It holds our skin’s collagen and elastin in a proper configuration, stimulates the production of collagen and adds hydration, which can help slow down wrinkle formation. Hyaluronic acid is one of the most common active ingredients in skincare creams, gels and lotions.
Moisturisers can hydrate the skin in different ways. “Occlusive” substances produce a thin layer of oil on the skin that prevents water loss due to evaporation. “Humectants” attract and hold water in the skin, and they can differ in their capacity to bind with water, which influences the degree of skin hydration.
Do silk pillowcases actually make a difference?
Can they help? New Africa/Shutterstock Silk pillowcases can make a difference in wrinkle formation, if they let your skin glide and move, rather than adding friction and pressure on a single spot. If you can, use silk sheets and silk pillows.
Studies have also shown pillows designed to reduce mechanical stress during sleep can prevent skin deformations. Such a pillow could be useful in slowing down and preventing the formation of certain facial wrinkles.
Sleeping on your back can reduce the risk of sleep lines, as can a nighttime routine of moisturising before sleep.
Otherwise, lifestyle choices and habits, such quitting smoking, drinking plenty of water, a healthy diet (eating enough vegetables, fruits, nuts, seeds, healthy fats, yogurt and other fermented foods) and regular use of sunscreens can help improve the appearance of the skin on our face.
Yousuf Mohammed, Dermatology researcher, The University of Queensland; Khanh Phan, Postdoctoral Research Fellow, Frazer Institute, The University of Queensland, and Vania Rodrigues Leite E. Silva, Honorary Associate Professor, Frazer Institute, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Collard Greens vs Watercress – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing collard greens to watercress, we picked the collard greens.
Why?
It was close! But…
In terms of macros, collard greens have 8x the fiber, 4x the carbs, and slightly more protein. The fiber-to-carbs ratio also gives collard greens the lower glycemic index, although honestly, nobody is getting metabolic disease from eating watercress. Still, by the numbers it’s a clear win for collard greens, and especially 8x the fiber is not to be undervalued!
When it comes to vitamins, things were much more even; collard greens have more of vitamins A, B3, B9, K, and choline, while watercress has more of vitamins B1, B2, B5, C, and E. They’re tied on vitamin B6, so that makes a 5.5:5.5 tie overall. Looking for a tiebreaker, collard greens’ margins of difference are greater, so we could call this a tie or the narrowest of wins for collard greens ion this category.
In the category of minerals, collard greens have more calcium, copper, iron, manganese, and zinc, while watercress has more copper, phosphorus, potassium, and selenium. They’re tied on magnesium. This time the margins of difference are also comparable, so there’s really no tiebreaker available for this one. Thus, an absolute tie on minerals.
Looking at polyphenols, watercress has slightly more, with the main contender being 4mg/100g quercetin.
Adding up the sections results in either a tie or a slight for collard greens based on the tiebreaker in the vitamins category.
We can also put the two clear wins (one for collard greens and one for watercress), and say that in our opinion, collard greens’ 4g/100g fiber beats watercress’s 4mg/100g quercetin.
Quercetin is great and all, but:
- if you buy a quercetin supplement like this one on Amazon it’s 1000mg capsules, so how critical is watercress’s 4mg, really? Yes, getting it from food is better, but it’s not 25,000% better.
- no doctor that we know of is saying “you need more quercetin or you’re going to die”, but they do say “you need more fiber or you’re going to die”
- indeed, the WHO passionately proclaims that 95% of people in the US especially desperately need to eat more fiber, whereas there is no similar giant public health campaign begging people to have 4mg more of quercetin
…so we’ll say that’s another tiebreaker in favor of collard greens.
In short: collard greens scrape a win based on several tiebreakers, but watercress was a very close contender indeed!
Of course, by all means enjoy either or (ideally!) both; diversity is good.
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
-
Cranberries vs Goji Berries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cranberries to goji berries, we picked the cranberries.
Why?
Both are great! And your priorities may differ. Here’s how they stack up:
In terms of macros, goji berries have more protein, carbs, and fiber. This is consistent with them generally being eaten very dried, whereas cranberries are more often eaten fresh or from frozen, or partially rehydrated. In any case, goji berries are the “more food per food” option, so it wins this category. The glycemic indices are both low, by the way, though goji berries are the lower.
When it comes to vitamins, cranberries have more of vitamins B1, B2, B3, B5, B6, B9, E, K, and choline, while goji berries have more of vitamins A and C. Admittedly it’s a lot more, but still, on strength of overall vitamin coverage, the clear winner here is cranberries.
We see a similar story when it comes to minerals: cranberries have more copper, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while goji berries have (a lot) more calcium and iron. Again, by strength of overall mineral coverage, the clear winner here is cranberries.
Cranberries do also have some extra phytochemical benefits, including their prevention/cure status when it comes to UTIs—see our link below for more on that.
At any rate, enjoy either or both, but those are the strengths and weaknesses of these two berries!
Want to learn more?
You might like to read:
- Health Benefits Of Cranberries (But: You’d Better Watch Out)
- Goji Berries: Which Benefits Do They Really Have?
- The Sugary Food That Lowers Blood Sugars ← this is also about goji berries
Take care!
Share This Post
Related Posts
-
Natto vs Tofu – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing nattō to tofu, we picked the nattō.
Why?
In other words, in the comparison of fermented soy to fermented soy, we picked the fermented soy. But the relevant difference here is that nattō is fermented whole soybeans, while tofu is fermented soy milk of which the coagulated curds are then compressed into a block—meaning that the nattō is the one that has “more food per food”.
Looking at the macros, it’s therefore no surprise that nattō has a lot more fiber to go with its higher carb count; it also has slightly more protein. You may be wondering what tofu has more of, and the answer is: water.
In terms of vitamins, nattō has more of vitamins B2, B4, B6, C, E, K, and choline, while tofu has more of vitamins A, B3, and B9. So, a 7:3 win for nattō, even before considering that that vitamin C content of nattō is 65x more than what tofu has.
When it comes to minerals, nattō has more copper, iron, magnesium, manganese, potassium, and zinc, while tofu has more calcium, phosphorus, and selenium. So, a 6:3 win for nattō, and yes, the margins of difference are comparable (being 2–3x more for most of these minerals).
In short, both of these foods are great, but nattō is better.
Want to learn more?
You might like to read:
21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cannabis & Heart Attacks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For many, cannabis use has taken the place that alcohol used to have when it comes to wanting a “downer”, that is to say, a drug that relaxes us as opposed to stimulating us.
Indeed, it is generally considered safer than alcohol ← however this is not a strong claim, because alcohol is much more dangerous than one would think given its ubiquity and (in many places, at least) social acceptability.
We’ve talked a bit about cannabis use before, in its various forms, for example:
Cannabis Myths vs Reality ← a very good starting point for the curious
And one specifically about the use of THC gummies (THC is the psychoactive compound in cannabis, i.e. it’s the chemical that gets people high, as opposed to CBD, which is not psychoactive) as a sleep aid:
Sweet Dreams Are Made of THC (Or Are They?)
And for those skipping the THC, we’ve also written about CBD use, including:
CBD Oil: What Does The Science Say? and Do CBD Gummies Work?
So, about cannabis and heart attacks
Alcohol is a relaxant, and yet it can contribute to heart disease (amongst many other things, of course):
Can We Drink To Good Health? ← this is mostly about red wine’s putative heart health benefits, how the idea got popularized, and how it doesn’t stand up to scrutiny when actually looking at the evidence.
And cannabis, another relaxant? Not so good either!
New research has shown that cannabis users have a higher risk of heart attacks, even among younger and otherwise healthy individuals. This is based on analyzing data from 4,636,628 relatively healthy adults.
Specifically, the data showed that even young healthy cannabis users get:
- Sixfold increased risk of heart attack
- Fourfold increased risk of ischemic stroke
- Threefold increased risk of cardiovascular death, heart attack, or stroke
We mention the otherwise “relatively healthy” nature of the participants, because it’s important to note that less healthy people (who were perhaps using cannabis to self-medicate for some serious condition) were not included in the dataset, as it’d skew the data unhelpfully and it’d make the risk look a lot higher than the risk levels we mentioned above.
The mechanisms by which cannabis affects heart health are not fully understood, but hypotheses include:
- Disrupting heart rhythm regulation
- Increasing oxygen demand in the heart muscle
- Causing endothelial dysfunction, which affects blood vessel function
Further, heart attack risk peaked one hour after cannabis use, and while this doesn’t prove causality, it certainly doesn’t make cannabis look safe.
You can read the paper in its entirety here:
Want a safer way to relax?
We recommend:
- No-Frills, Evidence-Based Mindfulness
- Meditation Games That You’ll Actually Enjoy
- Which Style Of Yoga Is Best For You?
- 7 Kinds Of Rest When Sleep Is Not Enough
- Better Sex = Longer Life (Here’s How)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
New Year, New Health Habits?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s that time of the year, and many of us hope to make this our healthiest year yet—or at least significantly improve it in some particular area that’s important to us! So, what news from the health world?
The rise of GLP-1 agonists continues
GLP-1 agonists have surged in popularity in the past year, and it looks like that trend is set to continue in the new one. The title of the below-linked pop-science article is slightly misleading, it’s not “almost three quarters of UK women”, but rather, “72% of the women using the digital weight loss platform Juniper”, which means the sample is confined to people interested in weight loss. Still, of those interested in weight loss, 72% is a lot, and the sample size was over 1000:
Read in full: New Year, new approach to weight loss: Almost three quarters of UK women are considering using GLP-1s in 2025
Related: 5 ways to naturally boost the “Ozempic Effect” ← these natural methods “hack” the same metabolic pathways as GLP-1 agonists do (it has to do with incretin levels), causing similar results
The lesser of two evils
Smoking is terrible, for everything. Vaping is… Not great, honestly, but as the below-discussed study shows, at the very least it results in much less severe respiratory symptoms than actual smoking. For many, vaping is a halfway-house to actually quitting; for some, it’s just harm reduction, and that too can be worthwhile.
We imagine that probably very few 10almonds readers smoke cigarettes, but we know quite a few use cannabis, which is discussed also:
Read in full: Switching to e-cigarettes may ease respiratory symptoms, offering hope for smokers
Related: Vaping: A Lot Of Hot Air? ← we look at the pros, cons, and popular beliefs that were true a little while ago but now they’re largely not (because of regulatory changes re what’s allowed in vapes)
Sometimes, more is more
The below-linked pop-science article has a potentially confusingly-worded title that makes it sound like increased exercise duration results in decreasing marginal returns (i.e., after a certain point, you’re getting very limited extra benefits), but in fact the study says the opposite.
Rather, increased moderate exercise (so, walking etc) results in a commensurately decreasing weight and a decreasing waistline.
In short: walk more, lose more (pounds and inches). The study examined those who moved their bodies for 150–300 minutes per week:
Read in full: Increased exercise duration linked to decreasing results in weight and waistline
Related: The Doctor Who Wants Us To Exercise Less, & Move More
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: