Retinoids: Retinol vs Retinal vs Retinoic Acid vs..?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I’m confused about retinol, retinal, retinoin, retinoids, etc, and of course every product claims to be the best, what’s the actual science on it?❞
Before we get into these skincare products, let’s first note that for most people, what’s best for the skin is good sleep and hydration, a plants-centric whole foods diet, and good stress management:
See for example: Of Brains And Breakouts: The Brain Skin Doctor
However, the world of potions and lotions can be an alluring one, and there is some merit there too. So, in a nutshell:
- Retinoids are the overall class of chemicals, and not a specific type
- Retinoic acid is the strongest form of this chemical and is prescription-controlled in most places
- “Retinoin” is probably tretinoin (all-trans retinoic acid) with the “t” having fallen off; we can only find it being used as a product name, not an actual substance
- Retinal, when it’s not an adjective referring to the retina (the part of the eye that receives refocussed light) and is instead a noun, is a less potent retinoid than the prescription-only kinds, but still stronger than retinol
- Retinol is a much less potent form, and is the most widely found in skincare products
- Retinoic acid is the strongest form of this chemical and is prescription-controlled in most places
All of them work the same way; it is only how serious they are about it that differs.
The mechanism of action is that they speed up the turnover (shedding cycle) of skin, so that cells are replaced sooner. As with any non-cancerous human tissue, this means that the tissue itself (in this case, your skin) will be biologically younger than if it had been replaced later.
The downside, of course, of this is that—while trying to make your skin healthier and more beautiful—the first thing that will happen is skin shedding. Depending on the retinoid type, dose, and the health of your skin to start with, this may mean anything from needing to exfoliate in the morning, to having to go to hospital with what looks like the world’s worst sunburn. For this reason, it is recommended to start with weaker products and lower doses, and work up carefully.
A note on doses: the recommended doses for these products are always truly tiny, like “use a pea-sized amount of this 0.05% serum on your face”. Take them seriously until you’re absolutely sure from experience that your skin can handle more.
Also, a tip: wear gloves when you apply any of the above products. This is because your fingers are also covered in skin, and if you don’t use gloves, then half the product that you intended for your face will be absorbed into your fingers instead. On the bright side, you’ll have beautifully rejuvenated fingertips, though.
You can learn more about the science of retinoids here, in our article about tretinoin, the usually prescription-only form of retinoic acid:
Tretinoin: Undo The Sun’s Damage To Your Skin
Want to try some?
We don’t sell it, but here for your convenience is an example product of retinal (stronger than retinol) on Amazon 😎
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
AC: The Power of Appetite Correction – by Dr. Bert Herring
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Appetite Correction” is an intriguing concept, and so it intrigued us sufficiently to read this book. So what’s it about?
It’s about modifying our response to hunger, and treating it as a messenger to whom we may say “thank you for your opinion” and then do as we already planned to do. And what is that?
Simply, this book is about intermittent fasting, specifically, 19:5 fasting, i.e., fast for 19 hours and eat during a 5hr window each day (the author proposes 5pm–10pm, but honestly, go with what works for you).
During the fasting period, drinking water, or consuming other non insulin-signalling things (e.g. black coffee, black tea, herbal tea, etc) is fine, but not so much as a bite of anything else (nor calorific drinks, e.g. with milk/cream or sugar in, and certainly not sodas, juices, etc).
During the eating period, the idea is to eat at will without restriction (even unhealthy things, if such is your desire) during those 5 hours, with the exception that one should start with something healthy. In other words, you can line up that take-out if you want, but eat a carrot first to break the fast. Or some nuts. Or whatever, but healthy.
The “appetite correction” part of it comes in with how, after a short adjustment period, you will get used to not suffering from hunger during the fasting period, and during the eating period, you will—paradoxically—be more able to practise moderation in your portions.
Most of the book is given over the dealing with psychological difficulties/objections, as well as some social objections, but he does also explain some of the science at hand too (i.e. how intermittent fasting works, on a physiological level). On which note…
The style is on the very light end of pop-science, and unusually, he doesn’t cite any sources for his claims at all. Now, no science that he claimed struck this reviewer as out of the ordinary, but it would have been nice to see a good few pages of bibliography at the back.
Bottom line: this is a super quick-and-easy read that makes a strong (albeit unsourced) case for intermittent fasting. It’s probably best for someone who would like the benefits and needs some persuading, but who is not very interested in delving into the science beyond being content to understand what is explained and put it into practice.
Click here to check out AC: The Power of Appetite Correction, and get yours where you want it!
Share This Post
-
Revealed: The Soviet Secret Recipe For Success That The CIA Admits Put The US To Shame
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today’s edition of 10almonds brings you a blast from the past with a modern twist: an ancient Russian peasant food that became a Soviet staple, and today, is almost unknown in the West.
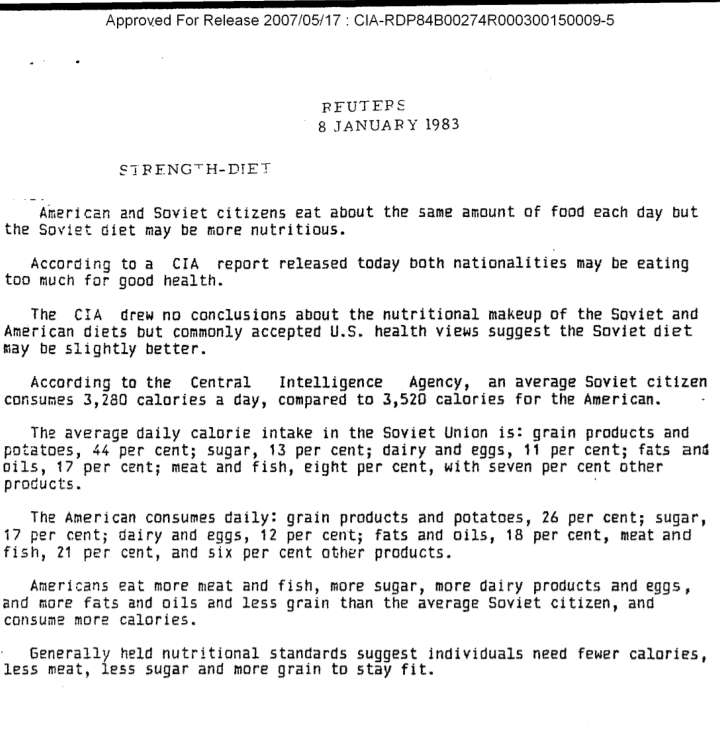
Before we get to that, let’s take a sneaky look at this declassified CIA memorandum from near the end of the Cold War:
(Click here to see a bigger version)
The take-away here is:
- Americans were eating 2–3 times more meat than Soviets
- Soviets were eating nearly double the amount of grain products and potatoes
…and both of these statistics meant that nutritionally speaking, the Soviets were doing better.
Americans also consumed more sugar and fats, which again, wasn’t the best dietary option.
But was the American diet tastier? Depends on whom you ask.
Which brings us to a literal recipe we’re going to be sharing with you today:
It’s not well-known in the West, but in Russia, it’s a famous national comfort food, a bastion of health and nutrition, and it rose to popularity because it was not only cheap and nutritious, but also, you could eat it for days without getting sick of it. And it could be easily frozen for reheating later without losing any of its appeal—it’d still be just as good.
In Russia there are sayings about it:
Щи да каша — пища наша (Shchi da kasha — pishcha nasha)
“Shchi and buckwheat are what we eat”
Top tip: buckwheat makes an excellent (and naturally sweet) alternative to porridge oats if prepared the same way!
Где щи, там и нас ищи (Gdye shchi, tam i nas ishchi)
“Where there’s shchi, us you’ll see”
Голь голью, а луковка во щах есть (Gol’ gol’yu, a lukovka vo shchakh yest’)
“I’m stark naked, but there’s shchi with onions”
There’s a very strong sentiment in Russia that really, all you need is shchi (shchi, shchi… shchi is all you need )
But what, you may ask, is shchi?
Our culinary cultural ambassador Nastja is here to offer her tried-and-tested recipe for…
…Russian cabbage soup (yes, really—bear with us now, and you can thank us later)
There are a lot of recipes for shchi (see for yourself what the Russian version of Lifehacker recommends), and we’ll be offering our favorite…
Nastja’s Nutritious and Delicious Homemade Shchi
Hi, Nastja here! I’m going to share with you my shchi recipe that is:
- Cheap
- So tasty
- Super nutritious*
- Vegan
- Gluten Free
You will also need:
- A cabbage (I use sweetheart, but any white cabbage will do)
- 1 cup (250g) red lentils (other kinds of lentils will work too)
- ½ lb or so (250–300g) tomatoes (I use baby plum tomatoes, but any kind will do)
- ½ lb or so (250–300g) mushrooms (the edible kind)
- An onion (I use a brown onion; any kind will do)
- Salt, pepper, rosemary, thyme, parsley, cumin
- Marmite or similar yeast extract (do you hate it? Me too. Trust me, it’ll be fine, you’ll love it. Omit if you’re a coward.)
- A little oil for sautéing (I use sunflower, but canola is fine, as is soy oil. Do not use olive oil or coconut oil, because the taste is too strong and the flashpoint too low)
First, what the French call mise-en-place, the prep work:
- Chop the cabbage into small strips, ⅛–¼ inch x 1 inch is a good guideline, but you can’t really go wrong unless you go to extremes
- Chop the tomatoes. If you’re using baby plum tomatoes (or cherry tomatoes), cut them in half. If using larger tomatoes, cut them into eighths (halve them, halve the halves, then halve the quarters)
- Chop the mushrooms. If using button mushrooms, half them. If using larger mushrooms, quarter them.
- Chop the onion finely.
- Gather the following kitchenware: A big pan (stock pot or similar), a sauté pan (a big wok or frying pan will do), a small frying pan (here a wok will not do), and a saucepan (a rice cook will also do)
Now, for actual cooking:
- Cook the red lentils until soft (I use a rice cooker, but a saucepan is fine) and set aside
- Sauté the cabbage, put it in the big pot (not yet on the heat!)
- Fry the mushrooms, put them in the big pot (still not yet on the heat!)
When you’ve done this a few times and/or if you’re feeling confident, you can do the above simultaneously to save time
- Blend the lentils into the water you cooked them in, and then add to the big pot.
- Turn the heat on low, and if necessary, add more water to make it into a rich soup
- Add the seasonings to taste, except the parsley. Go easy on the cumin, be generous with the rosemary and thyme, let your heart guide you with the salt and pepper.
- When it comes to the yeast extract: add about one teaspoon and stir it into the pot. Even if you don’t like Marmite, it barely changes the flavour (makes it slightly richer) and adds a healthy dose of vitamin B12.
We did not forget the tomatoes and the onion:
- Caramelize the onion (keep an eye on the big pot) and set it aside
- Fry the tomatoes and add them to the big pot
Last but definitely not least:
- Serve!
- The caramelized onion is a garnish, so put a little on top of each bowl of shchi
- The parsley is also a garnish, just add a little
Any shchi you don’t eat today will keep in the fridge for several days, or in the freezer for much longer.
*That nutritious goodness I talked about? Check it out:
- Lentils are high in protein and iron
- Cabbage is high in vitamin C and calcium
- Mushrooms are high in magnesium
- Tomatoes are good against inflammation
- Black pepper has a host of health benefits
- Yeast extract contains vitamin B12
Let us know how it went! We love to receive emails from our subscribers!
Share This Post
-
Infections, Heart Failure, & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some health news to round off the week:
The Infection That Leads To Heart Failure
It’s long been held that, for example, flossing reduces heart disease risk, with the hypothesis being that if plaque bacteria enter the blood stream, well, that’s an even worse place for plaque bacteria to be. Now, with much more data, attention has turned to
- actual infections, and
- actual heart failure
Way to up the ante! And, it holds true regardless of what kind of infection. So, you might think that a UTI, for example, is surely “downstream” and should not affect the heart, but it does. Because of this, researchers currently believe that it is not the infection itself, so much as the body’s inflammation response to infection, that leads to the heart failure. Which is reasonable, because, for example, atherosclerosis is made mostly not of cholesterol itself, but rather mostly of dead immune cells that got stuck in the cholesterol.
Moreover, it’s not so much about the acute inflammatory response (which is almost always a good thing, circumstantially), but rather that after cases where an infection managed to take hold, the immune system can then often stay on high alert for many years alter. Long COVID is an obvious recent example of this, but it’s hardly a new phenomenon; see for example post-polio syndrome, and consider how many more such post-infection maladies are likely to exist that never got a name because they flew under the radar or got diagnosed as fibromyalgia or something (fibromyalgia is a common diagnosis doctors give when they acknowledge something’s wrong, and it causes pain and exhaustion, but they don’t know what, and it appears to be stable—so while it can be helpful to put a name to the collection of symptoms, it’s a non-diagnosis diagnosis on the doctors’ part. It’s saying “I diagnose you with hurty tiredness”).
The take-away from all this? Avoid infections, for your heart’s sake, and if you do get an infection, take it seriously even if it’s minor. The safe amount of infection is “no infection”.
Read in full: Study uncovers new link between infections and heart failure
Cold Water Immersion: Hot Or Not?
The evidence is clear for some benefits; for others, not so much:
- It’s great (if you’re already in fair health, and definitely not if you have a heart condition) to improve circulation and stress response
- There may be some benefits to immune function, but however reasonable the hypothesis, actual evidence is thin on the ground
- The oft-hyped mood benefits are a) marginal b) short-lived, with benefits fading after 3 months of regular cold baths/showers/etc
Read in full: The big chill: Is cold-water immersion good for our health?
Related: Ice Baths: To Dip Or Not To Dip?
The Unspoken Trials Of Going To The Gym (While Being A Woman)
Public health decision-makers often think that getting people to go to the gym more is a matter of public information, or perhaps branding. Some who have their thinking heads on might even realize that there may be economic factors for many. But for women, there’s an additional factor—or rather, an additionally prominent factor. The study we’ll link started with this observation (please read it in the voice of your favorite nature documentary narrator):
❝Despite an increase in gym memberships, women are less active than men and little is known about the barriers women face when navigating gym spaces.❞
What then, of these shy, elusive creatures that make up a mere 51% of the world’s population?
A medium-sized (n=279) study of women, of whom 84% being current gym-goers, reported often feeling “judged for their appearance or performance, as well as having to fight for space in the gym and to be taken seriously, while navigating harassment and unsolicited comments from men”
Even gym attire becomes an issue:
❝Aligning with previous literature, women often chose attire based on comfort and functionality. However, their choices were also influenced by comparisons with others or fear of judgement for wearing non-branded attire or looking too put together. Many women also chose gym attire to hide perceived problem areas or avoid appearance concerns, including visible sweat stains.❞
…which main seem silly; you’re at the gym, of course you’re going to sweat, but if you’re the only one with visible sweat stains, then there can be social consequences (bad ones).
Similarly, there’s a “damned if you do; damned if you don’t” when it comes to working out while fat—on the one hand, society conflates fatness with laziness; on the other, it can be extra intimidating to be the only fat person in a gym full of people who look like they’re going to audition for a superhero movie.
❝In the gym, just like in other areas of life, women often feel stuck between being seen as ‘too much’ and ‘not enough’, dealing with judgement about how they look, how they perform, and even how much space they take up. Even though the pressure to be super thin is decreasing, the growing focus on being muscular and athletic is creating new challenges. It is pushing unrealistic standards that can negatively affect women’s body image and overall well-being.❞
Writer’s note: I live a few minutes walk from my nearest gym, and I work out at home instead. This way, if I want to do yoga in my pajamas, I can. If I want to use my treadmill naked and watch my T+A bounce in the mirror, I can. If I want to lift weights in the dress I happened to be wearing, I can. Alas that I can’t swim at home!
Read in full: Women face multiple barriers while exercising in gyms
Related: Body Image Dissatisfaction/Appreciation Across The Ages
Take care!
Share This Post
Related Posts
-
Driving under the influence of marijuana: An explainer and research roundup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Update 1: On May 16, 2024, the U.S. Department of Justice sent a proposed rule to the Federal Register to downgrade marijuana from a Schedule I to a Schedule III drug. This is the first step in a lengthy approval process that starts with a 60-day comment period.
Update 2: Two recent research studies were added to the “Studies on marijuana and driving” section of this piece on July 18, 2024.
As marijuana use continues to rise and state-level marijuana legalization sweeps the U.S., researchers and policymakers are grappling with a growing public safety concern: marijuana-impaired driving.
As of April 2023, 38 U.S. states had legalized medical marijuana and 23 had legalized its recreational use, according to the National Conference of State Legislatures. Recreational or medical marijuana measures are on the ballot in seven states this year.
The issue of marijuana-impaired driving has not been an easy one to tackle because, unlike alcohol, which has well-established thresholds of impairment, the metrics for marijuana’s effects on driving remain rather elusive.
“We don’t have that kind of deep knowledge right now and it’s not because of lack of trying,” says Dr. Guohua Li, professor of epidemiology and the founding director of the Center for Injury Science and Prevention at Columbia University.
“Marijuana is very different from alcohol in important ways,” says Li, who has published several studies on marijuana and driving. “And one of them is that the effect of marijuana on cognitive functions and behaviors is much more unpredictable than alcohol. In general, alcohol is a depressant drug. But marijuana could act on the central nervous system as a depressant, a stimulant, and a hallucinogenic substance.”
Efforts to create a breathalyzer to measure the level of THC, the main psychoactive compound found in the marijuana plant, have largely failed, because “the THC molecule is much bigger than ethanol and its behavior after ingestion is very different from alcohol,” Li says.
Currently, the two most common methods used to measure THC concentration to identify impaired drivers are blood and saliva tests, although there’s ongoing debate about their reliability.
Marijuana, a term interchangeably used with cannabis, is the most commonly used federally illegal drug in the U.S.: 48.2 million people, or about 18% of Americans reported using it at least once in 2019, according to the latest available data from the Centers for Disease Control and Prevention. Worldwide, 2.5% of the population consumes marijuana, according to the World Health Organization.
Marijuana is legal in several countries, including Canada, where it was legalized in 2018. Despite state laws legalizing cannabis, it remains illegal at the federal level in the U.S.
As states grapple with the contentious issue of marijuana legalization, the debate is not just about public health, potential tax revenues and economic interests. At the heart of the discussion is also the U.S. criminal justice system.
Marijuana is shown to have medicinal qualities and, compared with substances like alcohol, tobacco, and opioids, it has relatively milder health risks. However, it’s not risk-free, a large body of research has shown.
Marijuana consumption can lead to immediate effects such as impaired muscle coordination and paranoia, as well as longer-term effects on mental health and cognitive functions — and addiction. As its use becomes more widespread, researchers are trying to better understand the potential hazards of marijuana, particularly for younger users whose brains are in critical stages of development.
Marijuana and driving
The use of marijuana among drivers, passengers and pedestrians has increased steadily over the past two decades, Li says.
Compared with the year 2000, the proportion of U.S. drivers on the road who are under the influence of marijuana has increased by several folds, between five to 10 times, based on toxicology testing of people who died in car crashes, Li says.
A 2022 report from the National Transportation Safety Board finds alcohol and cannabis are the two most commonly detected drugs among drivers arrested for impaired driving and fatally injured drivers. Most drivers who tested positive for cannabis also tested positive for another potentially impairing drug.
“Although cannabis and many other drugs have been shown to impair driving performance and are associated with increased crash risk, there is evidence that, relative to alcohol, awareness about the potential dangers of driving after using other drugs is lower,” according to the report.
Indeed, many U.S. adults perceive daily marijuana use or exposure to its smoke safer than tobacco, even though research finds otherwise.
Several studies have demonstrated marijuana’s impact on driving.
Marijuana use can reduce the drivers’ ability to pay attention, particularly when they are performing multiple tasks, research finds. It also slows reaction time and can impair coordination.
“The combination is that you potentially have people who are noticing hazards later, braking slower and potentially not even noticing hazards because of their inability to focus on competing things on the road,” says Dr. Daniel Myran, an assistant professor at the Department of Family Medicine and health services researcher at the University of Ottawa.
In a study published in September in JAMA Network Open, Myran and colleagues find that from 2010 to 2021 the rate of cannabis-involved traffic injuries that led to emergency department visits in Ontario, Canada, increased by 475%, from 0.18 per 1,000 traffic injury emergency department visits in 2010 to 1.01 visits in 2021.
To be sure, cannabis-involved traffic injuries made up a small fraction of all traffic injury-related visits to hospital emergency departments. Out of 947,604 traffic injury emergency department visits, 426 had documented cannabis involvement.
Myran cautions the increase shouldn’t be solely attributed to marijuana legalization. It captures changing societal attitudes toward marijuana and acceptance of cannabis use over time in the lead-up to legalization. In addition, it may reflect an increasing awareness among health care providers about cannabis-impaired driving, and they may be more likely to ask about cannabis use and document it in medical charts, he says.
“When you look at the 475% increase in cannabis involvement in traffic injuries, rather than saying legalizing cannabis has caused the roads to be unsafe and is a public health disaster, it’s that cannabis use appears to be growing as a risk for road traffic injuries and that there seem to be more cannabis impaired drivers on the road,” Myran says. “Legalization may have accelerated this trend. Faced with this increase, we need to think about what are public health measures and different policy interventions to reduce harms from cannabis-impaired driving.”
Setting a legal limit for marijuana-impaired driving
Setting a legal limit for marijuana-impaired driving has not been easy. Countries like Canada and some U.S. states have agreed upon a certain level of THC in blood, usually between 1 to 5 nanograms per milliliter. Still, some studies have found those limits to be weak indicators of cannabis-impaired driving.
When Canada legalized recreational marijuana in 2018, it also passed a law that made it illegal to drive with blood THC levels of more than 2 nanograms. The penalties are more severe for blood THC levels above 5 nanograms. The blood test is done at the police station for people who are pulled over and are deemed to be drug impaired.
In the U.S., five states — Ohio, Illinois, Montana, Washington and Nevada — have “per se laws,” which set a specific amount of THC in the driver’s blood as evidence of impaired driving, according to the National Conference of State Legislatures. That limit ranges between 2 and 5 nanograms of THC per milliliter of blood.
Colorado, meanwhile, has a “permissible inference law,” which states that it’s permissible to assume the driver was under the influence if their blood THC level is 5 nanograms per milliliter or higher, according to NCSL.
Twelve states, most which have legalized some form of marijuana of use, have zero tolerance laws for any amount of certain drugs, including THC, in the body.
The remaining states have “driving under the influence of drugs” laws. Among those states, Alabama and Michigan, have oral fluid roadside testing program to screen drivers for marijuana and other drugs, according to NCSL.
In May this year, the U.S. Department of Transportation published a final rule that allows employers to use saliva testing for commercially licensed drivers, including truck drivers. The rule, which went into effect in June, sets the THC limit in saliva at 4 nanograms.
Saliva tests can detect THC for 8 to 24 hours after use, but the tests are not perfect and can results in false positives, leading some scientists to argue against using them in randomly-selected drivers.
In a 2021 report, the U.S. National Institute of Justice, the research and development arm of the Department of Justice, concluded that THC levels in bodily fluids, including blood and saliva “were not reliable indicators of marijuana intoxication.”
Studies on marijuana and driving
Over the past two decades, many studies have shown marijuana use can impair driving. However, discussions about what’s the best way to measure the level of THC in blood or saliva are ongoing. Below, we highlight and summarize several recent studies that address the issue. The studies are listed in order of publication date. We also include a list of related studies and resources to inform your audiences.
State Driving Under the Influence of Drugs Laws
Alexandra N. Origenes, Sarah A. White, Emma E. McGinty and Jon S. Vernick. Journal of Law, Medicine & Ethics, July 2024.Summary: As of January 2023, 33 states and D.C. had a driving under the influence of drugs law for at least one drug other than cannabis. Of those, 29 states and D.C. had a law specifically for driving under the influence of cannabis, in addition to a law for driving under the influence of other drugs. Four states had a driving under the influence of drug laws, excluding cannabis. Meanwhile, 17 states had no law for driving under the influence of drugs, including cannabis. “The 17 states lacking a DUID law that names specific drugs should consider enacting such a law. These states already have expressed their concern — through legislation — with drug-impaired driving. However, failure to name specific drugs is likely to make the laws more difficult to enforce. These laws may force courts and/or law enforcement to rely on potentially subjective indicators of impairment,” the authors write.
Associations between Adolescent Marijuana Use, Driving After Marijuana Use and Recreational Retail Sale in Colorado, USA
Lucas M. Neuroth, et al. Substance Use & Misuse, October 2023.Summary: Researchers use data from four waves (2013, 2015, 2017 and 2019) of the Healthy Kids Colorado Survey, including 47,518 students 15 and older who indicated that they drove. They find 20.3% of students said that they had used marijuana in the past month and 10.5% said they had driven under the influence of marijuana. They find that the availability of recreational marijuana in stores was associated with an increased prevalence of using marijuana one to two times in the past month and driving under the influence of marijuana at least once. “Over the study period, one in ten high school age drivers engaged in [driving after marijuana use], which is concerning given the high risk of motor vehicle-related injury and death arising from impaired driving among adolescents,” the authors write.
Are Blood and Oral Fluid Δ9-tetrahydrocannabinol (THC) and Metabolite Concentrations Related to Impairment? A Meta-Regression Analysis
Danielle McCartney, et al. Neuroscience & Biobehavioral Reviews, March 2022.Summary: Commonly used THC measurements may not be strong indicators of driving impairment. While there is a relationship between certain biomarkers like blood THC concentrations and impaired driving, this correlation is often weak. The study underscores the need for more nuanced and comprehensive research on this topic, especially as cannabis usage becomes more widespread and legally accepted.
The Effects of Cannabis and Alcohol on Driving Performance and Driver Behaviour: A Systematic Review and Meta-Analysis
Sarah M. Simmons, Jeff K. Caird, Frances Sterzer and Mark Asbridge. Addiction, January 2022.Summary: This meta-analysis of experimental driving studies, including driving simulations, confirms that cannabis impairs driving performance, contrary to some beliefs that it might enhance driving abilities. Cannabis affects lateral control and speed — typically increasing lane excursions while reducing speed. The combination of alcohol and marijuana appears worse than either alone, challenging the idea that they cancel each other out.
Cannabis Legalization and Detection of Tetrahydrocannabinol in Injured Drivers
Jeffrey R. Brubacher, et al. The New England Journal of Medicine, January 2022.Summary: Following the legalization of recreational marijuana in Canada, there was a notable increase in injured drivers testing positive for THC, especially among those 50 years of age or older. This rise in cannabis-related driving incidents occurred even with new traffic laws aiming to deter cannabis-impaired driving. This uptick began before legalization became official, possibly due to perceptions that cannabis use was soon-to-be legal or illegal but not enforced. The data suggests that while legalization has broad societal impacts, more comprehensive strategies are needed to deter driving under the influence of cannabis and raise public awareness about its risks.
Cannabis and Driving
Godfrey D. Pearlson, Michael C. Stevens and Deepak Cyril D’Souza. Frontiers in Psychiatry, September 2021.Summary: Cannabis-impaired driving is a growing public health concern, and studies show that such drivers are more likely to be involved in car crashes, according to this review paper. Drivers are less affected by cannabis than they are by alcohol or cocaine, but the problem is expected to escalate with increasing cannabis legalization and use. Unlike alcohol, THC’s properties make it challenging to determine direct impairment levels from testing results. Current roadside tests lack precision in detecting genuine cannabis-impaired drivers, leading to potential wrongful convictions. Moreover, there is a pressing need for research on the combined effects of alcohol and cannabis on driving, as well as the impact of emerging popular forms of cannabis, like concentrates and edibles. The authors recommend public awareness campaigns about the dangers of driving under the influence of cannabis, similar to those against drunk driving, to address misconceptions. Policymakers should prioritize science-based decisions and encourage further research in this domain.
Demographic And Policy-Based Differences in Behaviors And Attitudes Towards Driving After Marijuana Use: An Analysis of the 2013–2017 Traffic Safety Culture Index
Marco H. Benedetti, et al. BMC Research Notes, June 2021.Summary: The study, based on a U.S. survey, finds younger, low-income, low-education and male participants were more tolerant of driving after marijuana consumption. Notably, those in states that legalized medical marijuana reported driving after use more frequently, aligning with studies indicating a higher prevalence of THC detection in drivers from these states. Overall, while the majority perceive driving after marijuana use as dangerous, not all research agrees on its impairment effects. Existing studies highlight that marijuana impacts motor skills and executive functions, yet its direct correlation with crash risk remains debated, given the variations in individual tolerance and how long THC remains in the system.
Driving Under the Influence of Cannabis: A Framework for Future Policy
Robert M. Chow, et al.Anesthesia & Analgesia, June 2019.Summary: The study presents a conceptual framework focusing on four main domains: legalization, driving under the influence of cannabis, driver impairment, and motor vehicle accidents. With the growing legalization of cannabis, there’s an anticipated rise in cannabis-impaired driving cases. The authors group marijuana users into infrequent users who show significant impairment with increased THC blood levels, chronic users with minimal impairment despite high THC levels, and those with consistent psychomotor deficits. Current challenges lie in the lack of standardized regulation for drivers influenced by cannabis, primarily because of state-to-state variability and the absence of a federal statutory limit for blood THC levels. European nations, however, have established thresholds for blood THC levels, ranging from 0.5 to 50.0 micrograms per liter depending on whether blood or blood serum are tested. The authors suggest the combined use of alcohol and THC blood tests with a psychomotor evaluation by a trained professional to determine impairment levels. The paper stresses the importance of creating a structured policy framework, given the rising acceptance and use of marijuana in society.
Additional research
Cannabis-Involved Traffic Injury Emergency Department Visits After Cannabis Legalization and Commercialization
Daniel T. Myran, et al. JAMA Network Open, September 2023.Driving Performance and Cannabis Users’ Perception of Safety: A Randomized Clinical Trial
Thomas D. Marcotte, et al. JAMA Psychiatry, January 2022.Medicinal Cannabis and Driving: The Intersection of Health and Road Safety Policy
Daniel Perkins, et al. International Journal of Drug Policy, November 2021.Prevalence of Marijuana Use Among Trauma Patients Before and After Legalization of Medical Marijuana: The Arizona Experience
Michael Levine, et al. Substance Abuse, July 2021.Self-Reported Driving After Marijuana Use in Association With Medical And Recreational Marijuana Policies
Marco H. Benedetti, et al. International Journal of Drug Policy, June 2021.Cannabis and Driving Ability
Eric L. Sevigny. Current Opinion in Psychology, April 2021.The Failings of per se Limits to Detect Cannabis-Induced Driving Impairment: Results from a Simulated Driving Study
Thomas R. Arkell, et al. Traffic Injury Prevention, February 2021.Risky Driving Behaviors of Drivers Who Use Alcohol and Cannabis
Tara Kelley-Baker, et al. Transportation Research Record, January 2021.Direct and Indirect Effects of Marijuana Use on the Risk of Fatal 2-Vehicle Crash Initiation
Stanford Chihuri and Guohua Li. Injury Epidemiology, September 2020Cannabis-Impaired Driving: Evidence and the Role of Toxicology Testing
Edward C. Wood and Robert L. Dupont. Cannabis in Medicine, July 2020.Association of Recreational Cannabis Laws in Colorado and Washington State With Changes in Traffic Fatalities, 2005-2017
Julian Santaella-Tenorio, et al. JAMA Internal Medicine, June 2020.Marijuana Decriminalization, Medical Marijuana Laws, and Fatal Traffic Crashes in US Cities, 2010–2017
Amanda Cook, Gregory Leung and Rhet A. Smith. American Journal of Public Health, February 2020.Cannabis Use in Older Drivers in Colorado: The LongROAD Study
Carolyn G. DiGuiseppi, et al. Accident Analysis & Prevention, November 2019.Crash Fatality Rates After Recreational Marijuana Legalization in Washington and Colorado
Jayson D. Aydelotte, et al. American Journal of Public Health, August 2017.Marijuana-Impaired Driving: A Report to Congress
National Highway Traffic Safety Administration, July 2017Interaction of Marijuana And Alcohol on Fatal Motor Vehicle Crash Risk: A Case–Control Study
Stanford Chihuri, Guohua Li and Qixuan Chen. Injury Epidemiology, March 2017.US Traffic Fatalities, 1985–2014, and Their Relationship to Medical Marijuana Laws
Julian Santaella-Tenorio, et al. American Journal of Public Health, February 2017.Delays in DUI Blood Testing: Impact on Cannabis DUI Assessments
Ed Wood, Ashley Brooks-Russell and Phillip Drum. Traffic Injury Prevention, June 2015.Establishing Legal Limits for Driving Under the Influence of Marijuana
Kristin Wong, Joanne E. Brady and Guohua Li. Injury Epidemiology, October 2014.Cannabis Effects on Driving Skills
Rebecca L. Hartman and Marilyn A. Huestis. Clinical Chemistry, March 2014.Acute Cannabis Consumption And Motor Vehicle Collision Risk: Systematic Review of Observational Studies and Meta-Analysis
Mark Asbridge, Jill A. Hayden and Jennifer L. Cartwright. The BMJ, February 2012.Resources for your audiences
The following resources include explainers from federal agencies and national organizations. You’re free to use images and graphics from federal agencies.
- CDC’s main marijuana page.
- CDC’s marijuana data and statistics.
- Marijuana Drug Facts from the National Institute on Drug Abuse.
- Health Effects of Marijuana from the CDC.
- Learn About Marijuana Risks from the Substance Abuse and Mental Health Services Administration.
- Marijuana and Lung Health from the American Lung Association.
- Substance Use Disorder 101 from the U.S. Department of Health & Human Services.
- What You Need To Know About Marijuana Use and Driving from the CDC.
- Does marijuana use affect driving? from the National Institute on Drug Abuse.
- Drug-Impaired Driving from the National Highway Traffic Safety Administration.
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Synergistic Brain-Training
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let The Games Begin (But It Matters What Kind)
Exercise is good for brain health; we’ve written about this before, for example:
How To Reduce Your Alzheimer’s Risk ← there are many advices here, but exercise, especially cardiovascular exercise in this case, is an important item on the list!
Today it’s Psychology Sunday though, and we’re going to talk about looking after brain health by means of brain-training, via games.
“Brain-training” gets a lot of hype and flak:
- Hype: do sudoku every day and soon you will have an IQ of 200 and still have a sharp wit at the age of 120
- Flak: brain-training is usually training only one kind of cognitive function, with limited transferability to the rest of life
The reality is somewhere between the two. Brain training really does improve not just outwardly measurable cognitive function, but also internally measurable improvements visible on brain scans, for example:
- Cognitive training modified age-related brain changes in older adults with subjective memory decline
- Functional brain changes associated with cognitive training in healthy older adults: A preliminary ALE meta-analysis
But what about the transferability?
Let us play
This is where game-based brain-training comes in. And, the more complex the game, the better the benefits, because there is more chance of applicability to life, e.g:
- Sudoku: very limited applicability
- Crosswords: language faculties
- Chess: spatial reasoning, critical path analysis, planning, memory, focus (also unlike the previous two, chess tends to be social for most people, and also involve a lot of reading, if one is keen)
- Computer games: wildly varied depending on the game. While an arcade-style “shoot-em-up” may do little for the brain, there is a lot of potential for a lot of much more relevant brain-training in other kinds of games: it could be planning, problem-solving, social dynamics, economics, things that mirror the day-to-day challenges of running a household, even, or a business.
- It’s not that the skills are useful, by the way. Playing “Stardew Valley” will not qualify you to run a real farm, nor will playing “Civilization” qualify you to run a country. But the brain functions used and trained? Those are important.
It becomes easily explicable, then, why these two research reviews with very similar titles got very different results:
- A Game a Day Keeps Cognitive Decline Away? A Systematic Review and Meta-Analysis of Commercially-Available Brain Training Programs in Healthy and Cognitively Impaired Older Adults
- Game-based brain training for improving cognitive function in community-dwelling older adults: A systematic review and meta-regression
The first review found that game-based brain-training had negligible actual use. The “games” they looked at? BrainGymmer, BrainHQ, CogMed, CogniFit, Dakim, Lumosity, and MyBrainTrainer. In other words, made-for-purpose brain-trainers, not actual computer games per se.
The second reviewfound that game-based training was very beneficial. The games they looked at? They didn’t name them, but based on the descriptions, they were actual multiplayer online turn-based computer games, not made-for-purpose brain-trainers.
To summarize the above in few words: multiplayer online turn-based computer games outperform made-for-purpose brain-trainers for cognitive improvement.
Bringing synergy
However, before you order that expensive gaming-chair for marathon gaming sessions (research suggests a tail-off in usefulness after about an hour of continuous gaming per session, by the way), be aware that cognitive training and (physical) exercise training combined, performed close in time to each other or simultaneously, perform better than the sum of either alone:
See also:
❝Simultaneous training was the most efficacious approach for cognition, followed by sequential combinations and cognitive training alone, and significantly better than physical exercise.
Our findings suggest that simultaneously and sequentially combined interventions are efficacious for promoting cognitive alongside physical health in older adults, and therefore should be preferred over implementation of single-domain training❞
~ Dr. Hanna Malmberg Gavelin et al.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What families should know about whooping cough
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- Whooping cough is a bacterial respiratory illness that can cause long-term symptoms and even death.
- Two types of vaccines protect against it: The DTap vaccine is given to babies and children up to 6 years old, while the Tdap vaccine is given to children 7 years and older and adults.
- If you or your child has symptoms of whooping cough, isolate them from vulnerable family members and seek treatment early to reduce the risk of serious illness.
Whooping cough, also called pertussis, is a highly contagious respiratory illness that’s particularly dangerous for babies. Cases are now at least four times as high as they were at this time last year. Fortunately, vaccines are extremely effective at preventing the disease across age groups.
Read on to learn about the symptoms and risks of whooping cough, who should get vaccinated, and what to do when symptoms appear.What are the symptoms of whooping cough?
Early symptoms of whooping cough typically appear five to 10 days after exposure and may include a runny or stuffy nose, a low fever, and a mild cough. One to two weeks later, some people may experience extreme coughing fits that can cause shortness of breath, trouble sleeping, vomiting, fatigue, and rib fractures. These fits usually last one to six weeks, but they can last up to 10 weeks after infection.
About one in three babies under 1 year old who contract whooping cough require hospitalization, as they may experience life-threatening pauses in breathing (called apnea), pneumonia, and other complications. Children and adults who have asthma or are immunocompromised are also more likely to develop severe symptoms.
Which vaccines protect against whooping cough, and who is eligible?
Two types of vaccines protect against whooping cough: The DTap vaccine is given to babies and children up to 6 years old, while the Tdap vaccine is given to children 7 years and older and adults. Both vaccines protect against infections from diptheria, tetanus, and pertussis.
The Centers for Disease Control and Prevention recommends that pregnant people receive a single dose of the Tdap vaccine between 27 and 36 weeks of pregnancy, as this lowers the risk of whooping cough in babies younger than 2 months old by 78 percent.
Multiple doses are required for the best protection. Learn more about DTaP and Tdap vaccine schedules from the CDC, and talk to your health care provider about how many doses you and your children need.
What should families do when whooping cough symptoms appear?
If you or your child has symptoms of whooping cough, isolate the infected person from vulnerable family members. It’s also important to seek treatment early to reduce the risk of serious illness. Health care providers typically prescribe antibiotics to those recovering at home.
Over-the-counter cough and cold medicine is not recommended for children under 4 years old. However, limiting smoke, dust, and chemical fumes at home and using a humidifier can reduce coughing. If you are caring for someone with whooping cough who exhibits pauses in breathing or develops gray or blue skin, call 911 immediately.
For more information, talk to your health care provider.Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: