Women are less likely to receive CPR than men. Training on manikins with breasts could help
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
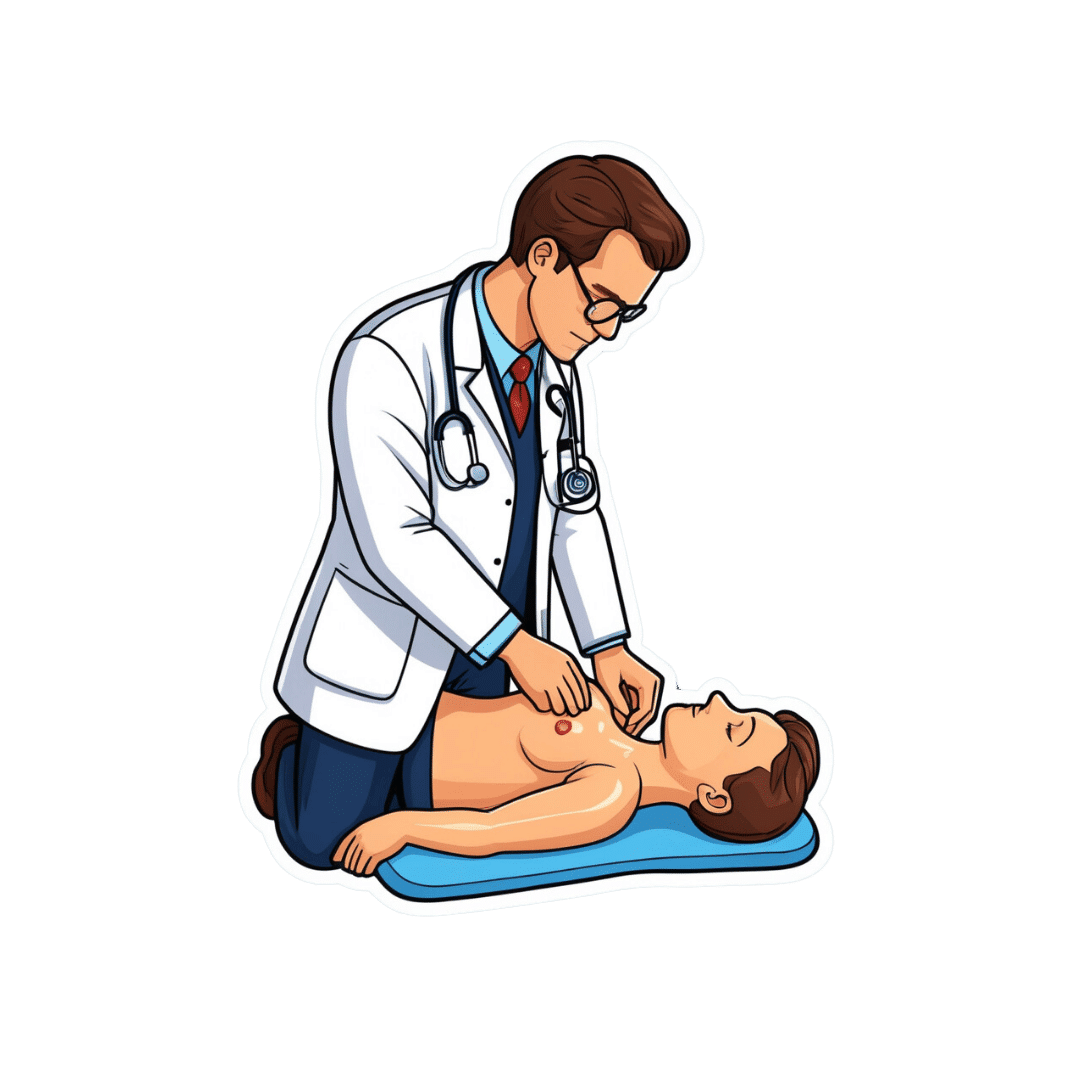
If someone’s heart suddenly stops beating, they may only have minutes to live. Doing CPR (cardiopulmonary resusciation) can increase their chances of survival. CPR makes sure blood keeps pumping, providing oxygen to the brain and vital organs until specialist treatment arrives.
But research shows bystanders are less likely to intervene to perform CPR when that person is a woman. A recent Australian study analysed 4,491 cardiac arrests between 2017–19 and found bystanders were more likely to give CPR to men (74%) than women (65%).
Could this partly be because CPR training dummies (known as manikins) don’t have breasts? Our new research looked at manikins available worldwide to train people in performing CPR and found 95% are flat-chested.
Anatomically, breasts don’t change CPR technique. But they may influence whether people attempt it – and hesitation in these crucial moments could mean the difference between life and death.

Heart health disparities
Cardiovascular diseases – including heart disease, stroke and cardiac arrest – are the leading cause of death for women across the world.
But if a woman has a cardiac arrest outside hospital (meaning her heart stops pumping properly), she is 10% less likely to receive CPR than a man. Women are also less likely to survive CPR and more likely to have brain damage following cardiac arrests.

These are just some of many unequal health outcomes women experience, along with transgender and non-binary people. Compared to men, their symptoms are more likely to be dismissed or misdiagnosed, or it may take longer for them to receive a diagnosis.
Bystander reluctance
There is also increasing evidence women are less likely to receive CPR compared to men.
This may be partly due to bystander concerns they’ll be accused of sexual harassment, worry they might cause damage (in some cases based on a perception women are more “frail”) and discomfort about touching a woman’s breast.
Bystanders may also have trouble recognising a woman is experiencing a cardiac arrest.
Even in simulations of scenarios, researchers have found those who intervened were less likely to remove a woman’s clothing to prepare for resuscitation, compared to men. And women were less likely to receive CPR or defibrillation (an electric charge to restart the heart) – even when the training was an online game that didn’t involve touching anyone.
There is evidence that how people act in resuscitation training scenarios mirrors what they do in real emergencies. This means it’s vital to train people to recognise a cardiac arrest and be prepared to intervene, across genders and body types.
Skewed to male bodies
Most CPR training resources feature male bodies, or don’t specify a sex. If the bodies don’t have breasts, it implies a male default.
For example, a 2022 study looking at CPR training across North, Central and South America, found most manikins available were white (88%), male (94%) and lean (99%).

These studies reflect what we see in our own work, training other health practitioners to do CPR. We have noticed all the manikins available to for training are flat-chested. One of us (Rebecca) found it difficult to find any training manikins with breasts.
A single manikin with breasts
Our new research investigated what CPR manikins are available and how diverse they are. We identified 20 CPR manikins on the global market in 2023. Manikins are usually a torso with a head and no arms.
Of the 20 available, five (25%) were sold as “female” – but only one of these had breasts. That means 95% of available CPR training manikins were flat-chested.
We also looked at other features of diversity, including skin tone and larger bodies. We found 65% had more than one skin tone available, but just one was a larger size body. More research is needed on how these aspects affect bystanders in giving CPR.
Breasts don’t change CPR technique
CPR technique doesn’t change when someone has breasts. The barriers are cultural. And while you might feel uncomfortable, starting CPR as soon as possible could save a life.
Signs someone might need CPR include not breathing properly or at all, or not responding to you.
To perform effective CPR, you should:
- put the heel of your hand on the middle of their chest
- put your other hand on the top of the first hand, and interlock fingers (keep your arms straight)
- press down hard, to a depth of about 5cm before releasing
- push the chest at a rate of 100-120 beats per minute (you can sing a song) in your head to help keep time!)
https://www.youtube.com/embed/Plse2FOkV4Q?wmode=transparent&start=94 An example of how to do CPR – with a flat-chested manikin.
What about a defibrillator?
You don’t need to remove someone’s bra to perform CPR. But you may need to if a defibrillator is required.
A defibrillator is a device that applies an electric charge to restore the heartbeat. A bra with an underwire could cause a slight burn to the skin when the debrillator’s pads apply the electric charge. But if you can’t remove the bra, don’t let it delay care.
What should change?
Our research highlights the need for a range of CPR training manikins with breasts, as well as different body sizes.
Training resources need to better prepare people to intervene and perform CPR on people with breasts. We also need greater education about women’s risk of getting and dying from heart-related diseases.
Jessica Stokes-Parish, Assistant Professor in Medicine, Bond University and Rebecca A. Szabo, Honorary Senior Lecturer in Critical Care and Obstetrics, Gynaecology and Newborn Health, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Seven Things To Do For Good Lung Health!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
YouTube Channel Wellness Check is challenging us all to do the following things. They’re framing it as a 30-day challenge, but honestly, there’s nothing here that isn’t worth doing for life
Here’s the list:
- Stop smoking (of course, smoking is bad for everything, but the lungs are one of its main areas of destruction)
- Good posture (a scrunched up chest is not the lungs’ best operating conditions!)
- Regular exercise (exercising your body in different ways exercises your lungs in different ways!)
- Monitor air quality (some environments are much better/worse than others, but don’t underestimate household air quality threats either)
- Avoid respiratory infections (shockingly, COVID is not great for your lungs, nor are the various other respiratory infections available)
- Check your O2 saturation levels (pulse oximeters like this one are very cheap to buy and easy to use)
- Prevent mucus and phlegm from accumulating (these things are there for reasons; the top reason is trapping pathogens, allergens, and general pollutants/dust etc; once those things are trapped, we don’t want that mucus there any more!)
Check out the video itself for more detail on each of these items:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to know more?
You might like our article about COPD:
Why Chronic Obstructive Pulmonary Disease (COPD) Is More Likely Than You Think
Take care!
Share This Post
-
Trout vs Carp – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing trout to carp, we picked the trout.
Why?
Both have their strong points!
In terms of macros, trout has slightly more protein and fat, and/but also has less cholesterol than carp. So, we pick the trout in the macros category.
In the category of vitamins, trout has much more of vitamins A, B1, B2, B3, B5, B6, B7, B12, C, D, E, K, and choline, while carp has slightly more vitamin B9. In other words, an easy win for trout here.
When it comes to minerals, however, trout has more potassium and selenium, while carp has more calcium, copper, iron, magnesium, manganese, phosphorus, and zinc. A fair win for carp this time.
You may be wondering about heavy metals: this will vary depending on location, as well as the age of the fish (younger fish have had less time to accumulate heavy metals than old ones, so if you’re visiting the fishmonger, choose the smaller ones) and the lives they have led (e.g. wild vs farmed), however, as a general rule of thumb, trout will generally have lower heavy metals levels than carp, all other things (e.g. location, age, etc) being equal.
In short, enjoy either or both in moderation, but trout wins on 3/4 categories today.
Want to learn more?
You might like to read:
Farmed Fish vs Wild Caught: Antibiotics, Mercury, & More
Take care!
Share This Post
-
Mimosa For Healing Your Body & Mind
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today we’re looking at mimosa (no relation to the cocktail!), which is a name given to several related plant species that belong to the same genus or general clade, look similar, and have similar properties and behavior.
As a point of interest that’s not useful: mimosa is one of those plants whereby if you touch it, it’ll retract its leaves and shrink away from you. The leaves also droop at nighttime (perfectly healthily; they’re not wilting or anything; this too is just plant movement), and spring back up in the daytime.
So that’s what we mean when we say “and behavior” 😉
Antidepressant & anxiolytic
Mimosa bark and leaves have long been used in Traditional Chinese Medicine, as well as (albeit different species) in the North-East of Brazil, and (again, sometimes different species) in Mexico.
Animal studies, in vivo studies, and clinical practice in humans, have found this to be effective, for example:
❝[Mimosa pudica extract] has anti-anxiety, anti-depressant and memory enhancing activities that are mediated through multiple mechanisms❞
Source: Effects of Mimosa pudica L. leaves extract on anxiety, depression and memory
Research is ongoing with regard to how, exactly, mimosa does what it does. Here’s a paper about another species mimosa:
(notwithstanding the genus name, it’s still part of the mimosa clade)
Anti-inflammatory & analgesic
In this case, mimosa has traditionally been used as a topical tincture (for skin damage of many kinds, ranging from cuts and abrasions to burns to autoimmune conditions and more), so what does the science say about that?
❝In summary, the present study provided evidence that the [mimosa extract], its fractions and the isolated compound sakuranetin showed significant anti-inflammatory and antinociceptive activities❞
Wound healing
About those various skin damages, here’s another application, and a study showing that it doesn’t just make it feel better, it actually helps it to heal, too:
❝Therapeutic effectiveness occurred in all patients of the extract group; after the 8th treatment week, ulcer size was reduced by 92% as mean value in this group, whereas therapeutic effectiveness was observed only in one patient of the control group (chi(2), p=0.0001). No side effects were observed in any patient in either group.❞
Very compelling stats!
Read more: Therapeutic effectiveness of a Mimosa tenuiflora cortex extract in venous leg ulceration treatment
Is it safe?
Yes, for most people, with some caveats:
- this one comes with a clear “don’t take if pregnant or breastfeeding” warning, as for unknown reasons it has caused a high incidence of fetal abnormalities or fetal death in animal studies.
- while the stem bark (the kind used in most mimosa supplements and most readily found online) has negligible psychoactivity, as do many species of mimosa in general, the root of M. tenuiflora has psychedelic effects similar to ayahuasca if taken orally, for example as a decoction, if in the presence of a monoamine oxidase inhibitor (MAOI), as otherwise MAO would metabolize the psychoactive component in the gut before it can enter the bloodstream.
That’s several “ifs”, meaning that the chances of unwanted psychedelic effects are slim if you’re paying attention, but as ever, do check with your doctor/pharmacist to be sure.
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
Related Posts
-
Will there soon be a cure for HIV?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Human immunodeficiency virus, or HIV, is a chronic health condition that can be fatal without treatment. People with HIV can live healthy lives by taking antiretroviral therapy (ART), but this medication must be taken daily in order to work, and treatment can be costly. Fortunately, researchers believe a cure is possible.
In July, a seventh person was reportedly cured of HIV following a 2015 stem cell transplant for acute myeloid leukemia. The patient stopped taking ART in 2018 and has remained in remission from HIV.
Read on to learn more about HIV, the promise of stem cell transplants, and what other potential cures are on the horizon.
What is HIV?
HIV infects and destroys the immune system’s cells, making people more susceptible to infections. If left untreated, HIV will severely impair the immune system and progress to acquired immunodeficiency syndrome (AIDS). People living with untreated AIDS typically die within three years.
People with HIV can take ART to help their immune systems recover and to reduce their viral load to an undetectable level, which slows the progression of the disease and prevents them passing the virus to others.
How can stem cell transplants cure HIV?
Several people have been cured of HIV after receiving stem cell transplants to treat leukemia or lymphoma. Stem cells are produced by the spongy tissue located in the center of some bones, and they can turn into new blood cells.
A mutation on the CCR5 gene prevents HIV from infecting new cells and creates resistance to the virus, which is why some HIV-positive people have received stem cells from donors carrying this mutation. (One person was reportedly cured of HIV after receiving stem cells without the CCR5 mutation, but further research is needed to understand how this occurred.)
Despite this promising news, experts warn that stem cell transplants can be fatal, so it’s unlikely this treatment will be available to treat people with HIV unless a stem cell transplant is needed to treat cancer. People with HIV are at an increased risk for blood cancers, such as Hodgkin lymphoma and non-Hodgkin lymphoma, which stem cell transplants can treat.
Additionally, finding compatible donors with the CCR5 mutation who share genetic heritage with patients of color can be challenging, as donors with the mutation are typically white.
What are other potential cures for HIV?
In some rare cases, people who started ART shortly after infection and later stopped treatment have maintained undetectable levels of HIV in their bodies. There have also been some people whose bodies have been able to maintain low viral loads without any ART at all.
Researchers are studying these cases in their search for a cure.
Other treatment options researchers are exploring include:
- Gene therapy: In addition to stem cell transplants, gene therapy for HIV involves removing genes from HIV particles in patients’ bodies to prevent the virus from infecting other cells.
- Immunotherapy: This treatment is typically used in cancer patients to teach their immune systems how to fight off cancer. Research has shown that giving some HIV patients antibodies that target the virus helps them reach undetectable levels of HIV without ART.
- mRNA technology: mRNA, a type of genetic material that helps produce proteins, has been used in vaccines to teach cells how to fight off viruses. Researchers are seeking a way to send mRNA to immune system cells that contain HIV.
When will there be a cure for HIV?
The United Nations and several countries have pledged to end HIV and AIDS by 2030, and a 2023 UNAIDS report affirmed that reaching this goal is possible. However, strategies to meet this goal include HIV prevention and improving access to existing treatment alongside the search for a cure, so we still don’t know when a cure might be available.
How can I find out if I have HIV?
You can get tested for HIV from your primary care provider or at your local health center. You can also purchase an at-home HIV test from a drugstore or online. If your at-home test result is positive, follow up with your health care provider to confirm the diagnosis and get treatment.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Ways To Beat Cancer (And Other Diseases)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Systematic Approach To Healthy Eating
This is Dr. William Li. He’s a physician, cancer researcher, and educator. He also founded the Angiogenesis Foundation back in 1994.
We recently reviewed one of his books, “Eat To Beat Disease”.
He has another book that we haven’t reviewed at time of writing, “Eat To Beat Your Diet“, which you might like to check out.
What does he want us to know?
He wants us to know how to eat to beat cancer and other diseases, by means of five specific angles:
Angiogenesis
This is about replacing blood vessels, which of course happens all the time, but it becomes a problem when it is feeding a cancer in the process.
Here, based on Dr. Li’s work, is what can be done about it:
A List of Anti-Angiogenic Foods for a Cancer-Fighting Diet
Regeneration
Generally speaking, we want to replace healthy cells early, because if we wait until they get damaged, then that damage will be copied forwards. As well as intermittent fasting, there are other things we can do to promote this—even, Dr. Li’s research shows, for stem cells:
Doctor’s Tip: Regeneration (stem cells)—one of your body’s five defense systems
Microbiome health
Healthy gut, healthy rest of the body. We’ve written about this before:
Making Friends With Your Gut (You Can Thank Us Later)
DNA protection
DNA gets unravelled and damaged with age, the telomere caps get shorter, and mistakes get copied forward. So there more we can protect our DNA, the longer we can live healthily. There are many ways to do this, but Dr. Li was one of the first to bring to light the DNA-protecting benefits of kiwi fruit:
Immunity
Paradoxically, what’s good for your immune system (making it stronger) also helps to protect against autoimmune diseases (for most people, for the most part).
In short: it’s good to have an immune system that’s powerful not just in its counterattacks, but also in its discerning nature. There are dietary and other lifestyle approaches to both, and they’re mostly the same things:
Beyond Supplements: The Real Immune-Boosters!
and thus see also:
Want to know more?
You might enjoy his blog or podcast, and here’s his TED talk:
Want to watch it, but not right now? Bookmark it for later
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Best Salt for Neti Pots?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
❓ Q&A With 10almonds Subscribers!
Q: What kind of salt is best for neti pots?
A: Non-iodised salt is usually recommended, but really, any human-safe salt is fine. By this we mean for example:
- Sodium chloride (like most kitchen salts),
- Potassium chloride (as found in “reduced sodium” kitchen salts), or
- Magnesium sulfate (also known as epsom salts).
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: