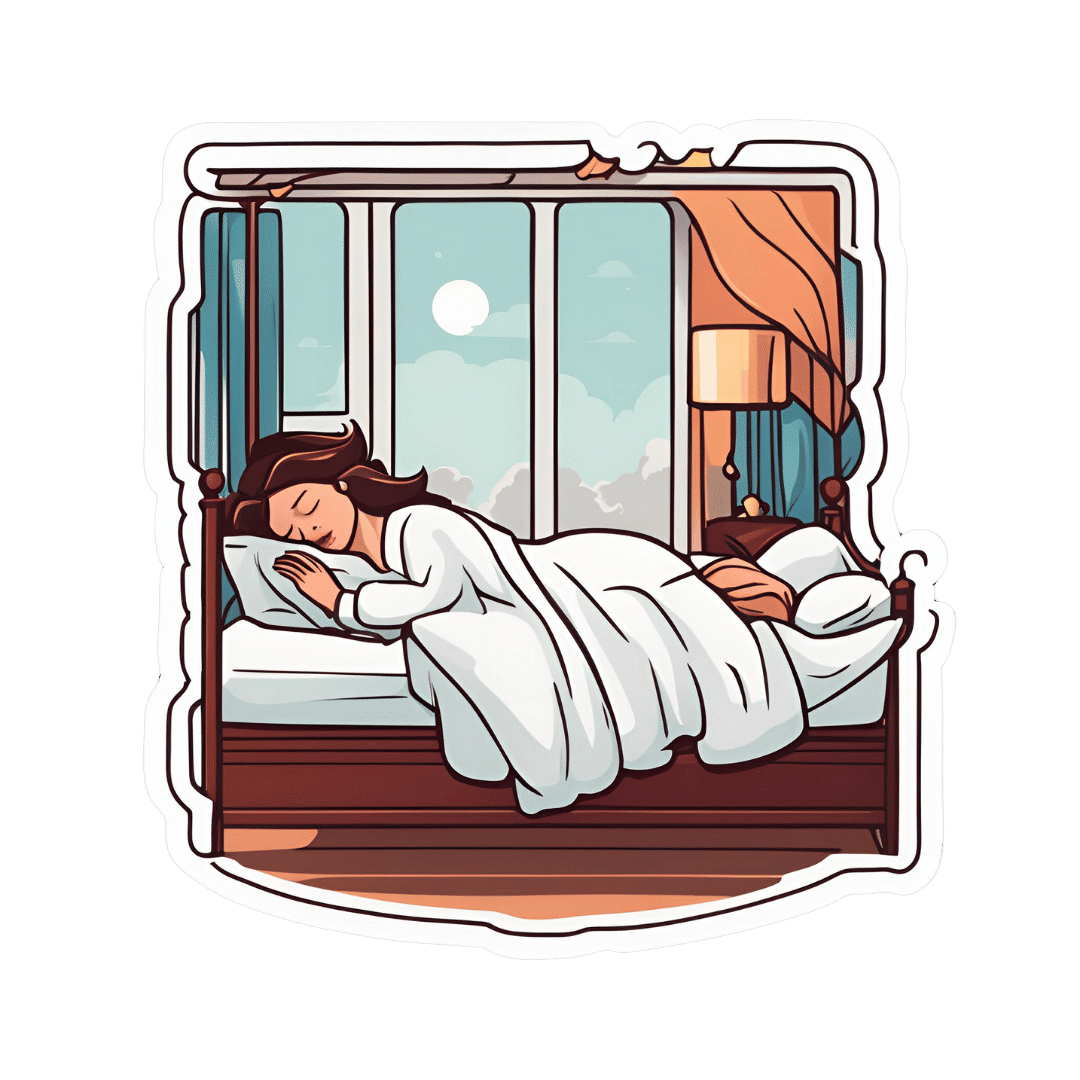
How Your Sleep Position Changes Dementia Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is not just about sleep duration or even about sleep quality… It really is about which way your body is positioned.
Goodnight, glymphatic system
The association between sleeping position and dementia risk is about glymphatic drainage, which is largely powered by gravity (and thus dependent on which way around your head and neck are oriented), and very important for clearing toxins out of the brain—including beta-amyloid proteins.
This becomes particularly important when the glymphatic system becomes less efficient in midlife, often 15–20 years before cognitive decline symptoms appear.
The video’s thumbnail headline, “SCIENTISTS REVEAL: THE WAY YOUR SLEEP CAN CAUSE DEMENTIA” is overstated and inaccurate, but our adjusted headline “how your sleep position changes dementia risk” is actually representative of the paper on which this video was based; we’ll quote from the paper itself here:
❝This paper concludes that 1. glymphatic clearance plays a major role in Alzheimer’s pathology; 2. the vast majority of waste clearance occurs during sleep; 3. dementias are associated with sleep disruption, alongside an age-related decline in AQP4 polarization; and 4. lifestyle choices such as sleep position, alcohol intake, exercise, omega-3 consumption, intermittent fasting and chronic stress all modulate* glymphatic clearance. Lifestyle choices could therefore alter Alzheimer’s disease risk through improved glymphatic clearance, and could be used as a preventative lifestyle intervention for both healthy brain ageing and Alzheimer’s disease.❞
…and specifically, they found:
❝Glymphatic transport is most efficient in the right lateral sleeping position, with more CSF clearance occurring compared to supine and prone. The average person changes sleeping position 11 times per night, but there was no difference in the number of position changes between neurodegenerative and control groups, making the percentage of time spent in supine position the risk factor, not the number of position changes❞
Read the paper in full here: The Sleeping Brain: Harnessing the Power of the Glymphatic System through Lifestyle Choices
*saying “modulate” here is not as useful as it could be, because they modulate it differently: side-sleeping improves clearance; back sleeping decreases it; front-sleeping isn’t great either. Alcohol intake reduces clearance, exercise (especially cardiovascular exercise) improves it; omega-3 consumption improves it up a degree and does depend on omega-3/6 ratios, intermittent fasting improves it, and chronic stress worsens it.
And for a more pop-science presentation, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Clean Your Brain (Glymphatic Health Primer)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dr. Greger’s Daily Dozen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Give Us This Day Our Daily Dozen
This is Dr. Michael Greger. He’s a physician-turned-author-educator, and we’ve featured him and his work occasionally over the past year or so:
- Brain Food? The Eyes Have It! ← this is about dark leafy greens, lutein, & avoiding Alzheimer’s
- Twenty-One, No Wait, Twenty Tweaks For Better Health ← he says 21, but we say one of them is very skippable. Check it out and decide what you think!
- Dr. Greger’s Anti-Aging Eight ← his top well-evidenced interventions specifically for slowing aging
But what we’ve not covered, astonishingly, is one of the things for which he’s most famous, which is…
Dr. Greger’s Daily Dozen
Based on the research in the very information-dense tome that his his magnum opus How Not To Die (while it doesn’t confer immortality, it does help avoid the most common causes of death), Dr. Greger recommends that we take care to enjoy each of the following things per day:
Beans
- Servings: 3 per day
- Examples: ½ cup cooked beans, ¼ cup hummus
Greens
- Servings: 2 per day
- Examples: 1 cup raw, ½ cup cooked
Cruciferous vegetables
- Servings: 1 per day
- Examples: ½ cup chopped, 1 tablespoon horseradish
Other vegetables
- Servings: 2 per day
- Examples: ½ cup non-leafy vegetables
Whole grains
- Servings: 3 per day
- Examples: ½ cup hot cereal, 1 slice of bread
Berries
- Servings: 1 per day
- Examples: ½ cup fresh or frozen, ¼ cup dried
Other fruits
- Servings: 3 per day
- Examples: 1 medium fruit, ¼ cup dried fruit
Flaxseed
- Servings: 1 per day
- Examples: 1 tablespoon ground
Nuts & (other) seeds
- Servings: 1 per day
- Examples: ¼ cup nuts, 2 tablespoons nut butter
Herbs & spices
- Servings: 1 per day
- Examples: ¼ teaspoon turmeric
Hydrating drinks
- Servings: 60 oz per day
- Examples: Water, green tea, hibiscus tea
Exercise
- Servings: Once per day
- Examples: 90 minutes moderate or 40 minutes vigorous
Superficially it seems an interesting choice to, after listing 11 foods and drinks, have the 12th item as exercise but not add a 13th one of sleep—but perhaps he quite reasonably expects that people get a dose of sleep with more consistency than people get a dose of exercise. After all, exercise is mostly optional, whereas if we try to skip sleep for too long, our body will force the matter for us.
Further 10almonds notes:
- We’d consider chia superior to flax, but you do you. Flax is a fine choice also.
- We recommend trying to get each of these top 5 most health-giving spices in daily if you can.
Enjoy!
Share This Post
-
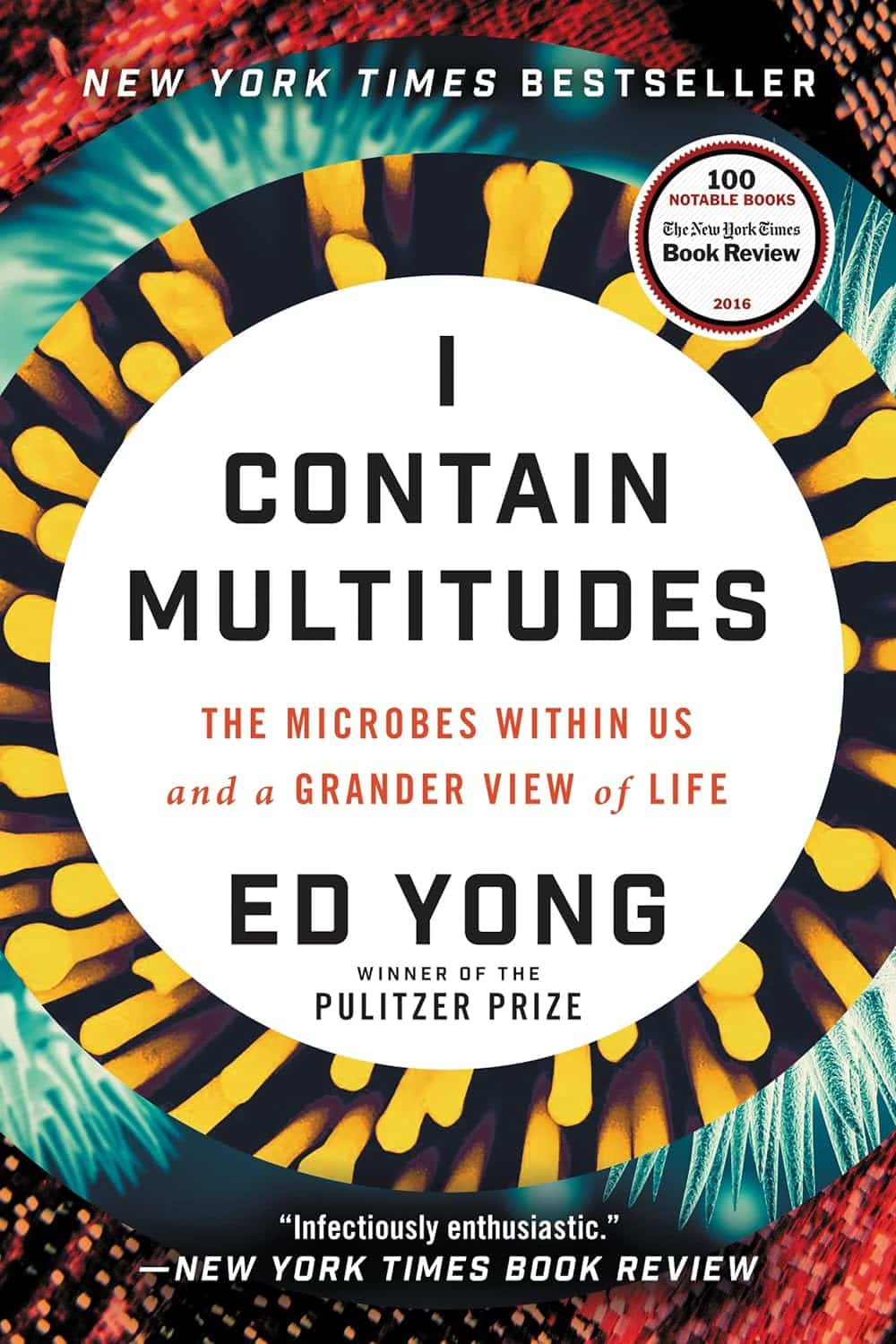
I Contain Multitudes – by Ed Yong
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A little while back we reviewed a book (Planet of Viruses) about the role of viruses in our lives, beyond the obvious. Today’s book gives the same treatment to microbes in general—mostly bacteria.
We all know about pathogens, and we all know about gut microbiota and that some (hopefully the majority) there are good for our health. This book covers those things too, but also much more.
Pulitzer Prize-winning science writer Ed Yong takes a big picture view (albeit, of some very small things) and looks at the many ways microbes keep us alive, directly or indirectly. From the microbes that convert certain proteins in breast milk into a form that babies can digest (yes, this means we produce nutrients in breast milk that have been evolved solely to feed that bacterium), to those without which agriculture would simply not work, we’re brought to realize how much our continued existence is contingent on our trillions of tiny friends.
The style throughout is easy-reading pop-science, very accessible. There’s also plenty in terms of practical take-away value, when it comes to adjusting our modern lives to better optimize the benefits we get from microbes—inside and out.
Bottom line: if you’d like to learn about the role of microbes in our life beyond “these ones are pathogens” and “these ones help our digestion”, this is the book for you.
Click here to check out I Contain Multitudes, and learn more about yours and those around you!
Share This Post
-
The Hormone Therapy That Reduces Breast Cancer Risk & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Hormone Balancing Act
We’ve written before about menopausal HRT:
What You Should Have Been Told About Menopause Beforehand
…and even specifically about the considerations when it comes to breast cancer risk:
Menopausal Hormone Replacement Therapy
this really does bear reading, by the way—scroll down to the bit about breast cancer risk, because it’s not a simple increased/decreased risk; it can go either way, and which way it goes will depend on various factors including your medical history and what HRT, if any, you are taking.
Hormone Modulating Therapy
Hormone modulating therapy, henceforth HMT, is something a little different.
Instead of replacing hormones, as hormone replacement therapy does, guess what hormone modulating therapy does instead? That’s right…
MHT can modulate hormones by various means, but the one we’re going to talk about today does it by blocking estrogen receptors,
Isn’t that the opposite of what we want?
You would think so, but since for many people with an increased breast cancer risk, the presence of estrogen increases that risk, which leaves menopausal (peri- or post) people in an unfortunate situation, having to choose between increased breast cancer risk (with estrogen), or osteoporosis and increased dementia risk, amongst other problems (without).
However, the key here (in fact, that’s a very good analogy) is in how the blocker works. Hormones and their receptors are like keys and locks, meaning that the wrong-shaped hormone won’t accidentally trigger it. And when the right-shaped hormone comes along, it gets activated and the message (in this case, “do estrogenic stuff here!” gets conveyed). A blocker is sufficiently similar to fit into the receptor, without being so similar as to otherwise act as the hormone.
In this case, it has been found that HMT blocking estrogen receptors was sufficient to alleviate the breast cancer risk, while also being associated with a 7% lower risk of developing Alzheimer’s disease or related dementias, with that risk reduction being even greater for some demographics depending on race and age. Black women in the 65–74 age bracket enjoyed a 24% relative risk reduction, with white women of the same age getting an 11% relative risk reduction. Black women enjoyed the same benefits after that age, whereas white women starting it at that age did not get the same benefits. The conclusion drawn from this is that it’s good to start this at 65 if relevant and practicable, especially if white, because the protective effect is strongest when gained aged 65–69.
Here’s a pop-science article that goes into the details more deeply than we have room for here:
Hormone therapy for breast cancer linked with lower dementia risk
And here’s the paper itself; we highly recommend reading at least the abstract, because it goes into the numbers in much more detail than we reasonably can here. It’s a huge cohort study of 18,808 women aged 65 years or older, so this is highly relevant data:
Want to learn more?
If you’d like a much deeper understanding of breast cancer risk management, including in the context of hormone therapy, you might like this excellent book that we reviewed recently:
The Smart Woman’s Guide to Breast Cancer – by Dr. Jenn Simmons
Take care!
Share This Post
Related Posts
-
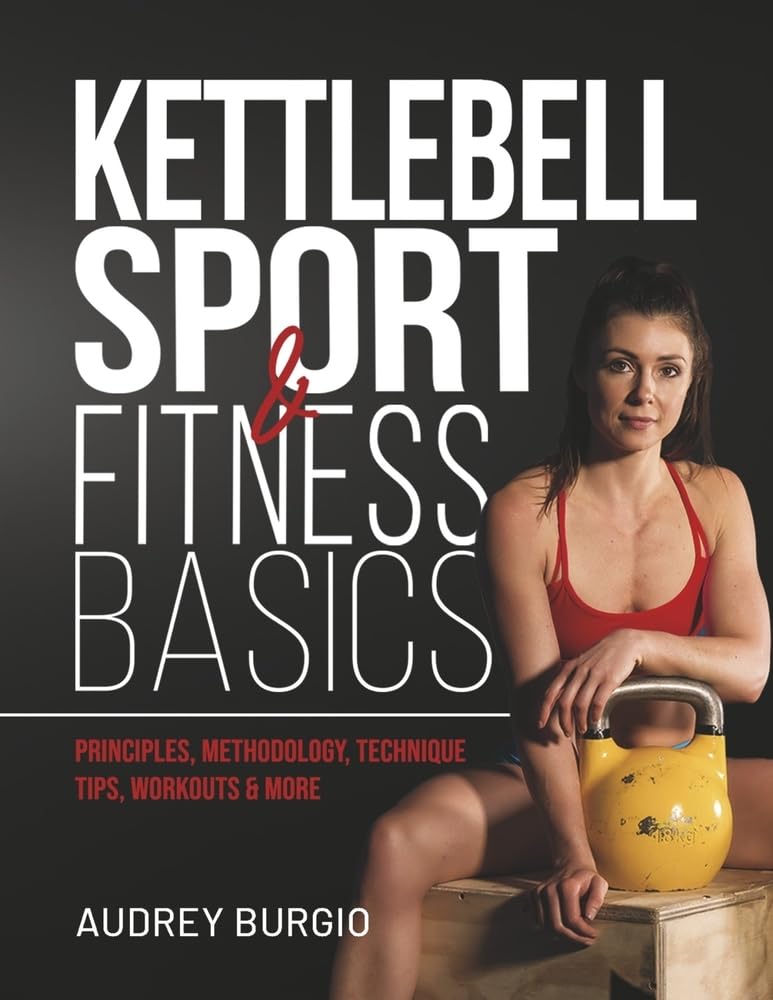
Kettlebell Sport & Fitness Basics – by Audrey Burgio
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Professional athlete & coach Audrey Burgio covers how to get a full-body workout that will make you stronger and more flexible (there are stretches here too, and many exercises are about strength and suppleness), as well as building stability and balance. In short, more robust and with better mobility.
Which is one of the best things about kettlebell training—unlike dumbbells and barbells, a kettlebell requires the kind of strength that one has to use when doing many routine tasks, from carrying the groceries to moving a big pan in the kitchen.
Because it is otherwise absolutely possible to look like Arnold Schwarzenegger in the gym, and then still pull a muscle moving something at home because the angle was awkward or somesuch!
However, making one’s body so robust does require training safely, and the clear instructions in this book will help the reader avoid injuries that might otherwise be incurred by just picking up some kettlebells and guessing.
Bottom line: if you’d like to get strong and supple from the comfort of your own home, this book can definitely lead the way!
Click here to check out Kettlebell Sport & Fitness Basics, and see the difference in your body!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Air Purifiers & Sleep
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I’ve read that air pollution has a negative effect on sleep quality and duration. Since I live next to a busy road, I was wondering whether I should invest in an air purifier. What are 10Almonds’s views?❞
Going straight to the science, there are two questions here:
- Does air pollution negatively affect sleep quality and duration?
- Does the use of an air purify actually improve the air quality in the way(s) necessary to make a difference?
We thought we’d have to tackle these questions separately, but we did find one study that addressed your question directly. It was a small study (n=30 if you believe the abstract; n=29 if you read the paper itself—one person dropped out); the results were modest but clear:
❝The purifier filter was associated with increased total sleep time for an average of 12 min per night, and increased total time in bed for an average of 19 min per night relative to the placebo.
There were several sleep and mood outcomes for which no changes were observed, and time awake after sleep onset was higher for the purifier filter. Air quality was better during the high-efficiency particulate air filter condition.
These findings offer positive indications that environmental interventions that improve air quality can have benefits for sleep outcomes in healthy populations who are not exhibiting clinical sleep disturbances.❞
In the above-linked paper’s introduction, it does establish the deleterious effect of air pollution on a wide variety of health metrics, including sleep, this latter evidenced per Caddick et al. (2018): A review of the environmental parameters necessary for an optimal sleep environment
Now, you may be wondering: is an extra 12 minutes per night worth it?
That’s your choice to make, but we would argue that it is. We can make many choices in our lives that affect our health slightly for the better or the worse. If we make a stack of choices in a particular direction, the effects will also stack, if not outright compound.
So in the case of sleep, it might be (arbitrary numbers for the sake of illustration):
- Get good exercise earlier in the day (+3%)
- Get good food earlier in the day (+2.5%)
- Practice mindfulness/meditation before bed (+2.5%)
- Have a nice dark room (+5%)
- Have fresh bedding (+2.5%)
- Have an air purifier running (+3%)
Now, those numbers are, as we said, arbitrary*, but remember that percentages don’t add up; they compound. So that “+3%” starts being a lot more meaningful than if it were just by itself.
*Confession: the figure of 3% for the air purifier wasn’t entirely arbitrary; it was based on 100(12/405) = 80/27 ≈ 3, wherein the 405 figure was an approximation of the average total time (in minutes) spent sleeping with placebo, based on a peep at their results graph. There are several ways the average could be reasonably calculated, but 6h45 (i.e., 405 minutes) was an approximate average of those reasonable approximate averages.
So, 12 minutes is a 3% improvement on that.
Don’t have an air purifier and want one?
We don’t sell them, but here’s an example on Amazon, for your convenience
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A Planet of Viruses – by Carl Zimmer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed numerous books on the immune system before, and this one’s mostly not about that.
Instead, this one focuses on the viruses themselves, and the part they play in our world, for good and for ill. Popular awareness tends to focus on the ill, of course.
But, there’s a lot that viruses do for us too, including:
- Weak/harmless viruses that keep our immune systems on their toes and ready
- Bacteriophage viruses that kill and consume pathogens that, left unchecked, would do the same to us
- Endogenous retroviruses that have become symbiotic with the human organism, without which our species would quickly go extinct
He also talks about biological warfare, and how we cannot bury our heads in the sand by avoiding research on those grounds, because someone will always do it anyway, so (as the motto of the immune system itself might say), best to be prepared.
The author is a science journalist, by the way, and has no PhD, but does have a flock of Fellowships and assorted scientific awards and honors, so he appears to be doing good work so far as the scientific community is concerned.
Bottom line: if you’d like to know more about viruses than “they’re very small and can cause harm”, then this book will open a whole new world.
Click here to check out A Planet of Viruses, and upgrade your knowledge!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: