What Nobody Teaches You About Strengthening Your Knees
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Strengthening unhappy knees can seem difficult, because many obvious exercises like squats may hurt, and can feel like they are doing harm (and if your knees are bad enough, maybe they are; it depends on many factors). Here’s a way to improve things:
The muscle nobody talks about
Well, not nobody. But, it’s a muscle that’s rarely talked about; namely, the tibialis anterior.
It plays a key role in decelerating knee motion—in other words, the movement that hurts if you have bad knees. It’s essential for absorbing shock during activities like walking, climbing stairs, and stepping off curbs
So, of course, strengthening this muscle supports knee health.
The exercise this video recommends for strengthening it involves leaning against a wall with feet about a foot away (closer feet make it easier, further makes it harder). Note, this is a lean, not a “Roman chair”.
The exercise involves squeezing the quadriceps, lifting toes toward the nose, and engaging the tibialis anterior muscle. If you’re wondering what to do with your hands, they can be held out with palms open to work on posture, or hanging by the sides. Do this for about 1½–2 minutes.
For more on all this, plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
When Bad Joints Stop You From Exercising (5 Things To Change)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Holy Basil: What Does (And Doesn’t) It Do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, a quick clarification:
- Ocimum sanctum is the botanical name given to what in English we call holy basil, and is what we will be discussing today. It’s also called “tulsi“, so if you see that name around, it is the same plant.
- Ocimum basilicum is the botanical name given to culinary basil, the kind you will find in your local supermarket. This one looks similar, but it has a different taste (culinary basil is sweeter) and a different phytochemical profile, and is certainly not the same plant.
We have touched on holy basil before, in our article:
Herbs For Evidence-Based Health & Healing
…where we listed that it helps boost immunity, per:
It’s popularly also consumed in the hopes of getting many other benefits, including:
- Calming effects on the mood (anti-stress)
- Accelerated wound-healing
- Anticancer activity
So, does it actually do those things?
Against stress
We literally couldn’t find anything. It’s often listed as being adaptogenic (reduces stress) in the preamble part of a given paper’s abstract, but we could find no study in any reputable journal that actually tested its effects against stress, and any citations for the claim just link to other papers that also include it in the preamble—and while “no original research” is a fine policy for, say, Wikipedia, it’s not a great policy when it comes to actual research science.
So… It might! There’s also no research (that we could find) showing that it doesn’t work. But one cannot claim something works on the basis of “we haven’t proved it doesn’t”.
For wound healing
Possibly! We found one (1) paper with a small (n=29) sample, and the results were promising, but that sample size of 29 was divided between three groups: a placebo control, holy basil, and another herb (which latter worked less well). So the resultant groups were tiny, arguably to the point of statistical insignificance. However, taking the study at face value and ignoring the small sample size, the results were very promising, as the holy basil group enjoyed a recovery in 4 weeks, rather than the 5 weeks recovery time of the control group:
Herbal remedies for mandibular fracture healing
An extra limitation that’s worth noting, though, is that healing bone is not necessarily the same as healing other injuries in all ways, so the same results might not be replicated in, say, organ or tissue injuries.
Against cancer
This time, there’s lots of evidence! Its mechanism of action appears to be severalfold:
- Anti-inflammatory
- Antioxidant
- Antitumor
- Chemopreventive
Because of the abundance of evidence (including specifically against skin cancer, lung cancer, breast cancer, and more), we could list studies all day here, but instead we’ll just link this one really good research review that has a handy navigation menu on the right, where you can see how it works in each of the stated ways.
Here’s the paper:
An Update on the Therapeutic Anticancer Potential of Ocimum sanctum L.: “Elixir of Life”
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
-
Undoing Creatine’s Puffiness Side Effect
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Creatine is known to increase “puffiness”, especially in my face. Are there any supplements that do the opposite?!❞
So first, let’s examine why this happens: creatine is most often taken to boost muscle size and performance. Your muscles are, of course, mostly water by mass, and so building your muscles requires extra water, which triggers systemic water retention.
In other words: you take creatine, exercise, and as the muscles start growing, the body goes “oh heck, we are running out of water, better save as much as possible in order to keep hydrating the muscles without running out” and starts putting it anywhere it can that’s not your bladder, so this will largely be the soft tissues of your body.
So, this results in classic water retentions symptoms including bloating and, yes, facial puffiness.
How much this happens, and how long the effects last, depend on three main things:
- What daily dose of creatine you are taking
- What kind of exercise you are doing
- What your hydration is like
The dose is relevant as it’s most common to get this puffiness during the “loading” phase, i.e. if you’re taking an increased dose to start with.
The exercise is relevant as it affects how much your body is actually using the water to build muscles.
The hydration is relevant because the less water you are taking, the more the body will try to retain whatever you do have.
This means, of course, that the supplement you are looking for to undo the facial puffiness is, in fact, water (even, nay, especially, if you feel bloated too):
Water For Everything? Water’s Counterintuitive Properties
Additionally, you could scale back the dose of creatine you’re taking, if you’re not currently doing heavy muscle-building exercise.
That said, the recommended dose for cognitive benefits is 5g/day, which is a very standard main-phase (i.e., post-loading) bodybuilding dose, so do with that information what you will.
See also: Creatine’s Brain Benefits Increase With Age
On which note: whether or not you want to take creatine for brain benefits, however, may depend on your age:
Creatine: Very Different For Young & Old People
Most research on creatine’s effects on humans has usually been either collegiate athletes or seniors, which leaves quite a research gap in the middle—so it’s unclear at what age the muscle-building effects begin to taper off, and at what age the cognitive benefits begin to take off.
Want a quicker fix?
If you want to reduce your facial puffiness acutely (e.g., you have a date in an hour and would like to not have a puffy face), then there are two things you can do that will help immediately, and/but only have short-term effects, meaning you’d have to do them daily to enjoy the results every day:
The first is an ice bath; simply fill a large bowl with water and ice cubes, give it a couple of minutes to get down to temperature, hold your breath and plunge your face in for as long as you can comfortably hold your breath. Repeat a few times, and towel off.
This helps by waking up the vasculature in your face, helping it to reduce puffiness naturally.
The second is facial yoga or guā shā, which is the practice of physically manipulating the soft tissues of your face to put them where you want them, rather than where you don’t want them. This will work against water retention puffiness, as well as cortisol puffiness, lymphatic puffiness, and more:
7-Minute Face Fitness For Lymphatic Drainage & Youthful Jawline
Enjoy!
Share This Post
-
Why STIs Are On The Rise In Older Adults
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Three Little Words
Sexually Transmitted Infections (STIs) are often thought of as something that predominantly plagues younger people… The truth, however, is different:
❝Rising divorce rates, forgoing condoms as there is no risk of pregnancy, the availability of drugs for sexual dysfunction, the large number of older adults living together in retirement communities, and the increased use of dating apps are likely to have contributed to the growing incidence of STIs in the over-50s.
These data likely underestimate the true extent of the problem as limited access to sexual health services for the over 50s, and trying to avoid the stigma and embarrassment both on the part of older people and healthcare professionals, is leading to this age group not seeking help for STIs.❞
Read more: Managing The Rise In STIs Among Older Adults
That said, there is a gender gap when it comes to the increased risk, for example:
❝A retrospective study from the USA involving 420,790 couples aged 67 to 99 years, found that widowhood was associated with an increased risk of STIs in older men, but not women❞
~ US Dept of Health & Human Services
Source: CDC: | Sexually Transmitted Disease Surveillance
Is abstinence the best preventative, then?
It is inarguably the most effective, but not necessarily the best for everyone.
This is because for most adults, a healthy sex life is an important part of overall wellbeing.
See also: Mythbusting The Big O
Even in this case there is a gender gap in:
- the level of importance placed on frequency of sexual interactions
- what act(s) of sexuality are held to be most important:
❝Among sexually active men, frequent (≥2 times a month) sexual intercourse (P < .001) and frequent kissing, petting, or fondling (P < .001) were associated with greater enjoyment of life.
Among sexually active women, frequent kissing, petting, or fondling was also associated with greater enjoyment of life (P < .001), but there was no significant association with frequent intercourse (P = .101).
Concerns about one’s sex life and problems with sexual function were strongly associated with lower levels of enjoyment of life in men and to a lesser extent in women.❞
Source: Sexual Activity is Associated with Greater Enjoyment of Life in Older Adults
If you have the time to go into it much more deeply, this paper from the Journal of Gerontology is much more comprehensive, looking also at related lifestyle factors, religious/political backgrounds, views on monogamy or non-monogamy (of various kinds), hormonal considerations, the impact of dementia or other long-term disabilities that may affect things, widowhood, and many other elements:
The National Social Life, Health, and Aging Project: An Introduction
What’s the best preventative, then?
Regular health screening for yourself and your partner(s) is an important key to preventative health when it comes to STIs.
You can Google search for a local STI clinic, and worry not, they are invariably discreet and are well-used to everybody coming in. They’re just glad you’re being responsible about things. It’s also not their job to judge your sexual activities, even if it’s something you might have reason to wish to be secretive about, try to be honest there.
Secondly, most of the usual advice about safe sex still goes, even when there’s no risk of pregnancy. For example, if there’s at least one penis involved, then condoms remain the #1 barrier to all manner of potential infections (we know, almost nobody likes condoms, but sometimes the truth isn’t what we want to hear).
Lastly, if there’s at least one vagina involved, then please for the love of all that is holey, do not put anything there that could cause a yeast infection.
What can cause a yeast infection? Pretty much anything with sugar, which includes but is not limited to:
- Most kinds of food that Cosmo-style “liven things up in the bedroom” advice columns might suggest using (including fruit, honey, chocolate sauce, whipped cream, etc)
- Hands that are not clean (watch out for bacteria too)
- A mouth that has recently been eating or drinking anything with sugar in it, and that includes many kinds of alcohol, as well as milk or hot drinks that had milk in
Yeast infections are not nearly so serious as the STIs the other measures are there to avoid, but they’re not fun either, so some sensible policies in that regard are always good!
On a related note, see also: How To Avoid UTIs
Recap on the single most important part of this article:
At all ages, it remains a good health practice—unless one is absolutely celibate—to regularly get oneself and one’s partner(s) checked for STIs.
Take care!
Share This Post
Related Posts
-
What is pathological demand avoidance – and how is it different to ‘acting out’?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Charlie” is an eight-year-old child with autism. Her parents are worried because she often responds to requests with insults, aggression and refusal. Simple demands, such as being asked to get dressed, can trigger an intense need to control the situation, fights and meltdowns.
Charlie’s parents find themselves in a constant cycle of conflict, trying to manage her and their own reactions, often unsuccessfully. Their attempts to provide structure and consequences are met with more resistance.
What’s going on? What makes Charlie’s behaviour – that some are calling “pathological demand avoidance” – different to the defiance most children show their parents or carers from time-to-time?
What is pathological demand avoidance?
British developmental psychologist Elizabeth Newson coined the term “pathological demand avoidance” (commonly shortened to PDA) in the 1980s after studying groups of children in her practice.
A 2021 systematic review noted features of PDA include resistance to everyday requests and strong emotional and behavioural reactions.
Children with PDA might show obsessive behaviour, struggle with persistence, and seek to control situations. They may struggle with attention and impulsivity, alongside motor and coordination difficulties, language delay and a tendency to retreat into role play or fantasy worlds.
PDA is also known as “extreme demand avoidance” and is often described as a subtype of autism. Some people prefer the term persistent drive for autonomy or pervasive drive for autonomy.
What does the evidence say?
Every clinician working with children and families recognises the behavioural profile described by PDA. The challenging question is why these behaviours emerge.
PDA is not currently listed in the two diagnostic manuals used in psychiatry and psychology to diagnose mental health and developmental conditions, the current Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the World Health Organization’s International Classification of Diseases (ICD-11).
Researchers have reported concerns about the science behind PDA. There are no clear theories or explanations of why or how the profile of symptoms develop, and little inclusion of children or adults with lived experience of PDA symptoms in the studies. Environmental, family or other contextual factors that may contribute to behaviour have not been systematically studied.
A major limitation of existing PDA research and case studies is a lack of consideration of overlapping symptoms with other conditions, such as autism, attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder, anxiety disorder, selective mutism and other developmental disorders. Diagnostic labels can have positive and negative consequences and so need to be thoroughly investigated before they are used in practice.
Classifying a “new” condition requires consistency across seven clinical and research aspects: epidemiological data, long-term patient follow-up, family inheritance, laboratory findings, exclusion from other conditions, response to treatment, and distinct predictors of outcome. At this stage, these domains have not been established for PDA. It is not clear whether PDA is different from other formal diagnoses or developmental differences.
When a child is stressed, demands or requests might tip them into fight, flight or freeze mode. Shutterstock Finding the why
Debates over classification don’t relieve distress for a child or those close to them. If a child is “intentionally” engaged in antisocial behaviour, the question is then “why?”
Beneath the behaviour is almost always developmental difference, genuine distress and difficulty coping. A broad and deep understanding of developmental processes is required.
Interestingly, while girls are “under-represented” in autism research, they are equally represented in studies characterising PDA. But if a child’s behaviour is only understood through a “pathologising” or diagnostic lens, there is a risk their agency may be reduced. Underlying experiences of distress, sensory overload, social confusion and feelings of isolation may be missed.
So, what can be done to help?
There are no empirical studies to date regarding PDA treatment strategies or their effectiveness. Clinical advice and case studies suggest strategies that may help include:
- reducing demands
- giving multiple options
- minimising expectations to avoid triggering avoidance
- engaging with interests to support regulation.
Early intervention in the preschool and primary years benefits children with complex developmental differences. Clinical care that involves a range of medical and allied health clinicians and considers the whole person is needed to ensure children and families get the support they need.
It is important to recognise these children often feel as frustrated and helpless as their caregivers. Both find themselves stuck in a repetitive cycle of distress, frustration and lack of progress. A personalised approach can take into account the child’s unique social, sensory and cognitive sensitivities.
In the preschool and early primary years, children have limited ability to manage their impulses or learn techniques for managing their emotions, relationships or environments. Careful watching for potential triggers and then working on timetables and routines, sleep, environments, tasks, and relationships can help.
As children move into later primary school and adolescence, they are more likely to want to influence others and be able to have more self control. As their autonomy and ability to collaborate increases, the problematic behaviours tend to reduce.
Strategies that build self-determination are crucial. They include opportunities for developing confidence, communication and more options to choose from when facing challenges. This therapeutic work with children and families takes time and needs to be revisited at different developmental stages. Support to engage in school and community activities is also needed. Each small step brings more capacity and more effective ways for a child to understand and manage themselves and their worlds.
What about Charlie?
The current scope to explain and manage PDA is limited. Future research must include the voices and views of children and adults with PDA symptoms.
Such emotional and behavioural difficulties are distressing and difficult for children and families. They need compassion and practical help.
For a child like Charlie, this could look like a series of sessions where she and her parents meet with clinicians to explore Charlie’s perspective, experiences and triggers. The family might come to understand that, in addition to autism, Charlie has complex developmental strengths and challenges, anxiety, and some difficulties with adjustment related to stress at home and school. This means Charlie experiences a fight, flight, freeze response that looks like aggression, avoidance or shutting down.
With carefully planned supports at home and school, Charlie’s options can broaden and her distress and avoidance can soften. Outside the clinic room, Charlie and her family can be supported to join an inclusive local community sporting or creative activity. Gradually she can spend more time engaged at home, school and in the community.
Nicole Rinehart, Professor, Child and Adolescent Psychology, Director, Krongold Clinic (Research), Monash University; David Moseley, Senior Research Fellow, Deputy Director (Clinical), Monash Krongold Clinic, Monash University, and Michael Gordon, Associate Professor, Psychiatry, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Brain Benefits in 3 Months…through walking?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Keeping it Simple
Today’s video (below) is another Big Think production (can you tell that we love their work?). Wendy Suzuki does a wonderful job of breaking down the brain benefits of exercise into three categories, within three minutes.
The first question to ask yourself is: what is your current level of fitness?
Low Fitness
Exercising, even if it’s just going on a walk, 2-3 times a week improves baseline mood state, as well as enhances prefrontal and hippocampal function. These areas of the brain are crucial for complex behaviors like planning and personality development, as well as memory and learning.
Mid Fitness
The suggested regimen is, without surprise, to slightly increase your regular workouts over three months. Whilst you’re already getting the benefits from the low-fitness routine, there is a likelihood that you’ll increase your baseline dopamine and serotonin levels–which, of course, we love! Read more on dopamine here, here, or here.
High Fitness
If you consider yourself in the high fitness bracket then well done, you’re doing an amazing job! Wendy Suzuki doesn’t make many suggestions for you; all she mentions is that there is the possibility of “too much” exercise actually having negative effects on the brain. However, if you’re not competing at an Olympic level, you should be fine.
Fitness and Exercise in General
Of course, fitness and exercise are both very broad terms. We would suggest that you find an exercise routine that you genuinely enjoy–something that is easy to continue over the long term. Try browsing different areas of exercise to see what resonates with you. For instance, Total Fitness After 40 is a great book on all things fitness in the second half of your life. Alternatively, search through our archive for fitness-related material.
Anyway, without further ado, here is today’s video:
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
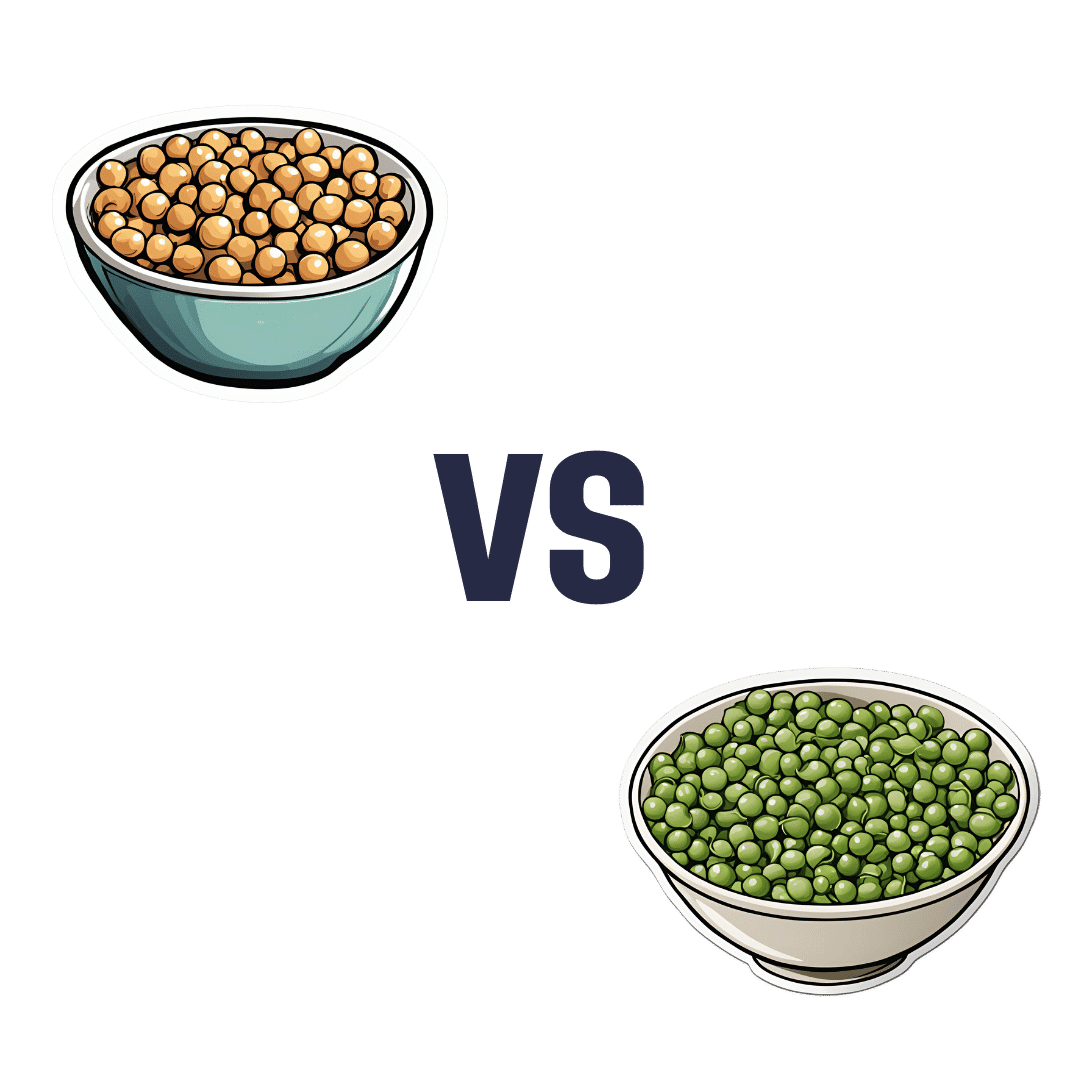
Chickpeas vs Peas – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chickpeas to peas, we picked the chickpeas.
Why?
Both are great! But…
In terms of macros, chickpeas have more protein, fiber, and carbs, the ratio of which latter two also gives them the lower glycemic index. It’s worth noting that peas are not far behind chickpeas here, but by the numbers, it’s a win for chickpeas in this category.
In the category of vitamins, chickpeas have more of vitamins B9, E, and choline, while peas have more of vitamins A, B1, B2, B3, B5, B6, C, and K. So, a win for peas this time!
When it comes to minerals, however, chickpeas have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while peas are not higher in any minerals.
Adding up the sections gives a 2:1 victory for chickpeas, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Plant vs Animal Protein: Head to Head
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: