Brothy Beans & Greens
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Eat beans and greens”, we say, “but how”, you ask. Here’s how! Tasty, filling, and fulfilling, this dish is full of protein, fiber, vitamins, minerals, and assorted powerful phytochemicals.
You will need
- 2½ cups low-sodium vegetable stock
- 2 cans cannellini beans, drained and rinsed
- 1 cup kale, stems removed and roughly chopped
- 4 dried shiitake mushrooms
- 2 shallots, sliced
- ½ bulb garlic, crushed
- 1 tbsp white miso paste
- 1 tbsp nutritional yeast
- 1 tsp rosemary leaves
- 1 tsp thyme leaves
- 1 tsp black pepper, coarse ground
- ½ tsp red chili flakes
- Juice of ½ lemon
- Extra virgin olive oil
- Optional: your favorite crusty bread, perhaps using our Delicious Quinoa Avocado Bread recipe
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a skillet and fry the shallots for 2–3 minutes.
2) Add the nutritional yeast, garlic, herbs, and spices, and stir for another 1 minute.
3) Add the beans, vegetable stock, and mushrooms. Simmer for 10 minutes.
4) Add the miso paste, stirring well to dissolve and distribute evenly.
5) Add the kale until it begins to wilt, and remove the pot from the heat.
6) Add the lemon juice and stir.
7) Serve; we recommend enjoying it with crusty wholegrain bread.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Dr. Greger’s Daily Dozen ← beans and greens up top!
- The Magic of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Alzheimer’s Risk Reduction Methods
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Q: I am now in the “aging” population. A great concern for me is Alzheimers. My father had it and I am so worried. What is the latest research on prevention?
Very important stuff! We wrote about this not long back:
- See: How To Reduce Your Alzheimer’s Risk
- See also: Brain Food? The Eyes Have It!
(one good thing to note is that while Alzheimer’s has a genetic component, it doesn’t appear to be hereditary per se. Still, good to be on top of these things, and it’s never too early to start with preventive measures!)
Share This Post
-
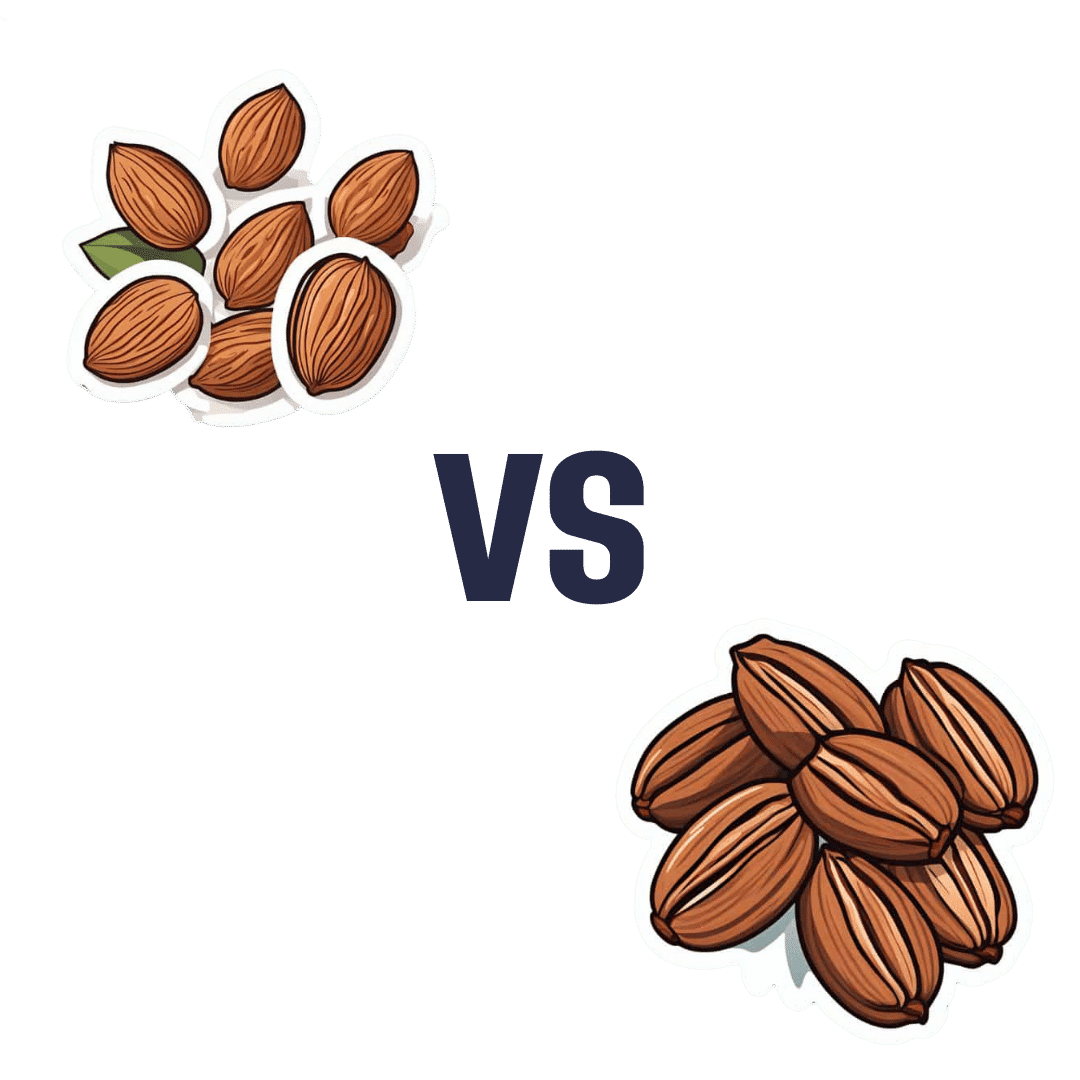
Almonds vs Pecans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing almonds to pecans, we picked the almonds.
Why?
In terms of macros, almonds have more protein, carbs, and fiber, as well as the lower glycemic index. A strong start for almonds here, though pecans have more fat (and the healthy blend of fats is quite comparable from one nut to the other).
In the category of vitamins, almonds have more of vitamins B2, B3, B9, E, and choline, while pecans have more of vitamins A, B1, B5, B6, and K. Numerically that’s a tie, though the biggest margins of difference are for vitamins A and E, respectively, and we might want to prioritize almonds’ extra vitamin E, over pecans’ extra vitamin A, given that vitamin A is more easily found in large quantities in many foods, whereas vitamin E is not quite so abundant generally. So in short, either a tie or a slight win for almonds here.
When it comes to minerals, both contain a lot of goodness, but almonds have more calcium, iron, magnesium, phosphorus, potassium, and selenium, while pecans have more copper, manganese, and zinc. A clear win for almonds, though as we say, pecans are also great for this, just not as great as almonds.
As a side-note, both of these nuts have been found to have anticancer properties against breast cancer cell lines. In all likelihood this means they help against other cancers too, but breast cancer is what the extant research has been for.
So, naturally, enjoy either or both (in fact, both is ideal). But if you want to choose one for nutritional density, it’s almonds.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Share This Post
-
Here’s how to help protect your family from norovirus
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- Norovirus is a very contagious infection that causes vomiting and diarrhea.
- The best way to help protect against norovirus is to wash your hands often with soap and warm water, since hand sanitizer may not be effective at killing the virus.
- If someone in your household has symptoms of norovirus, isolate them away from others, watch for signs of dehydration, and take steps to help prevent it from spreading.
If you feel like everyone is sick right now, you’re not alone. Levels of respiratory illnesses like COVID-19, flu, and RSV remain remain high in many states, and the U.S. is also battling a wave of norovirus, one of several viruses that cause a very contagious infection of the stomach and intestines.
Although norovirus infections are more common during the colder months—it’s also called the “winter vomiting disease”—the virus can spread at any time. Right now, however, cases have more than doubled since last year’s peak.
Read on to learn about the symptoms of norovirus, how it spreads, and what to do if someone in your household gets sick.
What are the symptoms of norovirus?
Norovirus is a very contagious infection that causes vomiting and diarrhea, which typically begins 12 to 48 hours after exposure to the virus. Additional symptoms may include stomach pain, body aches, headaches, and a fever. Norovirus typically resolves within three days, but people who are infected may still be contagious for up to two days after symptoms resolve.
Norovirus may cause dehydration, or a dangerous loss of fluids, especially in young children and older adults. See a health care provider if you or someone in your household shows signs of dehydration, which may include decreased urination, dizziness, a dry mouth and throat, sleepiness, and crying without tears.
How can you help protect against norovirus?
You can get norovirus if you have close contact with someone who is infected, touch a contaminated surface and then touch your mouth or nose, or consume contaminated food or beverages.
The best way to help protect yourself and others against norovirus is to wash your hands often with soap and warm water, since hand sanitizer may not be effective at killing the virus. Other ways to help protect yourself may include cooking food thoroughly and washing fruits and vegetables before eating them.
You can get sick with norovirus even if you’ve had it before, since there are many different strains.
How can families help protect against the spread of norovirus at home?
If someone in your household has symptoms of norovirus, isolate them away from others and watch for signs of dehydration. If you are sick with norovirus, do not prepare food for others in your household and use a separate bathroom, if possible.
When cleaning up after someone who has norovirus, wear rubber, latex, or nitrile gloves. Then wash your hands thoroughly.
Clean surfaces using a solution containing five to 25 tablespoons of bleach (that’s 12.5 fluid ounces, or just over ¾ cup), per gallon of water. Leave the bleach-water mix on surfaces for at least five minutes before wiping it off.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Is Fast Food Really All That Bad?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Yes, yes it is. However, most people misunderstand the nature of its badness, which is what causes problems. The biggest problem is not the acute effects of one afternoon’s burger and fries; the biggest problem is the gradual slide into regularly eating junk food, and the long-term effects of that habit as our body changes to accommodate it (of which, people tend to focus on subcutaneous fat gain as it’s usually the most visible, but that’s really the least of our problems).
Cumulative effects
There are, of course, immediate negative effects too, and they’re not without cause for concern. Because of the composition of most junk food, it will almost by definition result in immediate blood sugar spikes, rising insulin levels, and a feeling of fatigue not long afterwards.
- Within a week of regularly consuming junk food, gut bacteria will change, resulting in moderate cravings, as well as a tendency towards depression and anxiety. Mood swings are likely, as are the gastrointestinal woes associated with any gut microbiota change.
- Within two weeks, those effects will be greater, the cravings will increase, energy levels will plummet, and likely skin issues may start to show up (our skin mostly works on a 3-week replacement cycle; some things can show up in the skin more quickly or slowly than that, though).
- Within three weeks, the rest of our blood metrics (e.g. beyond blood sugar imbalances) will start to stray from safe zones. Increased LDL, decreased HDL, and the beginnings of higher cardiovascular disease risk and diabetes risk.
- Within a month, we will likely see the onset of non-alcoholic fatty liver disease, and chronic inflammation sets in, raising the risk of a lot of other diseases, especially immune disorders and cancer.
If that seems drastic, along the lines of “eat junk food for a month and get cancer”, well, it’s an elevated risk, not a scheduled diagnosis, but the body is constantly rebuilding itself, for better or for worse, and if we sabotage its efforts by consuming a poor diet, then it will be for worse.
The good news is: this works both ways, and we can get our body back on track in fairly short order too, by enjoying a healthier diet; our body will be thrilled to start repairing itself. And of course, all these effects, good and bad, are proportional to how well or badly we eat. There’s a difference between doing a “Supersize Me” month-long 100% junk food diet, and “merely” getting a junk food breakfast each day and eating healthily later.
In short, if your diet is only moderately bad, then you will only be moderately unwell.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Fix Chronic Fatigue & Regain Your Energy, By Science
- How To Unfatty A Fatty Liver
- How to Prevent (or Reduce) Inflammation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Artichoke vs Broccoli – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing artichoke to broccoli, we picked the artichoke.
Why?
Both have their strengths, and it was close! But…
In terms of macros, artichoke has about 2x the fiber (which is lots, because broccoli is already good for this) and more protein, for only slightly more carbs, making it the nutrient dense choice in all respects, and especially in the case of fiber.
In the category of vitamins, artichoke has more of vitamins B3, B9, and choline, while broccoli has more of vitamins A, B2, B5, B6, C, E, and K, thus winning this round.
When it comes to minerals, artichoke has more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc, while broccoli has more calcium and selenium, handing artichoke the win again here.
Looking at polyphenols, both have an abundance; artichoke has more by total mass (in terms of mg/100g) and is especially rich in luteolin and phenolic acids, but broccoli has some that artichoke doesn’t have (such as quercetin and kaempferol). We could reasonably call this a tie or a win for artichoke on strength of numbers; either way, it doesn’t change the end result:
Adding up the sections makes for an overall win for artichoke, but of course, by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
154 million lives saved in 50 years: 5 charts on the global success of vaccines
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We know vaccines have been a miracle for public health. Now, new research led by the World Health Organization has found vaccines have saved an estimated 154 million lives in the past 50 years from 14 different diseases. Most of these have been children under five, and around two-thirds children under one year old.
In 1974 the World Health Assembly launched the Expanded Programme on Immunization with the goal to vaccinate all children against diphtheria, tetanus, pertussis (whooping cough), measles, polio, tuberculosis and smallpox by 1990. The program was subsequently expanded to include several other diseases.
The modelling, marking 50 years since this program was established, shows a child aged under ten has about a 40% greater chance of living until their next birthday, compared to if we didn’t have vaccines. And these positive effects can be seen well into adult life. A 50-year-old has a 16% greater chance of celebrating their next birthday thanks to vaccines.
What the study did
The researchers developed mathematical and statistical models which took in vaccine coverage data and population numbers from 194 countries for the years 1974–2024. Not all diseases were included (for example smallpox, which was eradicated in 1980, was left out).
The analysis includes vaccines for 14 diseases, with 11 of these included in the Expanded Programme on Immunization. For some countries, additional vaccines such as Japanese encephalitis, meningitis A and yellow fever were included, as these diseases contribute to major disease burden in certain settings.
The models were used to simulate how diseases would have spread from 1974 to now, as vaccines were introduced, for each country and age group, incorporating data on increasing vaccine coverage over time.
Children are the greatest beneficiaries of vaccines
Since 1974, the rates of deaths in children before their first birthday has more than halved. The researchers calculated almost 40% of this reduction is due to vaccines.
The effects have been greatest for children born in the 1980s because of the intensive efforts made globally to reduce the burden of diseases like measles, polio and whooping cough.
Some 60% of the 154 million lives saved would have been lives lost to measles. This is likely due to its ability to spread rapidly. One person with measles can spread the infection to 12–18 people.
The study also found some variation across different parts of the world. For example, vaccination programs have had a much greater impact on the probability of children living longer across low- and middle-income countries and settings with weaker health systems such as the eastern Mediterranean and African regions. These results highlight the important role vaccines play in promoting health equity.
Vaccine success is not assured
Low or declining vaccine coverage can lead to epidemics which can devastate communities and overwhelm health systems.
Notably, the COVID pandemic saw an overall decline in measles vaccine coverage, with 86% of children having received their first dose in 2019 to 83% in 2022. This is concerning because very high levels of vaccination coverage (more than 95%) are required to achieve herd immunity against measles.
In Australia, the coverage for childhood vaccines, including measles, mumps and rubella, has declined compared to before the pandemic.
This study is a reminder of why we need to continue to vaccinate – not just against measles, but against all diseases we have safe and effective vaccines for.
The results of this research don’t tell us the full story about the impact of vaccines. For example, the authors didn’t include data for some vaccines such as COVID and HPV (human papillomavirus). Also, like with all modelling studies, there are some uncertainties, as data was not available for all time periods and countries.
Nonetheless, the results show the success of global vaccination programs over time. If we want to continue to see lives saved, we need to keep investing in vaccination locally, regionally and globally.
Meru Sheel, Associate Professor and Epidemiologist, Infectious Diseases, Immunisation and Emergencies Group, Sydney School of Public Health, University of Sydney and Alexandra Hogan, Mathematical epidemiologist, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: