Grains: Bread Of Life, Or Cereal Killer?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Going Against The Grain?
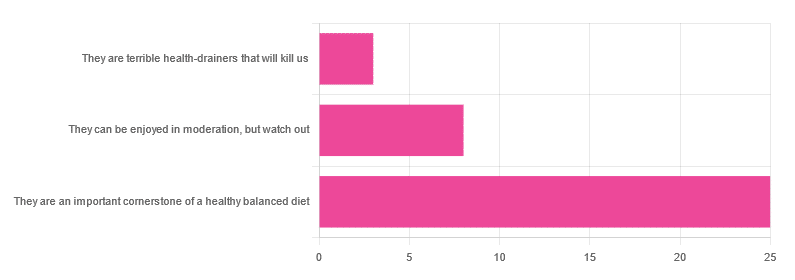
In Wednesday’s newsletter, we asked you for your health-related opinion of grains (aside from any gluten-specific concerns), and got the above-depicted, below-described, set of responses:
- About 69% said “They are an important cornerstone of a healthy balanced diet”
- About 22% said “They can be enjoyed in moderation, but watch out”
- About 8% said “They are terrible health-drainers that will kill us”
So, what does the science say?
They are terrible health-drainers that will kill us: True or False?
True or False depending on the manner of their consumption!
There is a big difference between the average pizza base and a bowl of oats, for instance. Or rather, there are a lot of differences, but what’s most critical here?
The key is: refined and ultraprocessed grains are so inferior to whole grains as to be actively negative for health in most cases for most people most of the time.
But! It’s not because processing is ontologically evil (in reality: some processed foods are healthy, and some unprocessed foods are poisonous). although it is a very good general rule of thumb.
So, we need to understand the “why” behind the “key” that we just gave above, and that’s mostly about the resultant glycemic index and associated metrics (glycemic load, insulin index, etc).
In the case of refined and ultraprocessed grains, our body gains sugar faster than it can process it, and stores it wherever and however it can, like someone who has just realised that they will be entertaining a houseguest in 10 minutes and must tidy up super-rapidly by hiding things wherever they’ll fit.
And when the body tries to do this with sugar from refined grains, the result is very bad for multiple organs (most notably the liver, but the pancreas takes quite a hit too) which in turn causes damage elsewhere in the body, not to mention that we now have urgently-produced fat stored in unfortunate places like our liver and abdominal cavity when it should have gone to subcutaneous fat stores instead.
In contrast, whole grains come with fiber that slows down the absorption of the sugars, such that the body can deal with them in an ideal fashion, which usually means:
- using them immediately, or
- storing them as muscle glycogen, or
- storing them as subcutaneous fat
👆 that’s an oversimplification, but we only have so much room here.
For more on this, see:
Glycemic Index vs Glycemic Load vs Insulin Index
And for why this matters, see:
Which Sugars Are Healthier, And Which Are Just The Same?
And for fixing it, see:
They can be enjoyed in moderation, but watch out: True or False?
Technically True but functionally False:
- Technically true: “in moderation” is doing a lot of heavy lifting here. One person’s “moderation” may be another person’s “abstemiousness” or “gluttony”.
- Functionally false: while of course extreme consumption of pretty much anything is going to be bad, unless you are Cereals Georg eating 10,000 cereals each day and being a statistical outlier, the issue is not the quantity so much as the quality.
Quality, we discussed above—and that is, as we say, paramount. As for quantity however, you might want to know a baseline for “getting enough”, so…
They are an important cornerstone of a healthy balanced diet: True or False?
True! This one’s quite straightforward.
3 servings (each being 90g, or about ½ cup) of whole grains per day is associated with a 22% reduction in risk of heart disease, 5% reduction in all-cause mortality, and a lot of benefits across a lot of disease risks:
❝This meta-analysis provides further evidence that whole grain intake is associated with a reduced risk of coronary heart disease, cardiovascular disease, and total cancer, and mortality from all causes, respiratory diseases, infectious diseases, diabetes, and all non-cardiovascular, non-cancer causes.
These findings support dietary guidelines that recommend increased intake of whole grain to reduce the risk of chronic diseases and premature mortality.❞
~ Dr. Dagfinn Aune et al.
We’d like to give a lot more sources for the same findings, as well as papers for all the individual claims, but frankly, there are so many that there isn’t room. Suffice it to say, this is neither controversial nor uncertain; these benefits are well-established.
Here’s a very informative pop-science article, that also covers some of the things we discussed earlier (it shows what happens during refinement of grains) before getting on to recommendations and more citations for claims than we can fit here:
Harvard School Of Public Health | Whole Grains
“That’s all great, but what if I am concerned about gluten?”
There certainly are reasons you might be, be it because of a sensitivity, allergy, or just because perhaps you’d like to know more.
Let’s first mention: not all grains contain gluten, so it’s perfectly possible to enjoy naturally gluten-free grains (such as oats and rice) as well as gluten-free pseudocereals, which are not actually grains but do the same job in culinary and nutritional terms (such as quinoa and buckwheat, despite the latter’s name).
Finally, if you’d like to know more about gluten’s health considerations, then check out our previous mythbusting special:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Do We Need Supplements, And Do They Work?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Does our diet need a little help?
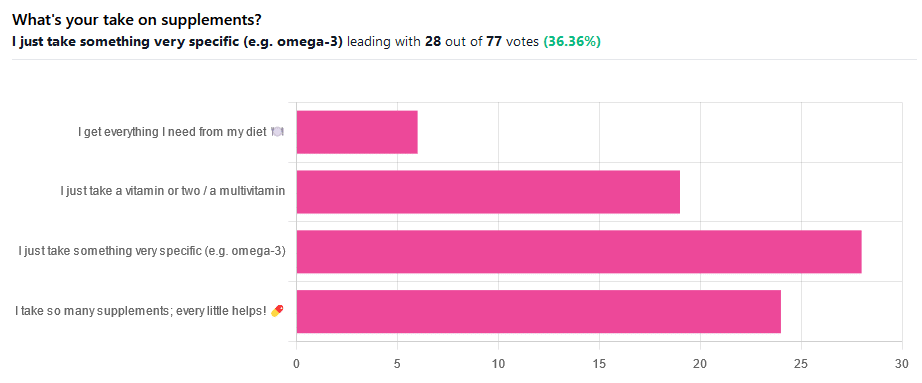
We asked you for your take on supplements, and got the above-illustrated, below-described set of results.
- The largest minority of respondents (a little over a third) voted for “I just take something very specific”
- The next most respondents voted for “I take so many supplements; every little helps!”
- Almost as many voted for “I just take a vitamin or two / a multivitamin”
- Fewest, about 8%, voted for “I get everything I need from my diet”
But what does the science say?
Food is less nutritious now than it used to be: True or False?
True or False depending on how you measure it.
An apple today and an apple from a hundred years ago are likely to contain the same amounts of micronutrients per apple, but a lower percentage of micronutrients per 100g of apple.
The reason for this is that apples (and many other food products; apples are just an arbitrary example) have been selectively bred (and in some cases, modified) for size, and because the soil mineral density has remained the same, the micronutrients per apple have not increased commensurate to the increase in carbohydrate weight and/or water weight. Thus, the resultant percentage will be lower, despite the quantity remaining the same.
We’re going to share some science on this, and/but would like to forewarn readers that the language of this paper is a bit biased, as it looks to “debunk” claims of nutritional values dropping while skimming over “yes, they really have dropped percentage-wise” in favor of “but look, the discrete mass values are still the same, so that’s just a mathematical illusion”.
The reality is, it’s no more a mathematical illusion than is the converse standpoint of saying the nutritional value is the same, despite the per-100g values dropping. After all, sometimes we eat an apple as-is; sometimes we buy a bag of frozen chopped fruit. That 500g bag of chopped fruit is going to contain less copper (for example) than one from decades past.
Here’s the paper, and you’ll see what we mean:
Supplements aren’t absorbed properly and thus are a waste of money: True or False?
True or False depending on the supplement (and your body, and the rest of your diet)
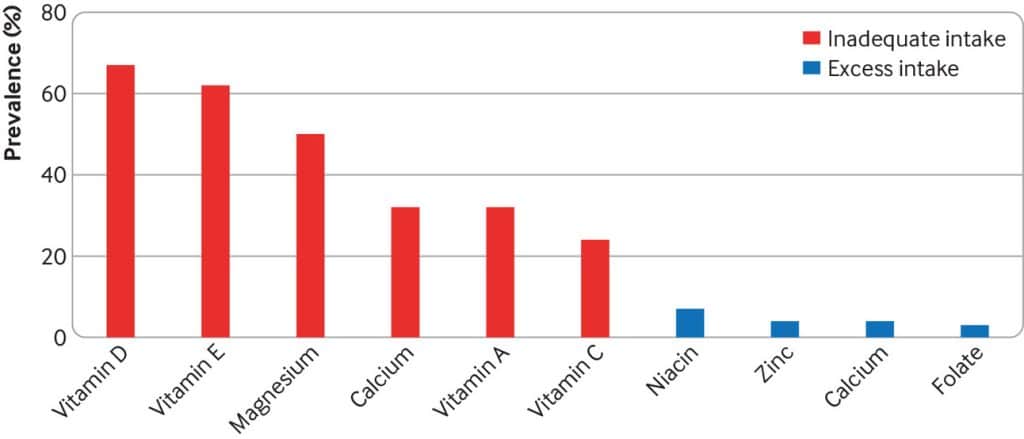
Many people are suffering from dietary deficiencies of vitamins and minerals, that could be easily correctable by supplementation:
However, as this study by Dr. Fang Fang Zhang shows, a lot of vitamin and mineral supplementation does not appear to have much of an effect on actual health outcomes, vis-à-vis specific diseases. She looks at:
- Cardiovascular disease
- Cancer
- Type 2 diabetes
- Osteoporosis
Her key take-aways from this study were:
- Randomised trial evidence does not support use of vitamin, mineral, and fish oil supplements to reduce the risk of non-communicable diseases
- People using supplements tend to be older, female, and have higher education, income, and healthier lifestyles than people who do not use them
- Use of supplements appreciably reduces the prevalence of inadequate intake for most nutrients but also increases the prevalence of excess intake for some nutrients
- Further research is needed to assess the long term effects of supplements on the health of the general population and in individuals with specific nutritional needs, including those from low and middle income countries
Read her damning report: Health effects of vitamin and mineral supplements
On the other hand…
This is almost entirely about blanket vitamin-and-mineral supplementation. With regard to fish oil supplementation, many commercial fish oil supplements break down in the stomach rather than the intestines, and don’t get absorbed well. Additionally, many people take them in forms that aren’t pleasant, and thus result in low adherence (i.e., they nominally take them, but in fact they just sit on the kitchen counter for a year).
One thing we can conclude from this is that it’s good to check the science for any given supplement before taking it, and know what it will and won’t help for. Our “Monday Research Review” editions of 10almonds do this a lot, although we tend to focus on herbal supplements rather than vitamins and minerals.
We can get everything we need from our diet: True or False?
Contingently True (but here be caveats)
In principle, if we eat the recommended guideline amounts of various macro- and micro-nutrients, we will indeed get all that we are generally considered to need. Obviously.
However, this may come with:
- Make sure to get enough protein… Without too much meat, and also without too much carbohydrate, such as from most plant sources of protein
- Make sure to get enough carbohydrates… But only the right kinds, and not too much, nor at the wrong time, and without eating things in the wrong order
- Make sure to get enough healthy fats… Without too much of the unhealthy fats that often exist in the same foods
- Make sure to get the right amount of vitamins and minerals… We hope you have your calculators out to get the delicate balance of calcium, magnesium, potassium, phosphorus, and vitamin D right.
That last one’s a real pain, by the way. Too much or too little of one or another and the whole set start causing problems, and several of them interact with several others, and/or compete for resources, and/or are needed for the others to do their job.
And, that’s hard enough to balance when you’re taking supplements with the mg/µg amount written on them, never mind when you’re juggling cabbages and sardines.
On the topic of those sardines, don’t forget to carefully balance your omega-3, -6, and -9, and even within omega-3, balancing ALA, EPA, and DHA, and we hope you’re juggling those HDL and LDL levels too.
So, when it comes to getting everything we need from our diet, for most of us (who aren’t living in food deserts and/or experiencing food poverty, or having a medical condition that restricts our diet), the biggest task is not “getting enough”, it’s “getting enough of the right things without simultaneously overdoing it on the others”.
With supplements, it’s a lot easier to control what we’re putting in our bodies.
And of course, unless our diet includes things that usually can’t be bought in supermarkets, we’re not going to get the benefits of taking, as a supplement, such things as:
Etc.
So, there definitely are supplements with strong science-backed benefits, that probably can’t be found on your plate!
Share This Post
-
The Secret to Mental Health – by George Pransky
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book (and its author) have a sizeable popular following, so it definitely can be said that it has been well-received by many people. The premise in this book is that there is fundamentally nothing wrong with anybody’s brain, and rather everything can be broken down into:
- Mind (the energy and intelligence that animates all life)
- Consciousness (the capacity to be aware of one’s life and experiences)
- Thought (the ability to think, allowing individuals to create their personal experience of reality)
The author explains, over the course of 145 pages, that where anyone with any perceived mental health issue is going wrong is by either lacking self-awareness (Consciousness) or erring by creating an undesirable personal experience of reality (Thought).
In terms of the science of this, frequent references are made to “there is evidence that shows”, “new discoveries about mental health suggest…”, etc, but this claimed evidence is never actually presented, just alluded to. Where many books would have a bibliography, this one has simply a collection of what the author has titled “interesting case studies, conversations, papers, and discussions” (there are no actual case studies or papers; it is just a collection of anecdotes).
The style is… Honestly, in this reviewer’s opinion, barely readable. But, apparently lots of people love it, so your mileage may vary.
We don’t usually delve too far into claimed credentials, but because of the interesting writing style and the bold claims without evidence, we were curious as to where this PhD came from, and apparently it came from a now-shut-down diploma mill that was described by the court as “a complete scam”.
Bottom line: we can’t recommend this one, but we read it so that you don’t have to, and we hope that publishing this review will help reassure you that when we do recommend a book, we mean it!
Share This Post
-
Ice Cream vs Fruit Sorbet – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing ice cream to fruit sorbet, we picked the ice cream.
Why?
Well, neither are great!
But the deciding factor is simple: ice cream has more nutrients to go with its sugar.
While “fruit is good” is a very reliable truism in and of itself, sorbet tends to be made with fruit juice (or at best, purée, which for these purposes is more or less the same) and sugar. The small vitamin content is nowhere near enough to make up for this. The fiber having been removed by juicing or puréeing, the fruit juice with added sugar is basically shooting glucose and fructose into your veins while doing little else.
Fruit juice (even freshly-pressed) is nowhere near in the same league of healthiness as actual fruit!
See also: Which Sugars Are Healthier, And Which Are Just The Same?
Ice cream, meanwhile, is also not exactly a health food. But it has at least some minerals worth speaking of (mostly: calcium, potassium, phosphorus), and some fat that a) can be used b) helps slightly slow the absorption of the sugars.
In short: please do not consider either of these things to be a health food. But if you’re going to choose one or the other (and are not lactose-intolerant), then ice cream has some small positives to go with its negatives.
Take care!
Share This Post
Related Posts
-
Shoe Wear Patterns: What They Mean, Why It Matters, & How To Fix It
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you look under your shoes, do you notice how the tread is worn more in some places than others? Specific patterns of shoe wear correspond to how our body applies force, weight, and rotational movement. This reveals how we move, and uneven wear can indicate problematic movement dynamics.
The clues in your shoes
Common shoe wear patterns include:
- Diagonal wear on the outside of the heel: caused by foot angle, leg position, and instability, leading to joint stress.
- Rotational wear at specific points: due to internal or external rotation, often originating from the hip, pelvis, or torso.
- Wear above the big toe: caused by excessive toe lifting, often associated with a “lighter” or kicking leg.
Fixing movement issues to prevent wear involves correcting posture, improving balance, and adjusting how the legs land during walking/running.
Key fixes include:
- Aligning the center of gravity properly to prevent leg overcompensation.
- Ensuring feet land under the hips and not far in front.
- Stabilizing the torso to avoid unnecessary rotation.
- Engaging the glutes effectively to reduce hip flexor dominance and improve leg mechanics.
- Maintaining even weight distribution on both legs to prevent excessive lifting or twisting.
Posture and walking mechanics are vital to reducing uneven wear, but meaningful, lasting change takes time and focused effort, to build new habits.
For more on all this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Steps For Keeping Your Feet A Healthy Foundation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Painkilling Power Of Opioids, Without The Harm?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to painkilling medications, they can generally be categorized into two kinds:
- non-opioids (e.g. ibuprofen, paracetamol/acetaminophen, aspirin)
- ones that actually work for something more serious than a headache
That’s an oversimplification, but broadly speaking, when there is serious painkilling to be done, that’s when doctors consider it’s time to break out the opioids.
Nor are all opioids created equal—there’s a noteworthy difference between codeine and morphine, for instance—but the problems of opioids are typically the same (tolerance, addiction, and eventual likelihood of overdose when one tries to take enough to make it work after developing a tolerance), and it becomes simply a matter of degree.
See also: I’ve been given opioids after surgery to take at home. What do I need to know?
So, what’s the new development?
A team of researchers have found that the body can effectively produce its own targetted painkilling peptides, similar in function to benzodiazepines (an opioid drug), but—and which is a big difference—confined to the peripheral nervous system (PNS), meaning that it doesn’t enter the brain.
- The peptides killing the pain before it can reach the brain is obviously good because that means the pain is simply not experienced
- The peptides not having any effect on the brain, however, means that the mechanism of addiction of opioids simply does not apply here
- The peptides not having any effect on the brain also means that the CNS can’t be “put to sleep” by these peptides in the same way it can if a high dose of opioids is taken (this is what typically causes death in opioid overdoses; the heart simply beats too slowly to maintain life)
The hope, therefore, is to now create medications that target the spinal ganglia that produce these peptides, to “switch them on” at will.
Obviously, this won’t happen overnight; there will need to be first a lot of research to find a drug that does that (likely this will involve a lot of trial and error and so many mice/rats), and then multiple rounds of testing to ascertain that the drug is safe and effective for humans, before it can then be rolled out commercially.
But, this is still a big breakthrough; there arguably hasn’t been a breakthrough this big in pain research since various opioid-related breakthroughs in the 70s and 80s.
You can see a pop-science article about it here:
And you can see the previous research (from earlier this year) that this is now building from, about the glial cells in the spinal ganglia, here:
Peripheral gating of mechanosensation by glial diazepam binding inhibitor
But wait, there’s more!
Remember what we said about affecting the PNS without affecting the CNS, to kill the pain without killing the brain?
More researchers are already approaching the same idea to deal with the same problem, but from the angle of gene therapy, and have already had some very promising results with mice:
Structure-guided design of a peripherally restricted chemogenetic system
…which you can read about in pop-science terms (with diagrams!) here:
New gene therapy could alleviate chronic pain, researchers find
While you’re waiting…
In the meantime, approaches that are already available include:
- The 7 Approaches To Pain Management
- Managing Chronic Pain (Realistically!)
- Science-Based Alternative Pain Relief ← when painkillers aren’t helping, these things might!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Too Much Exercise Does To Your Body And Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Get more exercise” is a common rallying-cry for good health, but it is possible to overdo it. And, this is not just a matter of extreme cases of “exercise addiction”, but even going much above certain limits can already result in sabotaging one’s healthy gains. But how, and where does the line get drawn?
Too Much Of A Good Thing
The famous 150 minutes per week of moderate exercise (or 75 minutes of intense exercise) is an oft-touted figure. This video, on the other hand, springs for 5 hours of moderate exercise or 2.5 hours intense exercise as a good guideline.
We’re advised that going over those guidelines doesn’t necessarily increase health benefits, and on the contrary, may reduce or even reverse them. For example, we are told…
- Light to moderate running reduces the risk of death, but running intensely more than 3 times a week can negate these benefits.
- Extreme endurance exercises, like ultra-marathons, may cause heart damage, heart rhythm disorders, and artery enlargement.
- Women who exercise strenuously every day have a higher risk of heart attacks and strokes compared to those who exercise moderately.
- Excessive exercise in women can lead to the “female athlete triad” (loss of menstruation, osteoporosis, and eating disorders).
- In men, intense exercise can lower libido due to fatigue and reduced testosterone levels.
- Both men and women are at increased risk of overuse injuries (e.g., tendinitis, stress fractures) and impaired immunity from excessive exercise.
- There is a 72-hour window of impaired immunity after intense exercise, increasing the risk of infections.
Exercise addiction is rare, though, with this video citing “around 1 million people in the US suffer from exercise addiction”.
For more on finding the right balance, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: